Goals
During the procedure, the doctor may find in the patient:
- Polyps;
- Ulcers;
- Inflammation;
- Tumors.
In addition, by resorting to manipulation, the doctor can take a biopsy sample for examination, as well as perform therapeutic actions.
There is a recommendation that a colonoscopy should be performed at age 50. Everything else is individual.
Medical practice shows that most colon tumors are detected at mature stages, since diagnosis is carried out too late.
Early diagnosis allows you to identify precancerous diseases, which means you can start treatment on time. This is where colonoscopy comes to the rescue.
General information
Colonoscopy in Brest, another city, is an instrumental diagnostic method for visualization and assessment of the condition of the colon using an endoscope or a special probe. An examination is carried out for the following complaints and pathologies:
- Blood impurities in stool;
- Intestinal polyps;
- Anemia;
- Chronic constipation;
- Intestinal obstruction;
- Intestinal bleeding;
- Foreign body in the anus.
Before a colonoscopy is performed, the doctor eliminates medical contraindications and minimizes the risk of side effects and complications. Be sure to report any medications you are taking that may cause an allergic reaction during diagnosis.
Preparation
Preparation usually takes two to three days. The doctor gives recommendations to the patient, including following a diet, taking laxatives, and minimally eating the day before.
Diet plays an important role during the preparation period.
The patient needs to switch to a low-fiber diet, reduce or abandon fresh vegetables and fruits to a minimum, and forget about dried fruits, nuts, and whole grains.
A couple of days before the procedure, you need to give up solid food. There are broths, clear fruit juices, tea and coffee, jelly. The day before you need to drink more fluid.
Four hours before the procedure, you need to completely abstain from food and water, since the procedure is done on an empty stomach.
Preparatory activities
The doctor informs the patient a few days in advance about the upcoming diagnosis, focuses on dietary nutrition, and home methods of cleansing the intestines. General recommendations on how to prepare for intestinal colonoscopy:
- For 10 days, stop taking iron supplements, activated carbon, and blood thinners. Also exclude nonsteroidal anti-inflammatory and antidiarrheal drugs.
- In 2-3 days, switch to a slag-free diet, exclude meat, cereals, nuts, vegetables, and fruits from your daily diet. Dishes and food products that increase intestinal gas formation are prohibited. Here's what you can eat before a colonoscopy: low-fat kefir, diet omelet, honey, etc.
- Completely stop eating 20 hours in advance; on the day of the colonoscopy, drink only still water and weak tea.
- Before the session, take an antispasmodic according to the doctor’s recommendation, and give a cleansing enema.
Knowing how to prepare for a colonoscopy at home, you can have no doubt about the reliability of the method. During the procedure, the patient experiences discomfort, but this is a temporary phenomenon.
Methodology
Diagnostic manipulation usually takes place faster than therapeutic procedure.
Sedation is used for patient comfort.
He is laid on his left side, his legs are bent, his knees are brought to his stomach.
The colonoscope is lubricated with Vaseline and carefully inserted through the anus, moving slowly.
To ensure a good view, the intestines are inflated with gas.
The image is shown on the monitor screen, the process itself is recorded.
Dermatoscopy
After examining the intestines, the colonoscope is removed.
The drug "Fortrans" instructions for preparing for colonoscopy
Before the procedure, it is necessary to follow a slag-free diet and completely cleanse the intestines of feces.
If the colonoscopy is planned from 8.00 to 14.00
Preparation is carried out using the drug FORTRANS. At the same time, there is no need to follow a slag-free diet, as well as to perform cleansing enemas!
For effective preparation, you need to purchase 4 packets of FORTRANS at the pharmacy. Four packages must be purchased for those patients who have a large body size, constipation, adhesive disease of the abdominal cavity, previously identified lengthening or prolapse of the colon (during the passage of barium through the intestines, irrigation or colonoscopy).
On the eve of the study, you can have a light lunch (no later than 13.00) and not dinner.
