Author
Egamberdiev Shavkat Makhmudovich
Doctor
Endoscopist
until September 30
We're giving away RUR 1,000 for all services per visit in September More details All promotions
Colonoscopy
(
fibrocolonoscopy
) is an endoscopic examination of the lower intestine. Unlike retroromanoscopy, colonoscopy allows you to get an idea of the condition of not only the rectum, but also the colon.
Colonoscopy is performed using a colonoscope, a special device that is a flexible tube equipped with a lighting system. An optical fiber runs inside the tube, allowing the doctor to see the actual condition of the intestines. The colonoscope is also equipped with a device for taking a biopsy (biological material), which can be used to perform minor surgical interventions.
Indications for colonoscopy
Colonoscopy may be prescribed for the following complaints (symptoms):
- pain and cramps in the abdomen;
- bowel dysfunction (chronic constipation or diarrhea);
- flatulence: feeling of heaviness in the stomach, bloating;
- belching, feeling of nausea after eating;
- decreased appetite.
Recovery after colonoscopy
Side effects of the procedure are discomfort as a result of the injection of air into the intestines during the examination, pain due to involuntary contractions of smooth muscles as the probe passes further than 15 centimeters. Proper rehabilitation will help the patient overcome all this - daily routine, dietary nutrition, medications that eliminate discomfort in the stomach and intestines.
The menu during this period is formed taking into account possible injury to the intestinal walls, especially if the examination was accompanied by the removal of tumors or the collection of biomaterial. Basic nutrition rules:
Among the permitted products: lean meats and fish, heat-treated vegetables, light broths, dairy products (low-fat cottage cheese, yogurt, kefir), lightly dried whole grain bread, eggs in the form of a steam omelet, savory cookies, fruit drinks, compotes, jelly. Method of preparation: boiling or stewing. It is advisable not to consume fresh fruits on the first day after a colonoscopy. It is forbidden to drink strong tea or coffee, carbonated drinks, alcohol, or freshly squeezed juices. Long-term dietary restrictions after colonoscopy are not required. 2-3 days are enough.
To reduce intestinal colic after the study, on the recommendation of a doctor, you can take sorbents and antispasmodics. To eliminate pain in the anus, it is advisable to use rectal suppositories or ointments that are used for hemorrhoids. If abdominal discomfort, diarrhea or constipation, bleeding from the anus and other disorders continue for more than 2-3 days, you should definitely consult a specialist! It is necessary to carefully monitor the condition of your body.
Colonoscopy
- a modern diagnostic method that will not only establish, but also eliminate the cause of pathological symptoms of the digestive tract. If you are regularly bothered by intestinal problems, do not delay visiting your doctor. Don't self-medicate!
Sign up for a colonoscopy procedure
Make an appointment
How is a colonoscopy performed?
Colonoscopy is performed through the anus. The procedure is inevitably associated with some discomfort and pain. Understanding this, the doctor acts carefully and carefully, trying to reduce possible unpleasant and painful sensations to a minimum.
To carry out the procedure, you will need to undress from the waist down, lie on a couch or examination table on your left side, pulling your knees to your chest.
The colonoscope is inserted into the lumen of the rectum and gradually moves along the intestine. The study takes from 20 to 60 minutes. More time is required if manipulations are performed (taking a biopsy, removing a polyp).
In what cases is colonoscopy indicated or contraindicated for you?
Colonoscopy is a serious endoscopic examination of the colon to diagnose its pathologies or disorders in its functioning. A diagnostic procedure is performed using a special device - a colonoscope, which allows you to examine the large intestine along almost its entire length. During a colonoscopy, it is possible to quickly perform some therapeutic procedures: removing a foreign body that has entered the colon, stopping bleeding, excision of a polyp, etc.
Colonoscopy in a dream
For patients who want to completely eliminate discomfort during colonoscopy, the option of performing the study in a state of medicated sleep is offered.
Colonoscopy in a dream is carried out in the hospitals of JSC "Family Doctor". To put you to sleep, the drug “Proviv” is used. Drug-induced sleep should be distinguished from general anesthesia. Before the drug is administered, you must be examined by an anesthesiologist, so you must come to the study in advance - 30 minutes before the time for which the colonoscopy is scheduled. In this case, you must have a transcript of a fresh electrocardiogram on hand.
