November 30, 2017
November 30, 2017
- Indications for use
- What does a head CT scan show?
- Brain
- Paranasal sinuses
- Temporal bones
- Facial bones
- Brain vessels
- Jaw
- Eye sockets
- Larynx
- Teeth
- Soft tissues of the neck
- Scull
- Inner ear
CT scan of the head is an accurate, highly informative and irreplaceable method for studying the entire bone structure of the head and internal organs. The examination is based on the principle of layer-by-layer scanning of the head with X-rays.
The head is the most important part of the human body, since it contains the brain and other vital organs.
In case of prolonged headaches, nausea, or a sharp decrease in visual or hearing acuity, it is important to investigate its condition.
To diagnose the condition of the head, the following CT examinations are prescribed: the brain, paranasal sinuses, temporal bones, facial bones, cerebral vessels, jaw, orbit, larynx, teeth, soft tissues of the neck, skull and inner ear.
In many cases, in conjunction with the above studies, CT scans of the vessels of the head and neck are performed.
Indications for use
A referral for an examination is issued by a neurologist, ENT doctor, oncologist, traumatologist, psychologist, surgeon or therapist. The main purpose of the study is to make an accurate diagnosis, refute or confirm a previously made diagnosis.
A CT scan of a specific part of the head is prescribed for the following indications::
- Frequent headache of unknown etymology;
- Convulsions;
- Rapid deterioration of vision or hearing without serious reasons;
- swelling of the face or neck;
- Presence of head injury;
- Pathologies of coordination;
- Lack of balance;
- Suspicion of oncology;
- Constant increase in blood pressure (blood pressure);
- Foreign bodies;
- Diseases of the central nervous system.
Computed tomography allows you to diagnose the presence of minor pathologies and serious diseases at any stage, which is of great importance for patients with diseases for which treatment must begin immediately.
Indications
CT is prescribed to detect inflammatory processes, brain tumors, hemorrhages and the consequences of traumatic brain injury (TBI).
In addition, computed tomography is one of the methods for monitoring the effectiveness of treatment and rehabilitation for various diseases - the bones of the skull, membranes and structures of the brain, blood vessels and paranasal sinuses are clearly visible in the images.
A computed tomography scan of the brain may be prescribed by the attending physician (therapist) or a neurologist in the following cases:
- suspected swelling, inflammation, hemorrhage after TBI;
- acute circulatory disorder (stroke);
- abscess and cysts of the brain;
- infectious diseases (encephalitis, meningitis);
- oncopathology (tumors, metastases);
- abnormalities in the development of brain structures and blood vessels;
- pathologies of blood vessels (thrombosis, aneurysm);
- hydrocephalus (“dropsy” of the brain - excessive accumulation of cerebrospinal fluid (CSF) in the ventricular system of the brain);
- convulsions, visual disturbances, dizziness, decreased sensitivity, confusion - neurological symptoms for no apparent reason;
- causeless headaches for 2-3 months or more;
- preoperative examination;
- individual contraindications to MRI (presence of a pacemaker, insulin pump, metal prostheses).
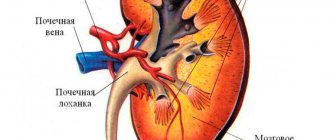
Facial bones
The facial bones are an important component of the skull and are included in the masticatory apparatus (paired maxillary bone and lower jaw). A recommendation for testing is given for headaches, swelling of the soft tissues of the facial area, nasal discharge, rapid deterioration of visual acuity and frequent pain in this area. Diagnostics reveals damage, deviated septum, the presence of a foreign body and pathological changes in blood vessels.
It lasts about 30 minutes, and the average price in Moscow ranges from 3,000 to 4,900 rubles.
Contraindications to CT scan of the brain
For CT diagnostics, X-ray radiation is used, albeit in a minimal dosage. Therefore, CT scanning is not recommended for pregnant women (risk of developing birth defects in the child).
Note: CT scanning with contrast is not contraindicated for nursing mothers if after the procedure the baby is weaned from the breast for 2 days (the contrast agent enters the secretions of the mammary glands).
Also, contrast-enhanced CT is not advisable for individuals with severe renal impairment. When the drug is excreted in the urine, side effects may develop in the form of intoxication (poisoning).
Acute pain syndrome and pathological inability to remain still (hyperkinesis) can become a serious obstacle to the study, since you cannot move during the procedure.
Contrast agents should not be administered to people who are allergic to iodine.
It is advisable to avoid any kind of radiation, including minimal radiation, for patients with multiple myeloma and those suffering from endocrine pathology.
For psychologically unstable individuals, as well as for patients with claustrophobia, CT is either not prescribed at all or is performed in a state of light medicated sleep.
And for obese people (weight over 120-130 kg), a CT scan is simply impossible, since their body volumes may exceed the diameter of the diagnostic chamber.
Inner ear
The inner ear is a system of canals in which the auditory and vestibular analyzers are located. The main reason for prescribing a diagnosis: a sharp deterioration in sound quality, pain in the ear, fluid from the ear canal, noise and injury. CT images can detect the following pathologies: damage or displacement of bones, infectious or inflammatory processes, as well as angioma.
On average, diagnostics takes 5-10 minutes, and the cost ranges from 4,500 to 6,000 rubles.
