X-rays of the hip joint are now useful not only in older patients in whom osteoarthritis or osteoarthritis of the joint is suspected, but also in younger patients.
Young people often come to the radiologist's office without osteoarthritis, but (unless there is a clearly defined problem) they are examined for femoroacetabular impingement or hip dysplasia.
A simple x-ray can evaluate both a normal and a dysplastic hip joint, or those with signs of damage.
In addition, pathological processes such as osteoarthritis, infections or tumors may be detected.
What is x-ray diagnostics
X-ray diagnostics is based on special X-rays that the device emits. Soft tissues allow them to pass through, while hard tissues absorb them, which is why in the picture the former are painted dark, and the latter light. Bone tissue is most clearly visible in the photographs, so the method is used to examine the condition of bones and joints. The results are provided on paper or digital media and saved on the computer’s hard drive.
Today you can get an X-ray image on digital media
How is it carried out?
X-rays are performed without preparation. The patient is positioned on a special table. The groin area is protected from irradiation with a lead apron. For children, protection is applied to the eye and thyroid area, while in infants, only the area being examined, such as a limb, is left exposed.
The doctor takes a picture in one or several projections. To make them clear, you need to remain motionless. The specialist independently determines the optimal projection depending on the segment being studied: straight, lateral or a combined option.
If the patient is overweight, the image may not be clear
Preparation
- If you need to have an x-ray of your hip joint, no special preparation is usually required, but it is still worth paying attention to certain points.
- Since the area of interest is quite close to the intestine, its contents may affect image quality. In particular, this concerns the process of gas formation. To remove intestinal contents, it is recommended to perform a cleansing enema the evening before the test and the next morning. The patient can also take any laxative before the procedure.
- If radiography is performed with a contrast agent, it is necessary to conduct a test in advance to determine an allergic reaction. The procedure is carried out if the result is negative.
Is it dangerous
X-rays are often prescribed not only at the diagnostic stage, but also during the treatment of arthrosis of the knee, hip or other joint. Many fear that radiation will harm the body and trigger irreversible processes in it, for example, the degeneration of cells into malignant ones, and weaken the already weak immunity of an elderly person. Is it possible to take x-rays often?
The harm from radiation on modern devices is minimal if all safety rules are followed. The dose of radiation is comparable to that which we receive daily from television or while flying on an airplane. Therefore, you should not refuse the examination if the doctor insists. The main thing is to take precautions.
How dangerous is x-ray and who is strictly contraindicated to undergo this examination? The answers are in the video below:
Restrictions
X-rays are not performed on children under three months of age, who are prescribed an ultrasound if necessary. Doctors also do not recommend excessively irradiating infants in the pelvic area, as this can lead to infertility, blood disease, and a tumor process in the future. Children are examined strictly according to indications and in a standardized manner, no more than once every six months.
X-rays are not performed on pregnant women to avoid negative effects on the fetus. It is also contraindicated in people with metal prosthetics or implants in the area being examined and in people with schizophrenia (and other mental disorders) who are unable to remain still. Other people, including older people, can undergo the examination.
Contraindications
It is not recommended to do an x-ray of the hip joint if:
- Pregnancy or lactation - radiation, although at a safe dose, can disrupt the intrauterine development of the fetus or lead to cessation of lactation.
- The patient is under 15 years of age (period of active growth).
- The patient is in serious condition – heavy blood loss, painful shock.
- Repeated X-rays taken within the previous year or several months.
There may also be a risk of using a contrast agent during x-rays. It is based on iodine, which is not advisable for diseases of the thyroid gland, allergies to iodine, severe renal and liver failure, and severe diabetes mellitus.
What does an ankle x-ray show?
The ankle suffers very often, since the feet take on the maximum load when walking upright. X-rays of this joint are usually taken in three projections, with or without load: lateral, oblique, and x-ray of the heel bone. Sometimes, to clarify the diagnosis and assess the condition of soft tissues, CT or MRI are additionally prescribed.