The patient falls asleep as soon as the administration of the drug begins, and wakes up almost as soon as the administration ends. Full recovery occurs in 15-20 minutes, but it is recommended to stay in the hospital for 1-3 hours under medical supervision. It is recommended to drive no earlier than 2 hours after the procedure.
What can be revealed
FCS with anesthesia allows you to:
- carry out differential diagnosis between chronic diseases with colitis syndrome;
- identify diverticula;
- detect polyps and other benign neoplasms and remove them endoscopically;
- detect malignant tumors (cancer) of any form at the earliest stages, when they are still small in size and limited to the mucous membrane and submucosal layer.
At the moment, FCS is the most informative, reliable and safe way to assess the condition of the wall of the large intestine and identify any neoplasms located here.
How to prepare for a colonoscopy?
Colonoscopy will be effective only if the patient has taken a responsible approach to preparing for the study and followed all the necessary recommendations.
First of all, 3 days before the procedure you should switch to a slag-free diet. The following should be excluded: brown bread, cereals, fresh vegetables and fruits, greens, cabbage in any form, legumes, peas, lentils, dried fruits, including raisins, berries and nuts, fatty dairy products (including cream, sour cream, ice cream , fatty cottage cheese), fatty fish and meats (including duck and goose), pickles, marinades, smoked foods, sweets, alcohol, carbonated drinks, kvass.
Allowed to eat: rice, pasta made from premium flour, white bread, boiled lean meat (veal, beef, chicken), cutlets, meatballs or soufflé, eggs, lean fish (cod, pike perch, perch, pike) , vegetable decoctions, potatoes (without peel), low-fat dairy products (cottage cheese, cheese, kefir, skim milk), honey.
If you suffer from constipation, be sure to take laxatives daily, perhaps slightly increasing their dose compared to the usual one (without violating the instructions for use).
On the eve of a colonoscopy, it is necessary to cleanse the intestines. Doctors at Family Doctor recommend using Fortrans or Fleet phospho-soda for this purpose. Taking medications will save you from having to do an enema.
NOTE!
The drug of choice for preparation for colonoscopy is FORTRANS if:
- the patient is taking drugs from the group of angiotensin-converting enzyme inhibitors (Ace Inhibitor, Akf-Inhibitor), such as Convertin, Captopril, Capoten;
- drugs of the angiotensin receptor blocker group, such as Atacand, Oksaar;
- there is renal failure;
- heart failure;
- have diabetes mellitus;
- symptoms that suggest nonspecific diseases of the large intestine (Crohn's disease, UC).
Preparation for colonoscopy using the drug "Fortrans"
A packet of Fortrans is diluted in 1 liter of water (clear juice or weak tea can be used). The more acidic the liquid, the easier it will be to drink the solution.
You should start drinking the solution on the day before the colonoscopy, no earlier than two hours after lunch. Lunch should be light (broth, tea). The Fortrans package contains 4 sachets. It is advisable to use all four (for persons whose weight is more than 50 kg). You need to drink a glass of the solution every 15-20 minutes for 4-5 hours. The optimal time to take Fortrans is from 9 a.m. to 11 p.m. You can wash down the solution with a small amount of sour juice (without pulp) or eat it with a slice of lemon. Loose stools will appear 1-2 hours after starting to take the drug, and 2-3 hours after taking the last dose, the intestines will be completely cleansed.
After which you cannot eat anything until the colonoscopy.
Section 2. Criteria for quality colonoscopy
In countries where national colorectal cancer screening programs are organized, special recommendations are created aimed at reducing the risk of complications during examinations, standards and indicators (indicators) of the quality of colonoscopy are determined. Proficiency in colonoscopy techniques is not sufficient to perform high-quality colonoscopy; compliance with target colonoscopy quality indicators is important. The main value of colonoscopy as a screening method depends on the quality of the examination of the colon mucosa, and the results are a decisive factor in determining the interval of subsequent colonoscopies.