Share link on social networks
Methodology
The duration of the procedure ranges from 2-3 minutes to half an hour, depending on the purpose of the study. Before the examination begins, the patient must remove all jewelry and metal objects.
The patient is positioned on a movable couch in the chamber, his head is secured with a special fixing device (it is required to remain completely still). The table with the patient moves inside the tomograph. During scanning, the outer part of the device will rotate around its axis, and the couch under the subject will move slightly in the horizontal plane. The tomograph makes a slight noise during operation, which does not cause much discomfort to the patient.
During the procedure, the medical staff is in an adjacent room and observes the process through glass. At the same time, a two-way connection is maintained with the patient: the doctor can inquire about his well-being, and he, in turn, can report any changes in his condition.
When a contrast agent is injected, you may experience a metallic taste in your mouth and a feeling of warmth or cold spreading through your veins. This is a normal reaction of the body to the administration of the drug.
It is not normal for the patient to experience nausea, dizziness, headache or stomach discomfort. He should immediately report these symptoms to his doctor. This may be a side effect of the injected contrast agent.
Computed tomography for children
CT scanning can be performed on children from 3 years of age (for emergency indications), if they can lie still for 15-20 minutes. If this is not possible, then the child is given a light anesthesia. Otherwise, the procedure for examining children is no different from adult tomography.
Complications
There are no serious complications after computed tomography, except for allergic reactions to the contrast agent. But this may not happen if the medical staff of the institution collects the history of the patient’s life and illness correctly and as completely as possible.
general information
Computed tomography (CT) is a cross-sectional imaging technique based on the X-ray principle.
A tomograph's X-ray tube is not static, unlike a conventional X-ray machine. Together with a digital detector, it rotates around the patient at high speed (up to 4 revolutions per second) inside the tomograph body, which is called a gantry. During scanning, the patient moves on a special table along the longitudinal axis of the body into the gantry aperture, so the X-ray beam “draws” a spiral trajectory on his body, hence the name spiral and multispiral computed tomography. From the data obtained by the detector, a three-dimensional model of the area under study is formed, and then sections in various planes are formed.
What are the contraindications to CT?
Most patients tolerate the study well and particularly appreciate its painlessness. However, brain CT has limitations. The following conditions have been added to this category:
- Carrying a child. Screening is not carried out to prevent the development of pathologies in the fetus after receiving a dose of radiation.
- Patient obesity. If a person weighs more than 200 kg, tomography is not performed for technical reasons - the patient simply cannot fit into the scanner.
- Mental disorders. These diseases are accompanied by inappropriate behavior of the patient, which causes difficulties in diagnosis.
- Allergy to contrast. Individual intolerance to the dye leads to refusal of testing with an additional enhancer and the appointment of an alternative diagnostic method.
- Kidney or liver failure. CT with contrast is contraindicated, since drug removal requires stable operation of the excretory system, which is not important for such diseases.
Alternative methods - MRI
Unlike magnetic resonance imaging (MRI), which is most effective in studying the physical state of the brain, CT studies the chemical structure of tissues. That is, CT allows you to determine their X-ray density, which usually changes with various diseases.
When examining the brain, MRI perfectly visualizes soft tissues, which is important for diffuse and focal lesions of brain structures and pathologies of the spinal cord. But on an MRI, the bones of the skull are practically not visible - a CT scan of the brain in this regard provides much more information. Therefore, in some cases, both studies are prescribed simultaneously, as complementary to each other and giving the most complete picture of the disease.
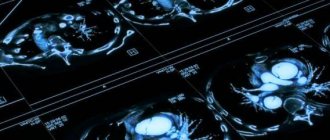
CT scan of the brain (systematic approach)
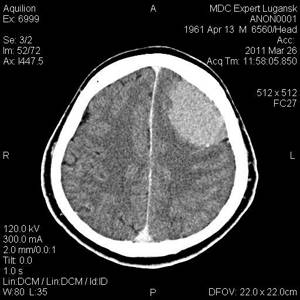
The approach to analyzing CT images of the brain should undoubtedly depend on the clinical problem and the patient's condition, but most radiologists repeat the same steps regardless of the input data and the clinical situation.
Input data analysis
Key points
- Make sure the data on the image matches the patient data
- Review previous studies and their descriptions (if available)
- View images in the brain and bone window
- View images with modified window width to identify subarachnoid hemorrhage
Patient details on image
Before starting the analysis, always check the consistency of the patient’s data (last name and initials, date of birth), date and time of the study on the obtained images. Make sure you are describing a current study and not a study from an archive or a study from another patient.
Analysis of previous images and their descriptions
Analysis of archived images is a key point in the work of a radiologist. Very often, only a comparison of the current picture with previous images allows one to obtain important information and draw correct conclusions about the changes/pathology present. It is equally important to read the previous descriptions (if any).
Choosing the right window width
CT scanning provides a 3-dimensional map based on the varying densities of anatomical structures. These CT data can be presented in a variety of ways allowing structures to be visualized over a given range of densities. ' brain window ' uses a range of densities close to the average density of brain structures, but carries limited information about the state of bone structures. ' Bone Window ', due to its narrower range, makes it possible to highlight structures close in density to bone tissue, but does not allow a detailed analysis of the structures of the brain. In the evaluation of brain CT, the use of both the brain and bone windows should be routine, and image analysis using them should become a habit. In addition, modification of CT window parameters often helps in the diagnosis of hemorrhages.
