Share information with your Facebook friends
VK
Colonoscopy during pregnancy is prescribed extremely rarely, if only for short periods and in case of severe bleeding or significant indications of a tumor process.
Preparation for colonoscopy during pregnancy and breastfeeding is limited. Of the available drugs to prepare for colonoscopy, Fortrans is used, but only for strict indications, since this drug does not have relevant studies on its effects on the fetus in the womb, but is approved for use during breastfeeding. It is also possible to use the drug Duphalac according to the original scheme given below, which has no corresponding contraindications.
What is colposcopy during pregnancy and how is it performed?
Colposcopy is a diagnostic method that involves examining the surface of the cervix under magnification. It is used in gynecology to identify a number of pathologies: dysplasia, leukoplakia (leucoplakia, Leukoplakia), cervical erosion, malignant and benign neoplasms, vascular pattern disorders, endometriosis (Endometriosis) of the vaginal cervix. In addition to disorders affecting the cervix, an indication for colposcopy during pregnancy may be a preventive assessment of the condition of the walls of the vagina and vulva.
There are two types of colposcopy performed during pregnancy:
- Survey (simple) colposcopy involves exclusively visual examination of the female genital organs without the use of chemical solutions and color filters.
- During extended colposcopy, the doctor applies special chemical reagents to certain areas of the mucosa to detect the presence or absence of altered cells. They are safe for mother and fetus. Typically, during extended colposcopy, a 3% acetic acid solution and an aqueous solution of potassium iodide (Schiller test) are used. When a weak solution of acetic acid is applied to the mucous membrane, a spasm of small blood vessels occurs, followed by expansion of the vascular network. Carrying out the Schiller test during colposcopy causes brown staining of the stratified squamous epithelium of the surface of the cervix and does not stain the altered mucosa. If, as a result of the use of reagents, any area of the cervix or vaginal walls raises doubts in the gynecologist, he scrapes this area for subsequent laboratory testing for oncocytology.
To conduct the examination, the doctor uses a special optical or video device - a colposcope. It is a device equipped with an illuminator and powerful lenses that allow you to obtain an image magnified by 3-40 times.
Expert opinion
Thanks to multiple magnification during colposcopy, the doctor is able to assess the color of the mucous membrane of the vagina and cervix, identify possible areas of damage, and apply special chemical solutions to the examined areas.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Colposcopy during pregnancy is performed in a gynecological chair. A plastic or metal speculum is inserted into the vagina to ensure optimal viewing. The optical head of the colposcope is placed at a distance of about 15-20 cm from the entrance to the vagina, and the resulting image is displayed on a computer monitor. The duration of the procedure depends on its type: a regular colposcopy takes about 10 minutes, and an extended examination takes about 20 minutes.
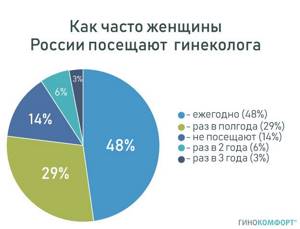
Visit to the gynecologist, statistics
The essence of colposcopy during pregnancy is practically no different from a similar study of non-pregnant women. The only difference is that the cervical canal during pregnancy is covered with a denser layer of mucus, which can impair visibility and complicate diagnosis. Therefore, colposcopy during pregnancy is usually performed by gynecologists-obstetricians who have experience in performing such manipulations on pregnant women.
It is also important to note that only a doctor can interpret the results of colposcopy.
Carrying out colonoscopy in pregnant women
Colonoscopy refers to endoscopic methods that can be used to examine the colon in the most informative way.
The need for surgery during pregnancy is not common, but may sometimes be necessary.
This article looks at how safe it is to have a colonoscopy during pregnancy (both for the mother and the fetus), and what the indications are.

- Correct assessment of possible risks and indications for diagnosis.
- Necessary preparation of the patient for endoscopy.
- Compliance with the examination method.
Computed tomography (CT) and contrast radiography to examine the bowel are highly discouraged during pregnancy due to radiation exposure during imaging and barium toxicity.
However, colonoscopy during pregnancy is also not a completely safe procedure. During the examination, it is necessary to administer anesthesia or even anesthesia, which can negatively affect the child.
You may be interested in: Placental polyp after a medical abortion: first symptoms and treatment without surgery
Tranquilizers, which put the patient to sleep during a diagnostic event, can cause oxygen deficiency (hypoxia) in the fetus and a decrease in blood pressure.
This is also caused by the long position of the woman on her back, which is necessary to insert the colonoscope.
In this case, the uterus is pressed by gravity against the back wall of the pelvis and compresses the blood vessels, especially the inferior vena cava, which supplies the abdominal organs and is involved in the blood supply to the developing baby.
In the early stages (first trimester), when important organs and systems begin to develop in the fetus, improper intervention can lead to internal bleeding or miscarriage.