The European Society of Gastrointestinal Endoscopy (ESGE) and the United European Gastroenterology have identified endoscopic quality as a top priority. Because of the wide variation among endoscopists in the quality of colonoscopy they perform and the implementation of national CRC screening programs, quality in colonoscopy has been identified as a priority by the ESGE Working Group. The goal of the ESGE working group is to identify key performance indicators for colonoscopy. Key performance indicators for colonoscopy had to meet the following requirements: proven impact on clinical outcomes or quality of life, simplicity of methods and methods of measurement, susceptibility to improvement, and ability to be used at all levels of the endoscopy service.
In 2012 and 2021, ESGE presented a list of key performance indicators for colonoscopy [10, 11]:
1) level of adequate preparation of the colon;
2) cecal intubation rate;
3) adenoma detection rate (ADR);
4) use of appropriate polypectomy technique;
5) level of development of complications;
6) patient tolerance to colonoscopy;
7) compliance with appropriate observation intervals after polypectomy.
According to the recommendations of the American Society of Gastrointestinal Endoscopy (ASGE), all indicators of the quality of colonoscopy are divided into three stages relative to the study [12]: the first stage - before the colonoscopy, the second stage - during the colonoscopy, the third stage - after the colonoscopy .
Indicators of the quality of colonoscopy at the stage preceding the examination:
1. Compliance with recommendations for prescribing colonoscopy. Colonoscopy should be justifiably prescribed for appropriate indications. Target: ≥80%.
2. Informed voluntary consent. Patients or their representatives must sign an informed consent form. All risks associated with colonoscopy, possible complications, benefits and alternative methods should be clearly explained before the colonoscopy is performed. Target: ≥90%.
3. Compliance with the recommended time intervals when performing subsequent colonoscopies. Intervals for subsequent colonoscopies should be observed based on the results of the examination (no pathology detected, polyps or cancer). Target: ≥90%.
4. Compliance with intervals between subsequent colonoscopies carried out for the purpose of observation in inflammatory bowel diseases: Crohn's disease and ulcerative colitis. ASGE recommends colonoscopies 1 to 2 times per year for the first 8 to 10 years after diagnosis due to the increased risk of developing colorectal cancer. Target: ≥90%.
Colonoscopy quality indicators at the stage of endoscopic examination of the colon should take into account the following indicators:
1. Quality of colon preparation. The endoscopist should document the quality of colon preparation in the colonoscopy report. Various rating scales are used to assess the level of colon cleansing. But you can also use the terms “adequate” and “inadequate” to characterize preparation for a colonoscopy. The quality of colon preparation directly affects the interval before subsequent colonoscopy. Repeat colonoscopy for “inadequate” colon preparation should be repeated within 1 year. Target: ≥98%. The number of patients recommended to repeat colonoscopy within 1 year should not exceed 15%. Target for adequate colon preparation: 85%.
2. Intubation of the cecum with photo documentation. During colonoscopy, it is mandatory to extend the colonoscope to the dome of the cecum (Cecal Intubation Rate - CIR) with clear identification and photographs of the main anatomical landmarks of the cecum. Target rate for screening colonoscopies: >95%.
3. The rate of adenomas detected in patients during screening colonoscopy should exceed 20%.
4. Colonoscopy Withdrawal Time (CWT) should be measured. Target: >98%. During screening colonoscopy without detecting pathology, the removal time of the colonoscope should exceed 6 minutes.
5. Compliance with recommendations for polypectomy. Pedicled and wide-based polyps up to 2 cm in size should be removed using endoscopic resection of the colon mucosa with a polyp. Only if endoscopic resection is not possible should these patients be referred for surgical treatment.
Colonoscopy quality indicators that are considered during the post-colonoscopy phase include the following:
1. Complications. The frequency of perforations after colonoscopy should not exceed 1 in 500 examinations, and in the case of screening colonoscopies - 1 in 1000 examinations. The bleeding rate after polypectomy should be <1%, taking into account both acute and delayed bleeding.
2. Compliance with recommendations for scheduling subsequent colonoscopies. Intervals for subsequent colonoscopies are determined after the results of histological examination and must be recorded in the medical records.
The European and American Societies of Gastrointestinal Endoscopy ( ESGE
and ASGE ) of all the above indicators of the quality of colonoscopy identify priority ones that are most important when assessing the organization of screening colonoscopy and assessing the professional training of the endoscopist.