Analysis of images in orthogonal planes
CT images of the brain are obtained in the axial plane (which the laboratory technician sets, for example, parallel to the plane of the base of the skull), this approach allows to reduce the overlap of artifacts from the dense structures of the bones of the base of the skull on the structures of the brain. Modern tomographs allow the obtained axial images to be reconstructed in other planes, which helps in a more detailed assessment of the pathology. The most commonly used are the orthogonal coronal (parallel to the medulla oblongata) and sagittal (through the midline structures) planes.
Research quality and artifacts
Key points
- Check availability of medical products
- Common artifacts are motion artifacts, scattering artifacts, and radiation hardening artifacts.
- Evaluation of the entire series of images, rather than a single slice, avoids possible errors
Artifacts
The quality of images is often limited by the quality of the CT scanner, the experience of the x-ray technician, and the severity of the patient's condition, which reduces his ability to follow commands. You should always be aware of the most common artifacts. In addition, do not forget that some of them cannot be avoided.
Artifacts from medical devices
The presence of medical devices, as evidence of previous manipulations, should always be displayed in the description of the study.
Artifacts from motion
The patient's movement during the examination leads to the appearance of artifacts on the images that complicate interpretation, sometimes to the point of complete impossibility of analysis. In such cases, it is necessary to either repeat the study or note in the protocol that the obtained images are of unsatisfactory diagnostic quality. This is important because motion artifacts at the interface of media can give a false impression of the presence of a pathological process.
Artifact of Increased Cruelty
CT images of the brain often show dark and light bands at the base of the skull. These commonly seen lines usually run between two dense parts of the skull (for example, the projections of the internal endplate of the calvarium or the petrous part of the temporal bone). These artifacts are formed partly by scattering of x-rays and partly by changes in average power as a result of absorption and attenuation of x-rays as they pass through dense structures. The base of the skull is the area in which this artifact is most often found. After X-ray radiation passes through the dense structures of the temporal bones, stripes of reduced density are visualized in the bridge. The clinical significance of this phenomenon lies in the limited possibility of reliable assessment of stem structures.
Series of images or single slice
When evaluating a CT scan of the brain, it is important to analyze the entire series of images, not just a single slice, without comparing it with the underlying and superior slices.
Contrast enhancement
The administration of intravenous contrast agents allows us to obtain additional information about the anatomical features or pathological process. As a rule, a native study is performed first, and in case of detected pathology (for example, solid or cystic formation) and in the absence of contraindications, a repeat study with contrast enhancement is performed.
Analysis of damage to soft tissues and bones of the skull
Key points
- The sutures of the skull are serrated
- Fresh skull fractures have a linear, straight course and are not covered by periosteum
Analysis of CT images of the brain requires systematic evaluation of images in both the bone and brain windows. Bone window assessment in the context of trauma identifies skull fracture(s). The brain window is used to look for cerebral contusions and intracranial hemorrhages. Evaluation of both the bone and brain windows allows us to obtain a more detailed picture of damage to the soft tissues of the head, which complements the clinical picture.
Fractures or sutures
In case of head trauma, knowledge of the normal pattern and anatomy of sutures allows one to avoid interpretation errors.
The sutures of the bones of the cranial vault are localized in typical anatomical areas and are classified as serrated sutures. Fractures, unlike sutures, cross the inner and outer endplates in a straight line.
The edges of the sutures are covered with periosteum, which, continuing continuously, passes from the internal endplate to the external one. Unlike sutures, fractures of the calvarial bones are not covered by periosteum. Illustration 3.1
Severe trauma leads to the formation of depressed skull fractures. Similar to linear fractures, the bone window allows for a detailed assessment of bone damage, and the brain window allows for the identification of concomitant intracranial hematoma.
Fractures of the base of the skull are sometimes difficult to visualize directly, but in the pyramid of the temporal bone (if there is a history of trauma), darkening of the air cells can help identify the fracture.
Assessment of brain volume and subarachnoid spaces
Key points
- Evaluation of subarachnoial spaces
- It is easier to assess the size of the grooves at the apex of the cranial vault.
- The age of the patient must be taken into account
Brain volume/Volume of subarachnoid spaces
Brain volume is assessed subjectively by relative assessment of the volume of the cisterns. In this case, the age of the patient must be taken into account. The ventricles may be small in young patients and quite large in older patients. And in both cases this should be considered the norm. Brain volume decreases with age due to natural aging and diseases such as dementia or alcoholism. There is no uniform approach to assessing brain volume. The assessment can be carried out subjectively by determining the volume of spaces containing cerebrospinal fluid (sulci, fissures, ventricles and cisterns). Read more…
Hydrocephalus
Hydrocephalus results from increased production or decreased absorption of cerebrospinal fluid. Hydrocephalus can lead to marked enlargement of the ventricles. Acute hydrocephalus can lead to damage to the ependyma (lining the ventricular cavity) causing swelling of the periventricular white matter, so-called transependymal edema. Read more…
Alzheimer's disease
Alzheimer's disease, the most widely known example of dementia, cannot be diagnosed by imaging alone. However, this disease is characterized by a typical pattern of local reduction in brain volume in the temporal lobes. Read more…
Increased volume (cerebral edema)
Generalized cerebral edema can cause swelling leading to reduction of subarachnoid spaces and decreased differentiation of gray and white matter. One example is hypoxic injury, in which the boundary between gray and white matter in the affected area is blurred, and cell swelling leads to the reduction and smoothing of the grooves. Read more…
Chronic ischemia
Key points
Chronic ischemic changes are often found on computed tomography of the brain. This concept includes disease of small vessels of the brain, old lacunar infarctions or consequences of territorial strokes/infarctions.