Dissolve the contents of each FORTRANS package in 1 liter of high-quality drinking water at room temperature (it is convenient to use a 1.5-liter plastic mineral water bottle to dissolve the drug).
During the time interval from 15.00 to 19.00 on the eve of the study, you need to drink 3-4 liters of FORTRANS solution (1 liter of solution is drunk in 1 hour). Persons sensitive to taking large volumes of liquid (nausea, belching, etc.) are recommended to take 1 tablet of Motilium 1 hour before the start of preparation.
Approximately 1.5-2 hours after taking the first liter of FORTRANS solution, loose stools will appear, which is a natural consequence of taking this drug. Liquid stool will periodically appear several more times until approximately 21.00 - 22.00. After this, as a rule, the urge stops, and the preparation is considered complete.
At the NEOMED clinic, it is possible to perform video colonoscopy in a state of medicated sleep. If the examination is carried out under general anesthesia, please attend on an empty stomach and be accompanied.
If anesthesia is not planned, a light breakfast is acceptable.
If the colonoscopy is planned from 14.00 to 19.00
An indispensable condition for a successful colonoscopy is the complete cleansing of the colon of contents.
Preparation is carried out using the drug FORTRANS. At the same time, there is no need to follow a slag-free diet, as well as to perform cleansing enemas!
For effective preparation, you need to purchase 4 packets of the drug FORTRANS (1 box) at the pharmacy.
On the eve of the study, you can have breakfast, lunch and even a light dinner, but the last meal should be no later than 18 hours.
It is not recommended to drink carbonated drinks.
Dissolve the contents of each FORTRANS package in 1 liter of boiled water at room temperature (it is convenient to use a 1.5-liter plastic mineral water bottle to dissolve the drug).
On the eve of the study, during the time interval from 20.00 to 22.00, you need to drink 2 liters of FORTRANS solution (1 liter of solution is drunk in 1 hour). Persons sensitive to taking large volumes of liquid (nausea, belching, etc.) are recommended to take 1 tablet of Motilium 1 hour before the start of preparation.
Approximately 1.5-2 hours after taking the first liter of FORTRANS solution, loose stools will appear, which is a natural consequence of taking this drug. Loose stools will periodically repeat several more times until approximately 24.00. After this, as a rule, the urge to bottom stops, and the first stage of preparation is considered complete.
Before going to bed the night before, as well as at 7.00 on the day of the study, you can drink up to 300-400 ml of still water or weak tea.
On the day of the study, the second stage of preparation is carried out - taking two liters of FORTRANS solution from 8.00 to 10.00. After this, there will be loose stools several times again, which, as a rule, stops by 13.00. If the drug is poorly tolerated the day before, it is permissible to replace the intake of the FORTRANS solution on the day of the study with two cleansing enemas with a volume of 1.5-2.0 liters each at 8.00 and 10.00.
At the NEOMED clinic, it is possible to perform video colonoscopy in a state of medicated sleep. If the examination is carried out under general anesthesia, please attend on an empty stomach and be accompanied.
If you are not planning to undergo anesthesia for the examination, appear on an empty stomach at the appointed time (as an exception, you can take 200-300 ml of water or tea, but no later than 2 hours before the examination).
Recovery
Usually the procedure is performed in an outpatient setting. Therefore, the patient can leave the clinic as soon as the anesthesia wears off.
There are certain recommendations regarding recovery and more:
- You cannot drive or drink alcohol for 24 hours;
- Immediately after the procedure, it is recommended to walk around so that the gas leaves the intestines faster;
- It is recommended to rest during the day;
The doctor gives more specific recommendations, taking into account your condition and the nature of the procedure.
In case of fever, bleeding, or abdominal pain, you should consult a doctor.
Cost of colonoscopy
The price of diagnostics depends on the region, clinic, reputation of the proctologist-diagnostician, pain medication and other indicators. There are several options for where to have a colonoscopy in Brest: private clinics, diagnostic centers, local clinics. The diagnostic method is reliable and allows early diagnosis of neoplasms of various etiologies.