These include the quality of bowel preparation for examination, the rate of detection of adenomas, the rate of intubation of the cecum, the time of examination of the bowel when removing the endoscope from the cecum to the rectum.
1. Quality of colon preparation for examination: in at least 90% of screening studies, the quality of colon cleansing should be assessed as adequate or better, preferably 95%.
2. Rate of reaching the cecal dome: minimum cecal intubation rate of 90%, preferably 95%, photographic image of the cecal dome.
3. Adenoma detection rate: the minimum detection rate of adenomas during screening or diagnostic colonoscopies in people over 50 years of age is ≥25%.
4. Colonoscope withdrawal/withdrawal time (exit inspection time): minimum time 6 minutes for diagnostic studies, preferably 10 minutes.
5. Description of the morphology of non-polypoid formations: according to the Paris classification.
1. Quality of colon preparation for examination: in at least 90% of screening studies, the quality of colon cleansing should be assessed as adequate or better, preferably 95%.
According to ESGE recommendations [10], the level of colon cleansing before colonoscopy should be assessed and should be adequate (good and excellent bowel preparation as measured by the grading scale) in at least 90% of screening colonoscopies performed (Fig. 1).

Rice. 1. High-quality preparation (a) and insufficient preparation (b) of the intestines before colonoscopy. The photo shows a perfectly clean intestinal lumen during preparation with a two-stage regimen of MOVIPREP® in combination with simethicone. Several scales have been published to assess the level of colon cleansing. The most commonly used are the Ottawa Bowel Preparation Scale (Fig. 2)
Rice. 2. Ottawa scale. Explanations and translation into Russian of the abbreviations in the figure. OBPS - Ottawa Bowel Preparation Scale - scale for assessing the level of colon cleansing Ottawa, excellent - excellent, good - good, fair - sufficient, poor - bad, inadequate - inadequate, LC (left colon) - left sections of the intestine, TC (transverse colon ) - transverse sections of the intestine, RC (right colon) - right sections of the intestine. and Boston (Boston Bowel Preparation Scale) (Fig. 3)
3. Boston scale. Explanations and translation into Russian of the abbreviations in the figure. BBPS (Boston Bowel Preparation Scale) - scale for assessing the level of colon cleansing Boston, excellent - excellent, good - good, poor - bad, inadequate - inadequate, LC (left colon) - left parts of the intestine, TC (transverse colon) - transverse sections of the intestine, RC (right colon) - right sections of the intestine. [30-32]. In the Ottawa scale, the overall assessment of the level of preparation of the colon consists of two assessments. The first assessment includes the possibility of examining the mucous membrane and additional steps taken to clean the colon of residual feces and fluid (washing and removing the contents using suction). The level of preparation of the colon is assessed in three different segments: in the right flank, in the transverse colon and in the left flank, and then by adding the three numbers, an overall assessment of the level of preparation of the colon as a whole is obtained. The second assessment is the amount of residual fluid remaining in the entire colon after preparation. The Ottawa scale is overly sensitive to the actions required to remove residual stool and fluid. As a result, the final score does not always truly reflect the visualization of the mucosa. The Boston scale also evaluates the level of preparation of the colon in three different segments: in the right flank, in the transverse colon and in the left flank, and then add the three numbers and get an overall assessment of the level of preparation of the colon as a whole. This scale does not take into account the amount of residual fluid in the entire colon and does not separately separate the washing or removal by suction of residual colon contents. Ottawa scale.
Score the ability to examine the mucous membrane from 0 to 4 in each segment:
— Excellent (0) — the colon mucosa is well visualized. Minimum amount of residual liquid.
— Good (1) — good visualization of the mucous membrane. Minimal amount of cloudy liquid.
— Sufficient (2) — it is necessary to remove residual fluid with bubbles and liquid feces using suction. Acceptable visualization of the mucosa.
— Bad (3) — there is semi-solid feces in the intestinal lumen. The colon contents must be washed and suctioned to obtain acceptable visualization of the mucosa.
— Inadequate (4) — in the intestinal lumen there are semi-solid and hard feces that impede inspection. It is not possible to wash the intestinal contents and remove them using suction.