Small vessel diseases
Generalized low-density changes in the white matter of the brain without clear boundaries are a common sign of chronic ischemia due to pathology of small vessels. These changes are combined with such risk factors as smoking, diabetes, arterial hypertension. In many patients, signs of small vessel pathology are combined with a decrease in brain volume.
Lacunar infarction
Lacunar infarction is an area of brain cell death due to local ischemia. Lacunar infarctions are most often localized in areas supplied by the perforating branches of the middle cerebral artery. An acute lacunar infarction may not be visible on an initial CT scan, but after a few weeks it is visualized as a well-demarcated area of reduced density. Read more…
Post-stroke changes
Although stroke in the acute and acute stages is not always easy to detect on CT scans, over time, cell death leads to the formation of an area of reduced density in the affected area of the brain. Post-stroke changes are visualized as a clearly demarcated low-density zone, representing cystic-glial changes and extending to both white and gray matter. These changes are often localized in the middle cerebral artery.
Acute cerebral ischemia (stroke)
If an acute ischemic stroke is suspected, a CT scan of the brain often does not have pathological changes; the main purpose of the study is to exclude intracranial hemorrhage.
Key points
- If acute cerebral ischemia is suspected, computed tomography is performed to exclude hemorrhage
- Systematically look for areas of reduced density in the brain parenchyma
- Check for signs of hyperdense middle cerebral artery and attrition/blurring of gray and white matter boundaries in the insular lobes
Acute stroke
Often, CT is performed in the acute period, when the area of reduced density in the affected area of the brain is not yet visualized. In such a situation, positive signs of hyperdensity of the middle cerebral artery and a sign of decreased differentiation of the insular cortex can help. Main article
Sign of cerebral artery hyperdensity
If an acute cerebral stroke is suspected, computed tomography can sometimes reveal the accumulation of thrombotic masses in the middle cerebral artery. ( Illustration 6.1
) Read more…
Decreased differentiation of the insular cortex
If a cerebral stroke is suspected, computed tomography may visualize a sign of decreased differentiation of the insular cortex. This sign is rather inconspicuous and is easily missed if due attention is not paid to it. ( Illustration 6.2
) Read more…
Extra-axial hemorrhages
Key points
- Epidural hemorrhages often have a lenticular shape
- Subdural hemorrhages often have a crescent shape
- Subarachnoid hemorrhages occur in spaces filled with spinal larkspur - grooves, fissures, ventricles, basal cisterns
Intracranial hemorrhages are divided into intra-axial (into the brain parenchyma) and extra-axial (outside the brain). Extra-axial hemorrhages are divided into epidural, subdural and subarachnoid.
Epidural hematoma
Epidural hematoma is the result of post-traumatic injury to intracranial vessels, most often the middle meningeal artery. Blood from the damaged vessel accumulates between the detached layer of the dura mater and the internal endplate of the skull bone. An epidural hematoma often has a lenticular shape, since the dura mater tightly fuses with the bones in the area of the cranial sutures. Detachment of the dura mater is limited to the attachment sites and thus limits the volume of the hematoma. An epidural hematoma is often (but not always) associated with a calvarial fracture, so be sure to check the bone window images. Your illustration could be here

Read more…
Subdural hematoma
Cerebral veins are quite fragile vessels. The risk of damage increases with age and is exacerbated when the patient is prescribed anticoagulants. Subdural hematomas can occur with minimal traumatic exposure. If risk factors are present, there may be no history of trauma at all. Subdural hematomas are not limited to the areas of attachment of the dura mater to the bones of the cranial vault. As a result, the accumulation of blood often has a crescent shape. The subarachnoid spaces remain intact and blood does not fill the grooves. The density of the hematoma depends on the duration of the hemorrhage. The grooves and subarachnoid spaces on the affected side can be reduced due to the volumetric effect of the hematoma. ( Illustration 7.1
) Read more…
Subarachnoid hemorrhage
Subarachnoid hemorrhage often accompanies not only injuries, but also occurs spontaneously, for example, as a result of bleeding from an aneurysm. In this case, aneurysms are visualized on routine CT scans only if they are sufficiently large in size. Less often, subarachnoid hemorrhages occur with congenital arteriovenous vascular malformations or as a result of hemorrhage from the veins of the brain stem (Perimesencephalic nonaneurysmal subarachnoid hemorrhage).
Blood in subarachnoid hemorrhage can be localized in any space normally filled with cerebrospinal fluid - grooves, fissures, cisterns of the base of the brain or the ventricular system. Read more…
Intracerebral hemorrhage
Key points
- manifestations of spontaneous and post-traumatic intracerebral hemorrhages are often identical
- intracerebral hemorrhages can be combined with extra-axial hemorrhages
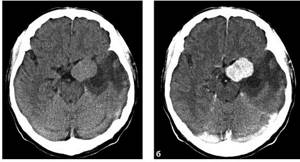
Intra-axial (syn. intracerebral) hemorrhage can occur spontaneously or due to traumatic exposure. Without an appropriate CT history, the CT picture for both spontaneous and post-traumatic hemorrhage may be identical, since the injury is not always accompanied by skull fractures.
