Causes Diagnosis Treatment
Leukospermia. The patient can receive such a conclusion after taking a spermogram. Leukospermia (pyospermia or leukocytospermia) is an increased number of leukocytes in the ejaculate. According to the latest WHO standards, leukospermia is defined when there are more than 1 million leukocytes per 1 ml of semen.
Leukocytes are white blood cells. Their main purpose is to protect the body from infections and help the body overcome them.
Treatment regimen for leukospermia
Consultation with an andrologist based on spermogram results Treatment of leukospermia in men
Price 4000 rub.
Address: Moscow, Begovaya st., 7, Begovaya metro station
Make an appointment by phone: +7 495 199-7554
+ MAKE AN APPOINTMENT
Leukocytes (white blood cells)
are markers of inflammation.
However, in addition to the fact that an increase in the number of leukocytes in sperm indicates an inflammatory process in the male genitourinary system, they directly affect the quality of sperm
. Leukocytes produce free radicals (reactive oxygen species), an imbalance with antioxidants or oxidative stress of sperm occurs. Free radicals attack and destroy infections, and at the same time destroy the sperm membrane and damage the DNA molecule in the head.
With leukospermia, a decrease in sperm motility and an increase in the DNA fragmentation index are also observed.
All this affects a man's fertility: slow sperm cannot reach the egg and fertilize it, and fertilization with sperm with damaged DNA increases the risk of miscarriage and delayed fetal development (Source)
Reasons for the development of leukospermia
An increase in the number of leukocytes indicates inflammation in the organs of the male genitourinary system (testes, vas deferens). The causes of inflammation may be:
- Infections
- Autoimmune diseases and reactions
- Urethral stricture
- Varicocele
- Systemic disease (affecting the entire body)
- Long-term abstinence
- Prostatitis
- Smoking tobacco and soft drugs, drinking alcohol
Most often, the cause is genitourinary tract infections: mycoplasma, ureaplasma and chlamydia. 10% of patients suffering from these infections do not notice any symptoms, which means they are not cured.
If the infection is confirmed, your partner should also get tested. And for the duration of treatment, suspend sexual activity.
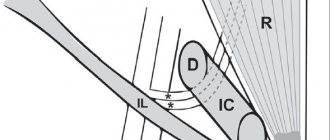
Pathogenic bacteria can end up in any part of the genitourinary tract, causing swelling and inflammation. Depending on their location this will result in:
- Epididymitis (inflammation of the epididymis)
- Orchitis (testicular inflammation)
- Orchiepididymitis (inflammation of the testicle and epididymis at the same time)
- Cystitis (inflammation of the bladder)
- Urethritis (inflammation of the urethra)
Symptoms
of inflammation can be: discomfort and pain in the scrotum and perineum, pain and burning when urinating, a strong smell of urine, discharge from the urethra (transparent from white to yellow and brownish, thick or liquid.)
Yellow semen is a symptom of high white blood cells and inflammation
Due to the increased content of leukocytes, semen may become yellow. There are so many of them that they turn the ejaculate yellow. In some men, sperm normally has a yellowish tint, but if it has always been white-gray in color and suddenly turns yellow, it is most likely pus, i.e. infectious inflammation in the genitourinary system.
Why are leukocytes elevated?
The source of infection should be looked for in the prostate gland, seminal follicles, scrotum, and testicles. When an inflammatory process develops in the testicles, the risk of infertility increases, since sperm maturation occurs in these organs.
To prevent infertility and eliminate the threatening consequences, you need to consult a doctor, undergo a medical examination and a course of therapy. If elevated leukocytes in the spermogram are left unattended, then the likelihood of an organic disorder of the sexual sphere increases. And this is a guarantee of infertility.
Diagnostics
After leukocytes above normal are detected in the spermogram, the following is additionally prescribed:
- Sowing ejaculate for bacteria and flora and sensitivity to antibiotics
Sperm culture should normally show a negative result, i.e. there should normally be no colonies of bacteria in the ejaculate. If pathogenic bacteria are detected during culture, the doctor will prescribe treatment with antibiotics to which they are sensitive.
Culture of ejaculate
with antibiotic sensitivity + preliminary sperm assessment
Price 3000 rub.
Address: Moscow, Begovaya st., 7, Begovaya metro station
Make an appointment by phone: +7 495 199-7554
+ MAKE AN APPOINTMENT
Acceptable norms of leukocytes
The main defenders of the immune system are leukocytes. They are the ones who prevent the invasion of foreign agents. The number of leukocytes in sperm is acceptable, but there are restrictions. If the infectious agent penetrates the genitals, the number of “white cells” increases; analysis of seminal fluid shows increased leukocytes in the spermogram.
With an increased concentration of protective cells, bacteriological seeding of sperm is prescribed in order to identify pathogens of diseases transmitted through sexual contact.