Thus, the trial is postponed to the second trimester, when there is practically no risk to the child.
However, this does not apply to emergency colonoscopy, which is necessary in case of significant risk to the life and health of the mother.
In the last weeks of pregnancy, insertion of a colonoscope can trigger premature labor, so if possible, the procedure is postponed until the postpartum period.
Indications
The main diseases and clinical manifestations for which colonoscopy is performed in pregnant women:
- Symptoms of acute intestinal obstruction
- Heavy bleeding from the anus
- Damage to bile and pancreas
- Ischemic colitis
- Nausea and vomiting without weight loss after taking medications
- difficulty receiving
- suspected tumor or precancerous polyps in the colon
- inflammation of the gallbladder or pancreas (or a combination of both)
The best conditions for research are achieved with routine diagnosis, but indications requiring emergency colonoscopy are not excluded.
Contraindications

- Severe patient condition with respiratory or cardiovascular failure
- Intestinal fusion
- Diverticulitis
- Hemorrhagic shock, which occurs in case of massive blood loss
- Suspected peritonitis (requires urgent surgical intervention)
- Perforation (rupture) of the intestinal wall
- Hemorrhoids in the acute phase
- Infectious and sexually transmitted diseases
- anal fissure
- hemorrhagic vasculitis
- cerebrovascular accidents
Relative contraindications (when the issue of colonoscopy is decided individually with an assessment of the risks and benefits of the study) include
- IVF (especially in multiple pregnancies)
- Previous spontaneous abortions
- Septic ulcer complications
Pregnancy itself is not an absolute contraindication for colonoscopy. General preparation:
Preparing for the study
General preparation: General preparation:
- Correction of the patient’s general condition (normalization of blood pressure and water-electrolyte balance)
- Blood test for infections
- Assessment of the blood coagulation system (coagulogram) if necessary
A topical medication is used to cleanse the colon.

- Hard fruits
- Vegetables
- Flour
- Potato
To maintain hydration, you can drink water, tea or natural juices. Among food products, preference is given to low-fat broths, boiled eggs and fermented milk products.
A special feature of the drug during pregnancy is the inability to prescribe stimulants for intestinal peristalsis (since they cause uterine contractions).
Take 1 dose of Duphalac (diluted in a glass of water) the evening before the examination. It liquefies the intestinal contents and promotes the passage of stool. Also take Fortrans: dissolve 1-2 sachets in 1 liter of cold water (take 2/3 within one hour, the remaining third the next day).
Give a cleansing enema in the morning and use a gas line if necessary.
Choice of anesthesia
All medications are divided into groups depending on their effect on the mother and fetus. Unfortunately, in the absolutely safe category “A” there is only one drug - folic acid. All medications needed for sedation during a colonoscopy are classified as “B” or “D.”
The main drugs prescribed for anesthesia are benzodiazepines:
- diazepam - prohibited for use during pregnancy.
- Midazolam - should not be used during the 1st trimester (up to 13 weeks).
- Propofol belongs to category “B” and can be used under the supervision of an anesthesiologist.
The latter drug was tested on animals and did not have a toxic effect on the development of the embryo.
Nursing mothers should be aware that all benzodiazepines pass into breast milk. The day after the test, you should stop feeding and decant the first dose of liquid.
Colposcopy of the cervix during pregnancy: why is this procedure prescribed?
Colposcopy is included in the list of mandatory diagnostic measures that are carried out at the stage of pregnancy planning. If the patient has been identified with certain disorders affecting the vaginal mucosa, cervix and cervical canal, it is recommended to conduct the necessary studies and, if necessary, their treatment before conceiving a child. If the pregnancy was unplanned and no preliminary examinations were carried out, the doctor may prescribe a colposcopy for the expectant mother during pregnancy. What is it for?
Expert opinion
Colposcopy during pregnancy is performed solely for indications and not for prevention.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
While carrying a baby, a woman's hormonal background undergoes significant changes.
In some cases, this can lead to erosion or ectopia of the cervix. These concepts are not the same in meaning, although many women mistakenly confuse them.

Cervical erosion is a collective concept and implies any identified changes. Includes, for example, true erosion, caused by a defect in the cervical mucosa by trauma, inflammation, burn, etc. True erosion is a bright red, easily bleeding area on the cervical mucosa, the appearance of which is caused by desquamation of the stratified squamous epithelium. This condition must be treated, since when pathogenic microbes enter the affected area, inflammation can begin, which is dangerous for both the pregnant woman and the child. In addition, cervical erosion is more susceptible to stretching and tearing during childbirth. Ectopia is a normal variant and is a replacement of squamous stratified epithelium with columnar epithelial cells. However, in both cases (both with true erosion and with ectopia), there is a danger of transformation of healthy cells into atypical ones with the subsequent development of benign or malignant neoplasms.