Spontaneous intracerebral hemorrhage
Spontaneous intracerebral hemorrhage often presents as an area of increased density (blood) surrounded by a perifocal area of low density (edema). //TODO NB in general, the density of the hematoma and the severity of perifocal edema depend on the timing/age of the hematoma More details...
Combination of intra- and extra-axial hemorrhages
Very often, intracerebral hemorrhages (spontaneous or traumatic) are combined with extra-axial hemorrhages.
Intracranial space-occupying formations
Key points
- Intracranial tumors can be intra- and extra-axial
- A single intra-axial formation is more often a malignant tumor
- Multiple intra-axial formations are often represented by metastases
- Brain abscess is one of the most important entities in the differential diagnosis of formations with ring-shaped accumulation of contrast
- Meningioma is the most common extra-axial tumor
Intracranial space-occupying formations, depending on their location, can be divided into intra-axial and extra-axial, while a clear distinction based only on CT data is not always easy to determine.
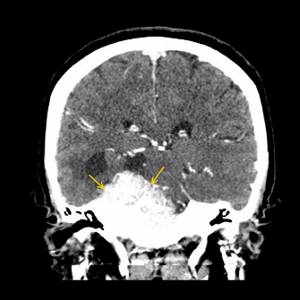
Intra-axial formations
Intra-axial mass lesions can be of a tumor or non-tumor nature, and tumor tumors, in turn, are divided into malignant or benign. Very generally, a single intra-axial lesion enhancing after intravenous contrast and surrounded by perifocal edema with mass-effecting surrounding structures will more often represent a primary malignancy (eg, glioma), whereas multiple intra-axial lesions with the same characteristics (contrast uptake, edema, volumetric effect) will be metastases. Illustration 9.1
Read more: Classification of tumors of the central nervous system, Metastatic brain tumors, Brain abscess, Ring-shaped accumulation of contrast
Extra-axial formations
Meningiomas are the most common extra-axial lesions. Despite their benign nature, they can reach large sizes and may be accompanied by edema in the adjacent parts of the brain. Typically, meningiomas have smooth, clear contours and may contain calcifications in their structure. On post-contrast images, meningiomas are characterized by pronounced homogeneous contrast enhancement. Meningiomas originate from the meninges, which also accumulate contrast in the adjacent sections, forming the characteristic sign of a dural tail. Illustration 9.2
Read more…
Volumetric effect
Key points
- Pathological processes can cause volumetric effects - displacement or compression of brain structures
- Massive effects may be caused by tumors, hemorrhage or edema
The brain is a soft tissue structure located in a limited space of the cranium. Since its volume is unchanged, any pathological process accompanied by a change in volume can lead to increased intracranial pressure and displacement of brain tissue. These changes are called “volumetric impact” .
Intracranial pressure during pathological processes such as tumors and hemorrhages can cause volumetric effects. Perifocal edema can also enhance the volumetric effect in the case of infarction, which in itself is not a “volumetric” process, and the volumetric effect in this case is due solely to edema.
Stages of volumetric influence
Volumetric impact during intracranial volumetric processes increases according to a predictable scenario. First, smoothness of the furrows adjacent to the zone appears. Then complete or partial compression of the adjacent ventricle . Smoothing of the sulci and compression of the ventricle can extend to the entire hemisphere. This is followed by displacement of the midline structures , followed by compression of the contralateral ventricle and the sulci of the contralateral hemisphere. In severe cases, CT reveals dislocation of brain structures through the notch of the tentorium cerebellum (which under normal conditions contains the brain stem and basal cisterns), or even extrusion of the structures of the posterior cranial fossa through the foramen magnum. The latter changes are quite rare and are observed (are predictors) with an unfavorable outcome. Illustration 10.1
CT scan of the brain with contrast
Brief description of the procedure
Duration: 10-35 minutes Necessity of using a contrast agent: as prescribed by a doctor Necessity of preparation for the study: no Presence of contraindications: yes Restrictions: available Time to prepare a report: up to 1 hour Children: over 14 years old
What is a contrast agent?
In computed tomography and radiology in general, the contrast of images is determined by the difference in the absorption of X-rays by tissues of different densities. Even structures of minimal size that block radiation are well visualized against the background of tissues that are transparent to X-rays. To maximize the difference in the intensity of absorption of X-rays by body tissues, artificial contrast is used - the introduction of a special X-ray contrast agent into the patient’s body.
For CT scans of the brain, water-soluble contrast agents containing iodine are used. When introduced into the circulatory system, such drugs stain the vessels and penetrate through the bloodstream into the interstitial space, increasing its natural contrast. The contrast is then removed from the patient's body through the urinary system.
In the procedure of CT of the brain with c/u (contrast enhancement), the drugs Omnipaque and Ultravist are mainly used. Their dosage is calculated according to the patient’s body weight.