The cost of a session starts from 52 rubles. When prescribing local anesthesia or general anesthesia, the cost increases. In general, the procedure is not pleasant, but it does not cause acute pain, so you can do without pain relief and be patient.
What is a colonoscopy?
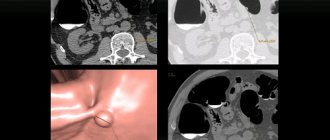
Colonoscopy (video colonoscopy) is a type of endoscopic examination during which all parts of the large intestine are examined, as well as a section of the small intestine - the ileum. An incomplete examination of the colon is called “rectoscopy” or “sigmoidoscopy”, in which only the rectum and part of the sigmoid colon are examined.
The purpose of the study is to detect any pathology of the colon. During the procedure, a very flexible, thin, completely non-traumatic endoscope with a built-in video camera at the end is inserted into the colon, allowing the doctor to evaluate the entire mucous membrane (inner surface) of the colon.
Colonoscopy is falsely associated with discomfort - many people follow unverified rumors and find dozens of what they think are “reasonable” reasons not to subject themselves to this, often the most important examination in their lives. Some people refuse to believe they are at risk for colon cancer. Some people are afraid of the pain that may occur during the study. Someone is afraid of the research results themselves - the unknown is scary!
However, none of these reasons are valid. What's more, colon cancer is one of the most preventable types of cancer, and a colonoscopy can truly save your or your loved one's life.
Only through colonoscopy can one detect and remove polyps (polypoid adenomas) of the rectum or the entire colon, which always degenerate into a malignant tumor. Colonoscopy also helps detect cancer at an early stage, which allows the disease to be completely cured in 90% of cases.
Tumors of the colon, unlike many others - for example, the stomach - always have a benign stage of development that lasts for years! And all you need to avoid tragedy is to perform a colonoscopy, get rid of polyps and return to your normal life in 1 hour!
Amazing, isn't it? It is worth taking advantage of the chance offered to us by nature and modern technology!
Colonoscopy under anesthesia
The price of a colonoscopy under anesthesia at the Central Clinical Hospital of the Presidential Administration is given below, at the end of the article.
Colonoscopy under anesthesia is an examination without pain or discomfort. At the same time, we still carry out quite a lot of examinations without anesthesia: the doctor’s experience, the latest expert-class with adjustable endoscope rigidity and the use of local anesthetic gels for the anus allow us to reduce discomfort to a minimum, and sometimes even avoid any pain. Pain during colonoscopy is usually “quite tolerable” and is caused by stretching of the intestinal lumen by the injected air and/or stretching of the intestine during difficult bends. At this point, the patient may experience short-term pain such as painful spasms.
If you are afraid of a colonoscopy, this is normal, obviously your friends or forums have already scared you.
You should know that even without anesthesia, colonoscopy (provided, of course, that the examination is performed by an experienced endoscopist) is more unpleasant than painful in more than 75% of patients.
... however, if the above argument does not convince you, simply undergo a colonoscopy under anesthesia or a “sleep” colonoscopy .
After several operations, or if an examination has already been performed and it was very painful, we certainly recommend performing a colonoscopy under general anesthesia. According to our observations, pain during examination of the intestines in these patients is, as a rule, more intense than in others, and conoscopy under anesthesia is simply the only way for them to carry out an examination, the diagnostic significance of which is difficult to overestimate.
So that you understand: the words “sedation”, “general anesthesia”, “anesthesia” and “ colonoscopy in a dream ” are the same thing. “Sedation” (translated from English as “calm”, “peace”) is less “deep” than standard intravenous anesthesia, is carried out with a different drug and can leave memories, as you understand - unpleasant and painful. In addition, the dose of the drug for traditional “sedation” is more difficult to control and can cause respiratory arrest. “Sedation”, as a rule, is carried out by the endoscopist himself, having administered the drug, but then the endoscopist is focused on the study, and not on the patient’s condition - whether the patient is breathing or no longer breathing, the endoscopist, carried away by the study, may not notice...