This requires treatment and taking this disease into account during delivery. In addition to suspicion of the occurrence of erosion during pregnancy, colposcopy is done in case of fear of the development of an oncological process or a polyp of the cervical canal.
In addition, if a pregnant woman notices symptoms such as unusual vaginal discharge, vulvar rash, vaginal itching and burning, tenderness in the lower abdomen, pain during urination, or spotting after sex, she is also advised to undergo a colposcopy.
Indications for routine diagnostic colonoscopy are:
- The presence of pus, mucus and blood in the stool
- Chronic diarrhea and constipation
- Abdominal pain along the colon, bloating
- Low-grade fever (fever over a long period) of unknown etiology,
- Weight loss
- Anemia of unknown etiology
- Sensation of a foreign body in the rectum
- Benign and malignant neoplasms of the colon, diagnosed through other studies (irrigoscopy, CT, MRI)
- Search for the primary tumor when metastases are detected
- Assessing the effectiveness of conservative or surgical treatment
- Screening for colon cancer
Is it possible to have a colposcopy during pregnancy?
The answer to this question depends on the general health of the expectant mother, the nature of the course and duration of pregnancy. In any case, colposcopy should be carried out exclusively with the consent of the woman herself: the doctor can only advise whether or not to perform colposcopy, and the decision is made by the pregnant patient.
However, sometimes this diagnostic procedure is undesirable and there are certain contraindications. For example, colposcopy is not recommended if there is a threat of miscarriage in the early stages. This is due to the risk of bleeding and spontaneous abortion.
It is also undesirable to do colposcopy in case of placenta previa and the threat of premature birth.
A cervical biopsy during pregnancy is performed only if precancer or cervical cancer is suspected.
Preparing for colposcopy during pregnancy
To obtain accurate results, it is recommended to follow simple rules for preparing colposcopy during pregnancy:
- a couple of days before the diagnosis, it is recommended to avoid vaginal intimacy;
- It is undesirable to use vaginal suppositories, tablets, gels and foams;
- To wash before colposcopy, you do not need to use soap or washing gel - clean warm water is used instead;
- On the eve of colposcopy during pregnancy, vaginal douching is not recommended.
What to take with you? You don’t need to take anything special with you for the procedure; you should try to follow the above recommendations.
How is a colonoscopy done without anesthesia?
Refusal to use medicinal sleep does not affect the sequence of this medical procedure. The subject will first need to cleanse the intestines with an enema or laxatives. A few days before the examination, it is recommended to adhere to a diet, limit the consumption of coloring foods and certain medications (for example, activated carbon). There is no need to have breakfast on the day of the test. It is also worth removing contact lenses and dentures (if any).
Since colonoscopy is performed without anesthesia in a standard sequence, its main stages are:
- Take off your clothes and lie down on the couch (on your left side, pull your knees to your chest).
- Administration of local anesthetic (if desired).
- Lubricating the endoscope with a special oil that ensures better patency.
- Insertion of equipment that transmits images onto a monitor into the anus.
- Examination of anatomical structures, biopsy or endoscopic treatment.
- Removing the tube.
What sensations are normal during and after colposcopy during pregnancy?

During the examination, a pregnant woman may feel slight discomfort caused by the insertion of a speculum. The bursting feeling provoked by this manipulation is not dangerous, so the patient should simply relax and try not to pay attention to it.
If a biopsy is performed during colposcopy, the woman may feel a slight tingling sensation that goes away on its own within a few hours (less often, days) after the colposcopy. The same applies to testing with acetic acid: a slight burning sensation is a natural reaction of the mucous membrane in response to the application of the reagent during extended colposcopy. You can reduce these unpleasant sensations with the help of Gynocomfort restoring gel. The product copes well with vaginal discomfort caused by gynecological manipulations (including colposcopy). It contains active ingredients such as lactic acid, tea tree oil, chamomile extract, panthenol and bisabolol. Restoring gel "Ginocomfort" reduces vaginal discomfort, ensures rapid regeneration of the mucous membrane after diagnostic procedures, and helps maintain a normal level of vaginal acidity. The product underwent clinical trials at the Department of Dermatovenereology with the clinic of St. Petersburg State Medical University under the leadership of Sokolovsky E.V. and Ignatovsky A.V. and showed excellent results, the gel also has the necessary documents and quality certificates.
What can be the consequences of colposcopy? If, after a colposcopy, a pregnant woman discovers slight spotting from the vagina, this is not a reason to panic. In most cases, they are caused by a reaction of the mucous membrane to chemical reagents.