Amount of fluid in the entire intestine, from 0 to 2:
— Low — 0
— Average — 1
— Big — 2
Boston scale.
A quantitative 4-point training assessment system is carried out in three segments: the right parts of the colon (cecum and ascending colon), the middle parts (transverse colon, including the hepatic and splenic flexures) and the left parts (descending and sigmoid colon, rectum ).
Each of the three departments is given a score from 0 to 3 points:
— Excellent (3) — excellent visualization of the mucous membrane without the presence of residual fluid in the intestine.
- Good (2) - a small amount of cloudy liquid mixed with liquid feces. Good visualization of the mucous membrane.
— Bad (1) — there are liquid and solid feces in the intestine.
— Inadequate (0) — hard stool in the intestine, the mucous membrane is not visualized.
The total number of points is summed up, and the maximum number corresponding to the ideal quality of preparation is 9. Training with a total score of 6 and/or is considered adequate if the total score for each segment is >2.
To apply this scale in your practice, it is recommended that you first undergo independent training using the training program: www: cori.org/bbps/.
An example of a description in the study protocol is excellent, 9 points (3, 3 and 3 for Quality of preparation: for each segment) on the Boston scale.
Assessment of the possibility of examining the mucous membrane from 0 to 3 points in each segment:
— excellent (3 points) — excellent visualization of the mucous membrane without the presence of residual fluid in the intestine;
— good (2 points) — a small amount of cloudy colored liquid mixed with liquid intestinal contents, but the visualization of the mucous membrane is good;
— bad (1 point) — there are liquid and solid feces in the intestine, only part of the mucous membrane is visible;
- inadequate (0 points) - there is solid (dense) intestinal contents in the intestine, the mucous membrane is not visualized due to the impossibility of washing it from dense intestinal contents, this section is not prepared for research.
Regardless of the scale used to assess the level of colon cleansing, the endoscopist should document the quality of colon preparation based on the ability to identify polyps after residual fluid and intestinal contents have been removed, if possible [12]. This quality indicator is one of the most important for the colonoscopy physician and the patient, who needs to conduct the examination in such a way as not to miss early forms of cancer and other minute structural changes in the intestinal mucosa. Effective colon cleansing is fundamental to performing a high-quality colonoscopy.
adequate
and inadequate preparation
to characterize the level of preparation of the colon before colonoscopy . With adequate preparation of the colon, polyps measuring >5 mm can be detected [33]. In case of inadequate colon preparation, it is recommended to perform a repeat colonoscopy within 1 year [12]. Adequate colonic preparation optimizes cecal intubation rates, whereas poor preparation is associated with prolonged colonoscopy time and decreased adenoma detection rates [34, 35].
When choosing a drug and a regimen for taking a laxative, it is necessary to carefully evaluate such points as the presence of hepatic, renal, or heart failure in the patient and the possible use of diuretics at the moment. Preparations based on soda phosphate may be better tolerated by the patient due to the smaller volume of solution, but they are not safe, especially when used in elderly patients with renal failure [36]. Tolerance of a large volume (4 L) of polyethylene glycol solution, especially in elderly patients, may be poor. The tolerability of a large volume of laxative drug is improved by dividing the dose (split-dose) into two stages, i.e., half the dose of the laxative drug is taken the evening before the test, and the second half - in the morning on the day of the study, which also improves the quality of preparation of the colon.
Alessandro Repici (Milan, Italy) et al. conducted a study that assessed the effectiveness and overall acceptability of different laxative drugs used to prepare the colon before colonoscopy. In the study, 57.3% of patients used 4 L of PEG (polyethylene glycol), 29.5% of patients used 2 L of PEG, and 13.2% of patients used 2 cups of a laxative solution containing sodium phosphate/magnesium citrate/sodium picosulfate. Overall acceptability was higher in the groups using 2 L PEG and 2 glasses of laxative solution. Colon cleansing was good in the 2 and 4 L PEG groups, and the level of colon cleansing in these groups was significantly better than in the group of patients using 2 glasses of laxative solution (sodium phosphate/magnesium citrate/sodium picosulfate). In summary, the study found that 2 and 4 L of PEG provided more effective colon cleansing prior to colonoscopy. But due to the 2 times smaller volume of laxative solution in the group of patients using 2 l of PEG, the acceptability of the preparation was significantly higher [37].