In our hospital, we perform intravenous anesthesia, and not “sedation,” that is, colonoscopy under anesthesia , and it looks like this: You fall asleep, then wake up - the procedure is performed, but you don’t remember anything and didn’t feel anything. All this time and 15-45 minutes after the anesthesia itself has ended, you are monitored by an anesthesiologist. We believe that this is the most optimal type of pain relief during colonoscopy. A safe drug is used, used in thousands of clinics in Europe, America and Israel; this drug has a clear dose-dependent effect - as soon as its administration is stopped, the patient wakes up. That's it, the procedure is over.
Our advantages:
The best endoscopic equipment of the highest (expert) class from the leader - Olympus (Japan) - with digital zoom and inspection functions in a narrow spectrum of light, allowing you to see early cancer with an area of 1 mm (not a typo - a millimeter!).
Friendly and polite staff.
Affordable prices - essentially “business class” at an “economy” price.
We don’t have hidden markups, like in private centers, where after research they will tell you that you owe another 5-6 thousand. Our doctors will discuss all pricing issues with you before the study begins. We are a government agency in which commercial activities are only a small part of our work.
The equipment is processed after each patient in special washing machines (also manufactured by Olympus), which completely eliminates the possibility of transmission of infection from one patient to another. Processing in a washing machine is considered the gold standard for processing endoscopes, but leads to an increase in the cost of the study; however, the clinic’s policy is not to skimp on the safety of our patients.
We conduct research on weekends and holidays - our service operates seven days a week.
The substance used for intravenous anesthesia in our department is the safest; it is used for anesthesia in all clinics in Europe and the USA. However, the anesthesiologist is responsible for your life and therefore has the right to request the following tests:
smear (PCR) for COVID-19 - later than 4 days from the date of collection of the material.
ECG - to be sure that you are not suffering a heart attack “on your feet” right now)
general (clinical) blood test - in order to know that your hemoglobin level will allow you to adequately saturate your blood with oxygen even during sleep;
biochemical blood test - to be sure that the liver and kidneys neutralize the anesthesia drug as expected and you will wake up easily and on time.
Colonoscopy under anesthesia or “in a dream” - price (valid for the period until the end of 2021) - from 2 1 thousand rubles,
(the price includes everything that is required to conduct the study under anesthesia: preliminary examination and consultation with an endoscopist, placement of a catheter for drug administration, consultation with an anesthesiologist, colonoscopy itself, stay and awakening in a day hospital bed under the supervision of experienced staff, explanation by the doctor -endoscopist results obtained during the study)
Please note that when drawing up a contract in the commercial department of the Central Clinical Hospital, an advance payment is taken not only for the study, but also an advance payment covering a possible biopsy or polyp removal, i.e. To formalize the contract, an amount of at least 30 thousand rubles will be needed. In the case where the manipulation is limited only to the examination itself (colonoscopy), the advance overpayment is, of course, returned to the patient on the same day after the final payment.
Often in our sleep we carry out both endoscopic examinations at once - conoscopy and gastroscopy (the so-called “check up”) - the increase in price is insignificant, but for one anesthesia in a dream, without pain and without discomfort, both the stomach and the large intestine are examined immediately - the price is from 25 thousand rubles.
Please note that the price may be slightly changed in one direction or the other; in any case, it is better to check the prices by phone in the Contacts section before your visit
How the research works
Colonoscopy probe
The procedure lasts from 15 to 30 minutes. During the examination, the patient is on his side. The doctor carefully inserts a soft, flexible colonoscope into the anus and gradually moves it further. A small amount of air is periodically injected through the endoscope to maximize the straightening of the folds of the intestine and provide maximum visibility of the entire mucous membrane. During or after the procedure, the patient may feel mild bloating; this is normal. During the procedure, the doctor may take a biopsy (small pieces of tissue) or remove polyps, which is necessary for an accurate diagnosis of the pathology. In a hospital setting, colonoscopy can be performed using anesthesia.