Expert opinion
Sometimes (especially if a biopsy was performed during colposcopy) a small amount of blood may be present in the discharge. The only cause for concern can be heavy discharge accompanied by pain - in this case, you should urgently consult a doctor.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Contraindications to the procedure:
- acute myocardial infarction and decompensated cardiopulmonary failure
- stroke
- fulminant form of colitis
- acute infectious process of any localization
- acute diverticulitis
- aortic aneurysm
- tense ascites
85% of patients with colon cancer are over 60 years of age. According to the recommendation of the World Health Organization, a colonoscopy should be performed for every healthy person after 55 years of age once every 10 years. If there is an increased risk of the disease in the family (in first-degree relatives, especially if colon cancer developed in the patient before 45 years of age), the first preventive colonoscopy should be performed 10 years before the age at which cancer was detected in relatives. If certain complaints or indications appear, a colonoscopy should be performed immediately.
Preparing for a colonoscopy:
Colposcopy: examination of the cervix, video
is not responsible for the accuracy of the information presented in this video clip.
Source – Oasis of Health Sources:
- COLPOSCOPIC CHANGES IN THE CERVIX DURING PREGNANCY. Kogan Ya.E., Gafarova A.A. // Practical medicine. – 2021. – No. 7 (108). – pp. 18-21.
- METHODS FOR STUDYING THE CERVIX IN PREGNANT WOMEN. Sidorova I.S. Atabieva D.A. // Obstetrics, gynecology and reproduction. – 2013. – No. 2. – 15-19.
- ALGORITHM FOR MANAGEMENT OF PREGNANT WOMEN WITH CERVICAL PATHOLOGY. Yusupoka M. A., Ismailova D. U., Matmuratova S. O. // Interactive science. – 2017. – No. 2 (12). – pp. 84-88.
- Pregnancy: cervical difficulties. Cervix of the uterus in pregnant women: normal picture and disease. N.V. Zarochentseva // Gynecology, obstetrics, infertile marriage. - 2014. - T. 18.
- Diseases of the cervix and modern methods of their diagnosis (literature review). HELL. Atabieva, T.V. Pikuza, R.A. Chilova, E.V. Zhukova, N.S. Trifonova // Bulletin of modern clinical medicine. — 2021. — Volume 9. — Issue. 4.
- Pregnancy and cervical diseases: frequency, gestational complications, maternal and perinatal outcomes. Kolomoets E.V. // Author's abstract. dis. Ph.D. honey. Sciences E.V. Kolomoets. - Moscow. - 2012. - P. 25.
- https://www.tosnocrb.ru/novosti/kolposkopiya/
- https://infobaby.org/colposcopy-during-pregnancy/
- https://www.pubfacts.com/detail/19550217/The-management-of-cervical-intraepithelial-neoplasia-during…
- https://www.longdom.org/open-access/diagnostic-and-therapeutic-endoscopy-in-pregnancy-when-why-and-h…
- https://www.ncbi.nlm.nih.gov/pubmed/30118992
Popular questions
The first pregnancy had placental abruption at 12 weeks.
I spent a week in the hospital. All that remained was yellow discharge. In the evening after discharge, the discharge changed to brown, to dark blood. This is fine? There should be no bleeding during pregnancy. This indicates a threat of interruption and requires treatment in a specialized department.
We are planning a pregnancy. According to my last ultrasound on the 18th day of the cycle, I had an M-echo of 0.6 cm and a cyst in the right ovary 3.3 * 2.4. in the left there are 16 follicles, with a diameter from 0.4 to 0.6. 1. Can I get pregnant in the next cycle with a cyst and is it dangerous? 2. How by day of the cycle and in what dosage can you take vitamins for follicle growth and endometrial growth (folic acid, vitamin E, vitamin C, group B, etc. are of interest)
First of all, it is necessary to find out the nature of the ovarian cyst and the reason for the multifollicularity of the second ovary. I will also note that the M-echo for this day of the cycle does not correspond to the norm. I recommend that you see an obstetrician-gynecologist during this cycle. Conduct a test for STIs, since most often it is this factor that leads to such changes. Perform an ultrasound on days 5-7 of the cycle to monitor the condition of the ovarian cyst. And only then discuss the feasibility of vitamin therapy according to the phases of the menstrual cycle.
Good afternoon At the appointment, the gynecologist, before examining with a speculum, irrigated the vagina with a solution of hydrogen peroxide. I'm 20 weeks pregnant and have some erosion. Will this harm the baby?
Hello! This antiseptic will not harm the baby; it acts locally, only on the mucous membranes where it is applied.
Hello! At 31 weeks and 4 days of pregnancy, they diagnosed stage 2 placenta maturity, is this dangerous? My doctor doesn’t say anything or prescribe anything, maybe I should go to another doctor?
Hello!
According to ultrasound, not only the degree of maturation of the placenta is important, but also hemodynamic indicators in the feto-placental complex, the amount and nature of amniotic fluid, and the condition of the fetus. In such cases, fetal hypoxia and microcirculation disorders are prevented. You can consult and carry out preventive treatment in a maternity hospital. For an accurate diagnosis, contact a specialist