Another important factor that improves the quality of colon preparation is the time interval between the end of taking a laxative and the start of a colonoscopy. Studies have shown that the quality of preparation deteriorates if this interval increases, especially for the right flanks of the colon [38]. Endoscopists who have >15% of examinations with inadequate preparation should review their colon preparation protocols, including more detailed patient education on all the rules for safe and effective bowel preparation for colonoscopy, selection of the most effective and safe laxative drug, and choice of laxative drug regimen.
2. Rate of reaching the cecal dome: minimum cecal intubation rate of 90%, preferably 95%, photographic image of the cecal dome.
The Cecal Intubation Rate (CIR) is defined as the number of colonoscopies in which the endoscope was inserted into the dome of the cecum and required photographic documentation of major cecal landmarks. According to ESGE recommendations [10], the cecal intubation rate should be at least 90% and confirmed by photographs of the appendix orifice and ileocecal valve. This number excludes cases of obstructive cancer requiring surgical treatment. A complete examination of the colon is the basis of a screening colonoscopy. The medial wall of the cecum between the mouth of the appendix and the ileocecal valve is not visualized at a distance. Cecal intubation involves inserting an endoscope into the cecum and touching the endoscope tip to the mouth of the appendix. ESGE recommends that the cecal intubation rate be calculated. A low value of this indicator is associated with a high rate of interval proximal colon cancer [20]. Quick and accurate insertion of the endoscope into the cecum is an indirect sign of the skill of the endoscopist. However, there are a number of factors that influence the successful insertion of a colonoscope into the cecum. As the patient's age and body mass index increase, the chances of successfully inserting an endoscope into the cecum decrease [21, 22]. The use of an endoscope with variable stiffness increases the chances of successful insertion of the colonoscope into the cecum [23]. Cecal intubation should always be supported by photographic documentation of major cecal landmarks. The first photograph, the orifice of the appendix, should be taken at a distance of 2 to 4 cm and include the cecal fold. The second photograph, the entrance to the cecum, should cover the entire cecum and the ileocecal valve. If the study is terminated for a number of reasons, photographs of the conditions for which the study was terminated must be provided [12]. No allowance is made for cases with poor colonic preparation, i.e. they are included in the calculation of the cecal intubation rate. This fact makes it possible to identify endoscopy departments where the level of colon cleansing is assessed as suboptimal, and to analyze the preparation of the colon in order to improve the level of cleansing before colonoscopy [10].
3. Adenoma detection rate: the minimum detection rate of adenomas during screening or diagnostic colonoscopies in people over 50 years of age is ≥25%.
The rate of detected adenomas and the rate of detected colon polyps (Polyp Detection Rate - PDR).
The adenoma detection rate
is the ratio of the number of colonoscopies in which one or more histologically confirmed adenomas were identified to the total number of colonoscopies performed [10].
The polyp detection rate
is the ratio of the number of colonoscopies in which one or more polyps were detected to the total number of colonoscopies performed. The value of the rate of detected adenomas with proper organization of screening colonoscopy should be at least 15% when examining women, and at least 25% for men, and on average exceed 20% [13]. Detection of adenomas and early cancer is the basis of colonoscopy, which is performed to screen for colorectal polyps and cancer. Data from the UK and US CRC screening studies suggest that removal of colon adenomas reduces the risk of subsequent development of colon cancer [14].
The rate of detected adenomas correlates with the rate of missed CRC. A study by M. Kaminski et al. [15] revealed a strong association between the rate of detected adenomas and the risk of developing interval cancer ( p
=0.008). Interval cancer was defined as colorectal adenocarcinoma detected between the screening colonoscopy and the subsequent post-screening colonoscopy. The study analyzed data obtained on the detection rate of adenomas during screening colonoscopies and data on interval cancers from the CRC incidence registry. The study showed that adenoma detection rates below 20% were significantly associated with an increased risk of interval CRC compared with adenoma detection rates of 20% and above [15].
In 2014, a study by D. Corley et al. [16] showed that a 1% increase in the detection rate of adenomas reduced the incidence of CRC by 3% and reduced the mortality from CRC by 5%. A high rate of adenoma detection was associated with a reduced risk of developing both proximal and distal colorectal cancer to the same extent for men and women.