Cost of treatment
Free treatment under compulsory medical insurance policy
A type of social insurance for citizens of the Russian Federation, which provides guarantees of free medical care in the detection of surgical diseases.
Quota treatment (VMP)
Providing medical care for the most severe diseases of the gastrointestinal tract, requiring the mandatory use of expensive instruments and/or the use of complex surgical techniques.
Specialists
The colonoscopy procedure in our Clinic is performed by the head of the department of diagnostic and therapeutic endoscopy, Ph.D. Pavel Vladimirovich Pavlov is a specialist who has been performing this research since 2003, and also performs all known endoscopic intraluminal operations on the intestine: polypectomies, mucosectomies, dissections in the submucosal layer, bougienage, balloon dilatations, stenting and others. Pavel Vladimirovich has extensive experience in the diagnosis and treatment of early cancer not only of the colon, but also of the entire digestive tract.
Candidate of Medical Sciences also deals with diagnostics and therapeutic interventions on the intestine. Afanasyeva Aigul Fanzirovna is a doctor who has devoted herself to endoscopy since 2003, performing most endoscopic intraluminal interventions on the digestive tract and has deservedly established herself as a brilliant specialist.
What should you watch out for during a colonoscopy?
Colonoscopy has become a fairly popular procedure, which is now performed in various clinics. Despite its widespread use, colonoscopy is an invasive procedure that should only be performed by an experienced and qualified specialist using modern high-tech equipment.
Side effects of a “poor” colonoscopy:
- Damage (perforation) of the colon is an extremely rare, but very dangerous complication that requires immediate surgical correction and most often occurs when the medical staff is extremely poorly prepared, excessive haste, and the desire to perform the study “fastest in Moscow.”
- Bleeding after colonoscopy is also an extremely rare complication and has the same causes as perforation.
- Improper removal of the polyp means the persistence of residual tumor, which entails progression of the disease, while the patient is completely confident in his recovery.
- Incorrectly selected anesthesia causes difficult awakening, nausea, dizziness and even vomiting, headaches, general weakness, and temporary loss of performance.
Be careful when choosing a clinic for a colonoscopy, beware of “counterfeits”. The study must be carried out by an experienced and qualified specialist.
Indications for colonoscopy
The main indications for colonoscopy, which we use in our clinical practice, may be one or more symptoms:
- Stomach ache
- Abdominal mass (on ultrasound, fluoroscopy or computed tomography)
- Unreasonable weight loss
- Iron deficiency anemia (especially in men of any age)
- Increased ESR (erythrocyte sedimentation rate)
- The appearance of blood from the rectum while maintaining the frequency and consistency of stools
- Monitoring patients with previously diagnosed colitis, Crohn's disease or ulcerative colitis
- Monitoring of patients with familial intestinal polyposis
- Monitoring patients after previous polypectomies
- Observation of patients with operated colon (inflammatory bowel diseases, familial polyposis, cancer)
- Increased levels of calprotectin in feces
- Prolonged diarrhea (especially during long-term antibiotic therapy)
- Examination of patients whose close relatives have been diagnosed with adenomas or colon cancer
- Presence of mutations in the BRCA 1 and BRCA 2 genes
- Preparing the patient for surgery for chronic bleeding hemorrhoids or anal fissure
When is it necessary to have a colonoscopy?
Colonoscopy on a regular basis - once a year, is recommended for all patients over 45 years of age. If your family has had or has relatives diagnosed with colorectal cancer, then you must perform the first test no later than 25-30 years of age, and then follow the recommendations that you will receive at the end of the procedure.
You must also undergo a video colonoscopy if you are suspected of having one of the following diseases:
- Crohn's disease
- Ulcerative colitis
- Pseudomembranous colitis
- Ischemic colitis
- Solitary rectal ulcer
- Rectocele
- Diverticular disease
- Volvulus
- Colon tumor