Normal white blood cell count
- In one milliliter of ejaculate – up to 1 million leukocytes
- In the field of view – from three to five cells
If elevated leukocytes are detected in the spermogram, the man is given a diagnosis that confirms inflammation of the genital organs.
Treatment of leukospermia
Treatment methods depend on the causes of the appearance of white blood cells.
Infections
, as a rule, are successfully treated with a course of antibiotics.
Non-infectious cases of pyospermia
successfully treated with non-steroidal anti-inflammatory drugs and antioxidants.
Varicocele and urethral stricture
treated surgically.
Why are antioxidants prescribed?
To protect the membrane of the sperm head from the action of free radicals.
Before prescribing them, you can take a test for oxidative stress of sperm and antioxidant activity of seminal plasma and make sure that they are necessary. If after a course of antibiotics a high level of leukocytes remains in the spermogram results
, it is necessary to look for a hidden source of inflammation. For example, get tested for an expanded list of sexually transmitted infections and conduct a transrectal ultrasound to examine the prostate gland for abnormalities.
What else can you do to help yourself with leukospermia?
- Quit smoking tobacco and/or narcotic smoking mixtures
- Reduce alcohol consumption
- Ejaculate more often (sex or masturbation)
Control sperm analysis
It takes time for the body to overcome inflammation and cleanse itself of its traces and consequences. 3 months after completing a course of antibiotics or other drugs, you must take a spermogram. This is exactly how long it takes to completely renew the germ cells in sperm. In general, if the treatment works, then not only the leukocyte level is normalized, but also other sperm parameters (for example, sperm motility or sperm count).
Prevention
Unfortunately, there are no specific preventive measures to help prevent leukospermia. Men who want to avoid an increased number of white blood cells in the seminal fluid are recommended:
- have a permanent sexual partner;
- prefer safe sex using condoms;
- take multivitamin medications;
- avoid hypothermia;
- harden the body;
- eat right, in particular, eat foods containing vitamin E and zinc;
- monitor the amount of antioxidants consumed.
It is very important to undergo regular preventive examinations with a urologist. Before planning a child, you should have sperm analyzed - this will help to diagnose the disease in a timely manner and carry out its treatment.
Patient questions about leukospermia
What medications should I take to cure leukospermia in a man?
The type, form and regimen of use of the drug completely depends on what caused the increase in leukocyte levels. If the inflammation has a pathogen, antibiotics are needed.
Can leukospermia cause infertility?
Leukocytes and their metabolic products (reactive oxygen species) affect the quality of sperm. Therefore, yes, leukospermia in men can be the reason for a partner’s failure to become pregnant. However, as a rule, all inflammatory diseases are successfully treated, so this effect of leukospermia on a man’s fertility can be called temporary.
WHO spermogram standards 2010
In 2010, WHO made changes to the ejaculate parameters, which was reflected in the 5th edition of the “WHO laboratory manual for the examination and processing of human semen”; the reference values for the number and motility of sperm, and the number of normal forms of sperm were changed.
| Index | Value (WHO 2010) |
| Ejaculate volume, ml | 1.5 ml or more |
| Total sperm count, million | 39 or more |
| Sperm concentration, million in 1 ml | 15 or more |
| Total sperm motility, % | 40 or more |
| Spermatozoa with progressive movement, % | 32 or more |
| Viability, % | 58 or more |
| Morphology: normal forms, % (according to Kruger*) | 4 or more |
*Crueg assessment uses a special stain and a complex assessment of at least 200 sperm. 4% normal sperm means that 4 out of 100 sperm should have an ideal appearance.
The head of such an ideal sperm should be oval, smooth, with a clear contour. The acrosome occupies 40–70% of the head area; in the acrosome zone there are no more than 2 small vacuoles. Head length 3.7–4.7 µm, width 2.5–3.2 µm. This measurement is carried out manually using a micrometer or using a special computer program.
The neck of a normal sperm is thin, its length is equal to the length of the head, the axis of the neck should coincide with the central axis of the head. A cytoplasmic droplet is considered abnormal if its size exceeds 1/3 of the size of the head. The main part of the flagellum should have the same diameter along its entire length (about 45 microns - about 10 times longer than the length of the head).
The Kruger standard of 4% is used only when the morphology is assessed on specially stained smears according to the criteria specified by the WHO.
Sperm motility
Native sperm (unprocessed) can contain sperm of four categories:
Category A
If the sperm moves in a straight line and travels more than half its own length per second (approximately 0.025 mm/s), it is classified in this category. About half of all group A sperm are healthy, young sperm that have recently formed in the testicles.
Category B
A sperm is classified as category B if it moves in a straight line, but its speed is less than 0.025 mm/s. As a rule, during ejaculation there are 10–15% of them. These are spermatozoa that are either aging or have a disturbed structure.
Decreased sperm motility may be associated with prolonged abstinence from sex.