A number of studies [17] demonstrate a good correlation between the rate of detected adenomas and the rate of detected colon polyps. However, the adenoma detection rate is more appropriate for assessing the quality of colonoscopy because the polyp detection rate includes the number of all polyps detected at colonoscopy—both the number of adenomas and the number of hyperplastic polyps.
Recently, the question has been increasingly asked: is the rate of detected adenomas the optimal indicator of the quality of examination of the colon mucosa? The literature presents a number of problems associated with the rate of identified adenomas. First, this indicator requires manual entry and additional work from endoscopists. Secondly, the doctor’s resistance to gaming behavior is necessary, when the endoscopist’s actions are aimed at achieving the goal, but do not lead to optimization of the detection of precancerous changes. This phenomenon is called “one and done,” when a doctor, during a colonoscopy, finds one formation with endoscopic signs of an adenoma and stops carefully examining the remaining areas of the colon mucosa [12]. Perhaps a more optimal indicator of the quality of examination of the colon mucosa may be the Adenoma Detection Index (ADI). The adenoma detection index is defined as the total number of adenomas detected divided by the total number of colonoscopies performed [10]. It reflects the quality of examination of the mucous membrane along the entire length of the colon and, more accurately than the rate of detection of adenomas, captures the difference between the performance of endoscopists in relation to the quality of examination of the mucous membrane [18]. Using the adenoma detection index helps overcome the “one and done” problem. Currently, this indicator is used mainly in clinical studies [19]. In many countries with national CRC screening programs, adenoma detection rates are the most important indicator of the quality of screening colonoscopy.
4. Colonoscope withdrawal/withdrawal time (exit inspection time): minimum time 6 minutes for diagnostic studies, preferably 10 minutes. The time for withdrawing the endoscope from the dome of the cecum to the anal canal (Colonoscopy Withdrawal Time - CWT) should be sufficient for a detailed examination of all parts of the colon in order to visualize polyps and colorectal cancer. According to ESGE guidelines [10], colonoscope withdrawal time (CWT) should be measured and be ≥6 min in at least 90% of cases.
The CWT indicator is directly related to the detection rates of polyps and adenomas. The detection rate of adenomas decreases when the time of removal of the colonoscope from the dome of the cecum is less than 6 minutes. In 2006, R. Barclay et al. [24] were among the first to report that endoscopists whose colonoscope withdrawal time (CWT) from the cecum to the anal canal was 6 min or more detected more colorectal neoplasia than those whose colonoscope withdrawal time was <6 min ( 28.3 and 11.8%, respectively; p
<0,001).
In a study by T. Lee et al. [25] in 2011, an analysis of adenoma detection rates depending on CWT was performed. Four groups of adenoma detection rates depending on CWT were considered. The results of the study are presented in table. 1.
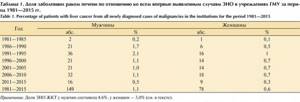
Table 1. Adenoma detection rate (ADR) in groups depending on the time of removal of the colonoscope from the cecum to the anal canal (CWT)
The study showed that as CWT increases to 10 minutes, the detection rate of adenomas also increases. Its increase occurs due to the detection of a greater number of neoplasias less than 1 cm in size, as well as due to the detection of neoplasia in the right parts of the colon. With a further increase in CWT (≥11 min), no increase in the detection rate of adenomas was observed. In summary, this study shows that the optimal colonoscope withdrawal time for screening colonoscopy is 10 minutes. A minimum of 6 minutes is recommended for cases without biopsy and polypectomy. The removal rate of the colonoscope is not the only factor influencing the detection rate of polyps and adenomas. Factors that increase the detection rate of polyps and adenomas include aspiration of intraluminal fluid, careful examination of the haustra [26], changing the patient’s position, using buscopan, using a distal soft cap [27], using chromoscopy [28], and using all available technologies for examining “blind” patients. » zones in the colon behind the haustra [29].
5. Description of the morphology of non-polypoid formations: according to the Paris classification
. Information is presented in the section “Section 7. Standards for completing a colonoscopy protocol.”