Contrast injection methods
With contrast CT of the brain, neck and other organs, except for some cases of examination of the digestive system, the drug can be administered into the patient’s blood in the following ways:
- “manual” intravenous contrast, in which an x-ray technician or nurse administers the drug by injection, without adjusting the speed and time of its delivery. A CT scan of the brain begins when the drug is completely injected into the bloodstream. This contrast method is considered obsolete and is used on first-generation equipment;
- bolus intravenous contrast, when the drug is administered automatically using a syringe injector. In this case, the time and speed of its administration are controlled. This method is widely used in multislice CT of the brain, and its main purpose is to separate the phases of the examination.
What pathological processes does a brain CT scan with contrast reveal?
X-ray contrast CT of the brain is widely used in medical practice. Since tumors, regardless of etiology, are well supplied with blood, contrast is widely used to identify tumors and metastases, determine the exact location of their location, structural features, nature, and relationships with neighboring tissues and organs.
Also in demand is a CT scan of brain vessels with contrast - the technique successfully diagnoses various pathologies and anomalies of vascular development, which include arteriovenous malformations, stenosis, sites of blood clots, areas of aneurysms, tumor processes of blood vessels, occlusions and other disorders.
Contraindications to CT scan of the brain with contrast
Due to the content of iodine compounds in the composition of the contrast agent, its administration has a number of restrictions. It is not recommended to perform a contrast CT scan of the head in patients with diabetes mellitus, renal failure, multiple myeloma, pathological processes in the thyroid gland, or allergies to iodine.
During lactation, women should stop feeding for 24 hours after a contrast CT scan of the brain - this time is necessary for the drug to be completely eliminated from the body.
CT scan of the brain: photos of various pathologies
Images obtained during a CT scan of the head are black-and-white images of the structures and tissues of the head: ventricles, temporal bones, subarachnoid space, skull base, brain stem, liquor spaces, gray and white matter, arteries, veins, venous sinuses, bone tissue skull and other structures.
Photos taken in three projections can be converted into a spatial model of the brain, on the basis of which the location of head structures relative to each other can be assessed.
How are various brain disorders visualized in photographs?
Pathological processes of the brain appear in the photo as areas of darkening, clearing, or their alternation. However, the X-ray density of some abnormalities may coincide with the density of healthy tissue, in which case they resort to intravenous administration of contrast agents or the use of alternative diagnostic methods.
Let us give examples of photographs of some disorders and post-traumatic conditions obtained during a brain CT scan.
With mild brain contusions resulting from traumatic brain injury, CT may reveal a limited area of traumatic edema, which is characterized by reduced density. Below is an example of such a bruise.
Let's look at an example of a CT image of a brain abscess without and with contrast. In the photo without contrast, a dark lesion is visible; in the image with enhancement, the abscess capsule, which is indicated by arrows, and the area of edema are clearly visualized.
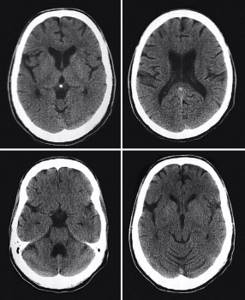
With bruises of moderate severity, the photo shows a significant number of small hemorrhages, which have an increased density and are localized in the area of edema. In some cases, narrowing of the intrathecal spaces and ventricles of the brain may be noticeable. The following photograph shows the CT dynamics of changes in the brain with this degree of injury: the top row shows the condition upon admission. In the area of the parietal and partially temporal lobes, areas of hemorrhagic impregnation are located non-compactly, which are surrounded by perifocal edema. The middle row shows photos of the condition on the 9th day after the injury. A decrease in the density of hemorrhagic foci was visualized, but the persistence of perifocal edema was noticeable. Bottom row: condition 1 month after injury. Moderate focal changes are noticeable in the area of hemorrhagic contusion.
In severe cases of brain contusion, the images reveal cerebral edema and/or a zone of crushed tissue, where clots of fresh blood are revealed as small areas of increased density. An example of a CT image of such a bruise is shown below.
Diffuse axonal damage resulting from a head injury is characterized by the presence of cerebral edema on images, against which small hemorrhagic foci may be visible in the corpus callosum, subcortical structures, and white matter. Below is a photograph of such a violation.
Tumor formations are detected using contrast enhancement based on direct (changes in density) and indirect (cerebral edema, blockage of the cerebrospinal fluid pathways, changes in the size of the ventricles, their compression, etc.) signs. Carrying out differential diagnosis between benign and malignant diseases is also based on the features of a photo CT scan of the brain with contrast. In particular, the malignant process is characterized by alternating zones of increased and decreased density, as well as the presence of an area of necrosis inside the tumor. Next, let's look at photographs of some head tumors.
Below is a photo of a cerebral tumor without contrast. It is located on the bone tissue of the base of the skull and has a heterogeneous structure. An area of perifocal edema is noticeable around the formation.
Now let's look at a photo of the same tumor, but with contrast. The tumor formation has accumulated the contrast agent to a significant extent, which indicates the presence of a developed vascular system in it. The tumor is marked on the images with arrows.

Brain hematomas of an epidural nature in the photo look like bi- or plano-convex areas under the calvarium, which have an increased x-ray density. The photo shows an example of this type of hematoma. The arrow indicates the area of hemorrhage.