Category C
If the sperm rotates in place or in a circle, it is recorded in category C. Their number is usually from 5 to 15%.
Category D
This category records how many sperm do not move at all ( azoospermia ). Approximately 50% of all group D sperm are old sperm that have either already died or are dying.
Even if you are completely healthy and have been diagnosed with normospermia or normozoospermia , semen analysis can detect sperm from all four groups.
If you have akinozoospermia , you need to find out what is causing sperm immobility . Eosin is used for this. In this preparation, the dead sperm is painted red: its membrane is quickly destroyed, and eosin easily penetrates it. Eosin cannot penetrate into a living sperm. If the sperm does not stain and does not move, this indicates that the morphology of the sperm is disturbed.
Sometimes during ejaculation all sperm are dead - this is necrozoospermia . It can be false and true. The causes of true necrozoospermia are not fully understood; it cannot be treated. With partial necrozoospermia, live sperm are less than 20%.
If, after several interpretations of the spermogram the doctor diagnoses necrozoospermia , such a married couple is recommended either adoption or artificial insemination with donor sperm.
Spermatozoon: structure of normal and abnormal forms
Sperm volume
Normospermia - 2.0–6.0 ml of sperm.
An insufficient volume of ejaculate also contains a small number of sperm . If the analysis shows that you have oligospermia , that is, an insufficient amount of sperm is released during ejaculation (less than 2 ml), this may be the cause of infertility.
A small volume of sperm also cannot protect sperm for a long time from the acidic environment of the vagina and “break” their way to the uterus.
To confirm the diagnosis of oligospermia, it is necessary to undergo a semen analysis several times. Even if the volume was less than 2 ml the first time, this is not a reason to worry.
If during ejaculation you release more than 6 ml of sperm, this will not speed up conception in any way. The fact is that approximately 5 ml of sperm is placed in the vagina. If you ejaculate more, the extra ejaculate leaks out and doesn't compete in the "who's on first" race.
Ejaculate liquefaction time
Normozoospermia involves the liquefaction of sperm within 10–60 minutes after ejaculation .
During eruption, sperm is in a viscous state. After some time, the prostate enzymes contained in the semen liquefy it. If the sperm does not liquefy, this indicates that the functioning of the prostate gland is impaired. Accordingly, the chemical composition of sperm is incorrect. This affects sperm motility and their ability to fertilize an egg. Due to insufficient liquefaction, there may be unhealthy sperm motility .
Hydrogen value (pH)
After ejaculation, sperm may die in the acidic environment of the vagina. In order for a sperm to fertilize an egg and safely pass this “barrier”, it needs protection. This is the seminal fluid : it reduces the acidity of the vagina, and the sperm can reach the uterus “alive”.
If all spermogram indicators are normal, except pH, this does not indicate any abnormalities. But together with other characteristics it can affect the diagnosis.
In azoospermia, a low pH level indicates that the ejaculatory ducts are clogged.
ASAT
ASAT are immunoglobulins (proteins) of groups A, M and G. Antisperm antibodies cause one sperm to stick to another. ASAT is formed in the body of both men and women.
ACAT can cause infertility. If the sperm is stuck to the ASAT flagellum, it moves more slowly; if the sperm is stuck to the head, it cannot fertilize the egg. the MAR test is most often used (translated from English as mixed immunoglobulin reaction - 'reaction of immunoglobulins when mixed'). If the MAR test item in the spermogram analysis shows zero, this means that you have not been diagnosed with ASAT .
Sperm color
What color is the sperm of a healthy man?
White-grayish is the color of sperm in most cases ( normospermia ).
Yellowish, milky or milky white - this color of sperm is also within the normal range ( normozoospermia ). The above shades do not indicate the presence of deviations. WHO recommends that neither the color of the semen nor its smell be taken into account.
But in some laboratories this characteristic is still recorded.
Thus, the pinkish color of sperm indicates an increased number of red blood cells in the ejaculate ( hemospermia ). With hemospermia, there may be a brownish tint to the sperm.
Transparent color of semen indicates azoospermia (semen does not contain sperm).
The importance of temperature conditions (thermal stabilization) for all embryological procedures
The body is able to maintain a constant temperature, and this process occurs with high precision. During natural conception, the egg moves towards the uterus at 37 degrees Celsius. It is very important during in vitro fertilization (and other ART methods) to provide the cells with the required temperature regime. Therefore, one of the embryologist’s goals is to bring the conditions for procedures within the IVF protocol closer to natural ones and to provide the oocytes with the required temperature. The same applies to the conditions of embryo maturation. To achieve this, the Oxy center clinic practices thermal stabilization.
Thermal stabilization involves warming up all instruments used when working with embryos and oocytes: puncture needles, catheters, tubes for follicular fluid. Maintaining the required temperature is possible thanks to special thermal tables that are equipped in the embryology laboratory.