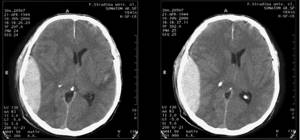
Subdural hematomas are visualized as crescent-shaped areas of increased density. The photo below shows an acute subdural hematoma. Above the area of the right hemisphere, a crescent-shaped structure of increased density is visualized (indicated by an arrow).
Intracerebral hematomas also have increased density, but are characterized by an irregular or round shape and are located in the substance of the brain. An example of an intracerebral hematoma:
Obtaining a photo of the brain using contrast-enhanced CT allows one to distinguish tumors from cystic formations - tumor cells actively accumulate contrast, while cyst tissue remains inert to the drug. Below is an example of a tumor process before and after contrast administration. It is noticeable that after contrast, a distinct tumor boundary is determined.
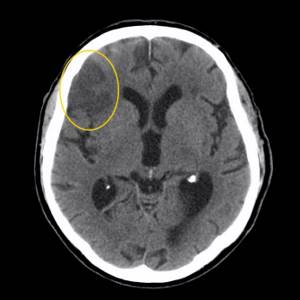
A common disorder, ischemic stroke, is characterized by the appearance of dark spots in the brain tissue. A hemorrhagic stroke, on the contrary, is distinguished by a light spot on the pictures. Consider an image of an ischemic stroke. The area of reduced tissue density in the right hemisphere is marked with an arrow.
Stages of a CT scan of the brain
Scanning is carried out as follows:
- You will need to lie horizontally on the couch.
- Doctors fix the head with fasteners to ensure maximum immobility during the examination.
- After starting the device, a series of images is created, thanks to which a three-dimensional picture of the brain appears.

Computer research is considered a painless diagnostic method. Equipment noise may be heard during a CT scan. To get rid of it and feel more comfortable in the tomograph tunnel, ask your doctor for earplugs before starting. When using a contrast enhancer, characteristic symptoms may appear:
- metallic taste;
- nausea;
- headache.
All manifestations go away on their own after completion of the procedure. Typically, testing on computer equipment takes about half an hour. The duration of the examination depends on the screening regimen and the general health of the patient. The information obtained during the CT scan is deciphered by the radiologist immediately after the completion of the session. The patient can stay in the clinic and wait for it to be drawn up for an hour.
Brain CT results
Decoding the results and preparing a conclusion takes from 1 to 1.5 hours. Also, many clinics practice sending results to the patient’s email address. The patient is given photographs and/or a CD with a recording of a three-dimensional image with detailed descriptions of them.
The patient is fine if:
- the bones of the skull, the brain and its vessels are of normal size;
- no foreign inclusions, tumors, hematomas, etc. were found;
- no symptoms of bleeding or fluid accumulation;
- the integrity of the bone tissue is not compromised.
Any deviation from the norm is considered a sign of a particular disease. Therefore, with the received conclusion, the patient is immediately sent to the doctor who prescribed the examination.
Why is a CT scan of the brain performed?
In medical organizations presented on mrt-v-msk.ru, examinations are prescribed to visualize internal organs, bones, the vascular system, as well as analyze their condition in different screening modes and projections. All this helps in detecting:
- tumors of different nature;
- assessing the prevalence and effect of therapy for cancer pathologies;
- vascular lesions;
- inflammatory foci;
- differential diagnosis of different lesions;
- acute conditions such as strokes, thromboembolism, etc.
Thanks to the use of this type of diagnosis, painful invasive procedures can be avoided.
How is a CT scan of the brain performed?
Of the large list of modern diagnostic tools, computed tomography is one of the most advanced and accurate methods, since it makes it possible to obtain a layer-by-layer image of any area under study with a slice thickness of 0.5 to 10 millimeters. From the image, you can determine the condition of the organs being examined, the extent of spread and localization of pathological processes.
No preparation is required for a CT scan of the brain. On the recommendation of the attending physician, a preliminary examination of the fundus and visual field, consultation with a neurologist, neurosurgeon, otolaryngologist, and craniography may be prescribed.
How is a CT scan of the brain performed?

A CT scan of the brain is performed on a unit located in an isolated room, where all the necessary conditions are observed. Before the procedure begins, the assistant explains how a CT scan of the brain is done and gives instructions on radiation safety and hygiene. Before entering the office, you need to remove outer clothing and all existing metal products and items. The patient lies down on a transport table and moves into the tomograph chamber. Recommendations for behavior during the examination.
The main requirement during the CT examination is to remain still. To eliminate involuntary movements, the patient's head is fixed with special soft rollers.
During the procedure, medical personnel are located in an adjacent room, maintaining contact with the patient using a built-in microphone. Apart from the noise of the operating device, nothing unusual happens. The procedure is absolutely painless. A CT scan of the brain is performed within a few minutes; with the introduction of contrast, the duration of the procedure can be increased by 15-20 minutes.
The CT scanner has an open design, so patients suffering from claustrophobia can undergo examination without any problems.
How is a brain CT scan done with contrast?

Sometimes, when performing a CT scan of the brain, the administration of a contrast agent is prescribed, which is necessary to enhance the clarity and detail of the image. The final decision on the use of the drug is made by the attending physician based on the available indications.
The administration of contrast is possible provided that the patient is not allergic to iodine-containing drugs. If you have an allergy to iodine or seafood, you must inform your doctor in advance.
Contrast drugs are usually administered intravenously, simultaneously through an injection or through a dropper. When contrast is administered, the patient may experience temporary changes in taste sensations (a metallic taste in the mouth), and a sensation of hot waves in the body may also appear. In very rare cases, nausea and headaches may occur.
Rules of behavior for the patient after the procedure
When the procedure is completed, the patient can return to normal life, that is, undergoing tomography does not limit eating, driving, or going to work. Outpatient observation is also not required.
What does a brain CT scan show?
The X-ray computed tomography method allows you to accurately and informatively determine the anatomical features and functional abnormalities in the ventricles of the brain, bones of the skull, including its base, subarachnoid space, temporal bones, and paranasal sinuses. In addition, the images obtained during the scan clearly visualize the cerebral hemispheres, brain stem, cerebellum, and also distinguish gray and white matter, cerebrospinal fluid spaces, cerebral arteries and veins - more than 200 structures in total.
CT scan of the brain: what does the study show?
In terms of information content, CT is almost no different from the alternative research method - MRI, with the exception of visualization of pituitary microadenomas, gliosis and mild disorders in the white matter. Therefore, these two methods can be used as complementary and provide the most complete picture of the pathology.
What does a brain CT scan reveal? A brain CT scan shows with a high degree of reliability and information content the following disorders:
- consequences of a head injury, including fractures of the base of the skull, cerebral edema, and in the case of traumatic brain injury, CT is the only diagnostic method, since pathological changes are noticeable in the images already 6 hours after the incident;
- atrophy of the medulla;
- hydrocephalus, CT allows you to determine the type of disease;
- hemorrhagic and ischemic strokes;
- developmental anomalies;
- areas of hematomas;
- bleeding;
- degenerative brain diseases;
- metallic and non-metallic foreign bodies;
- encephalitis;
- meningitis;
- inflammatory disorders, including abscesses, empyemas, granulomas;
- hemorrhages in the brain;
- aneurysms, thrombosis, malformations and other disorders of the vascular system of the brain;
- arachnoid and cerebral (intracerebral) cysts;
- otitis, sinusitis, pathologies of the pyramids of the temporal bones;
- morphological changes in the jaws and facial skeleton;
- acute subarachnoid hemorrhage when aneurysm rupture is suspected;
- meningiomas, hemangioblastomas, ependymomas, ganglioblastomas and other neoplasms of benign and malignant nature, areas of metastases.
Computed tomography of the brain is successfully used for preoperative examination, to monitor the effectiveness of therapy, and if the patient has individual contraindications to MRI.
What is a CT scan of the brain?
Despite the fact that CT is a radiological research method, the data obtained during a CT scan is an order of magnitude more informative than the results of classical radiography, and what a CT scan of the brain determines is of great importance in an accurate and timely diagnosis.
During computed tomography, a series of black and white images are obtained in three planes:
- frontal, which is carried out along the base of the zygomatic arches through the external auditory canals;
- axial, carried out through the external auditory canals along the lower edge of the orbits and in this projection the temporal bones, jugular foramen, cranial fossae and foramen magnum are clearly visualized;
- sagittal, which divides the study area into left and right symmetrical halves.
A series of images obtained can be reconstructed into a three-dimensional picture of the brain, which makes it possible to judge the spatial location of its structures and the relationship of pathology with unchanged tissues.
CT image acquisition is based on the different densities of different tissues and structures of the brain. Therefore, pathological disorders can manifest themselves either as darkened “dense” areas, for example, in the case of a tumor, or as “clearing” areas, as in the case of cysts, or their alternation.
Some pathologies may not be accompanied by a significant change in X-ray density compared to unchanged tissue, but are manifested by a change in the size of the head structure, deformation, dilation or narrowing of blood vessels, etc.
With intravenous contrast, pathological lesions are stained more intensely than healthy areas, which helps to increase the resolution of CT.
How to interpret pathologies from CT images?
After the scan, the doctor compares the resulting images with normal indicators of the condition of the skull and brain, and evaluates the speed of blood flow. The specialist also pays attention to the presence of foreign bodies, signs of fluid accumulation, and disruption of the structure of nerve fibers.
One of the common diseases - ischemic stroke - is visualized by dark spots on the brain tissue, hemorrhagic stroke is determined by white spots on CT images of the brain, as shown in the photo below.
The images also distinguish cystic formations from tumors - during a contrast study, a tumor neoplasm, unlike a cyst, accumulates contrast and appears more clearly in the images.
Note that the diagnosis of tumors is based on identifying direct (shadow of the formation) and indirect signs (swelling of brain tissue, hydrocephalus, etc.). Some features, such as areas of brain tissue with high density, are detected only if a contrast agent is injected. Also, many large formations or located deep in the brain are diagnosed by expansion, compression or displacement of the cerebral ventricles.
The patient does not have any brain disorders if the brain itself, blood vessels, and skull bones are of normal size, there are no symptoms of bleeding, there are no accumulations of fluid, the integrity of the bone tissue of the skull is not compromised, there are no neoplasms, damage to nerve fibers, enlargement or expansion of the ventricles of the brain and other signs of disease.
Only a radiologist should interpret the images, but not the patient himself, since interpretation of the results is a complex process, and incorrect interpretation of the data can lead to an incorrect diagnosis and lack of correct treatment.