X-ray allows you to diagnose:
- injuries;
- ankle arthrosis;
- arthritis, synovitis, gout;
- congenital anatomical disorders;
- osteophytes – heel spurs;
- flat feet;
- metabolic disorders, etc.
X-ray image shows the condition of the foot bones well
How informative is a knee x-ray?
In the case of the knee, this examination is prescribed for any damage and injury, pain at rest and movement. Other indications include swelling, changes in skin color, deformities and limited mobility, symptoms that often accompany arthrosis.
X-rays of the knee have the greatest diagnostic value for injuries - bone cracks, fractures, dislocations and subluxations of joints. He diagnoses condyle fractures, meniscus and patella injuries, and hemorrhages in the knee joint. The method allows you to examine the joint and adjacent areas - fibula, femur and tibia. With its help, you can identify arthrosis, arthritis and osteoporosis, and then continue the examination with other methods.
MRI is often used along with X-rays to diagnose the knee joint.
Comparison with MRI and ultrasound
Sometimes ultrasound is used to diagnose joint pathology. The studies are diametrically opposed, since radiography helps to identify bone pathologies, while ultrasound helps to identify soft tissue diseases.
X-rays look at the anatomical structure, while ultrasound reveals functional deficits, such as insufficient or excessive amounts of intra-articular fluid. Often, for the most complete picture of the disease, a joint appointment of studies is required.
Tomographic examination is a relatively new method, compared to conventional x-rays, which is much more informative. The main advantage of X-rays compared to MRI is its general availability, since the machines are present in every hospital, and its low cost, since MRI is much more expensive.
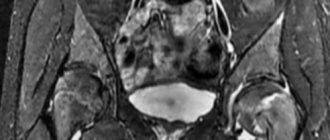
MRI
In what cases is a hip x-ray prescribed?
The hip joints are one of the most complex joints in the body. The patient is sent for an x-ray if he experiences discomfort when moving and has limited mobility. If the joint is painful or deformed, as well as after any injury.
Using radiography, you can identify the following diseases and pathologies:
- congenital dislocation and dysplasia of the hip joint;
- acquired dislocations and fractures (relevant for older people suffering from coxarthrosis);
- primary tumors, metastases of cancer of another location;
- osteoporosis, necrosis of the head of the femur;
- inflammation in the joint;
- arthrosis and other pathological changes.
Unlike other areas, before an x-ray of the hip joint, the patient may be advised to do a cleansing enema or take a laxative the day before. This is done to ensure that there are no shadows in the image due to a full intestine.
X-ray of the hip joint allows diagnosing coxarthrosis
The process of deciphering survey results
After the radiologist receives the X-ray images, he needs to interpret them and draw up a conclusion.

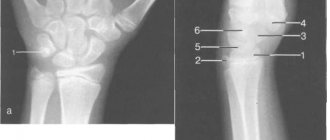
To decipher the results, there is a special technique called the Hilgenreiner scheme. It contains the following categories:
- acetabular angle;
- Hilgenreiner line;
- the distance between the metaphyseal plates and the Hilgenreiner line, denoted by the letter h;
- the distance from h to the lower contours of the vestibular plate, denoted as d.
The acetabular angle is defined as the area between two planes - the line of epsilon-shaped cartilages and the tangent running along the edge of the glenoid sockets.
Hilgenreiner's line is drawn horizontally through the Y-shaped cartilages along the lower points of the ilium.
Distance h is measured from the Hilgenreiner line to the middle of the metaphyseal plate of the proximal femur. It can be used to track how much the head of the femur is displaced in relation to the socket of the joint.
The d gap shows the lateral displacement of the head compared to the acetabulum.
The diagram makes it possible to represent the joint in a three-dimensional projection. Even at the earliest stages, it makes it possible to detect most pathologies and disorders of joint development.
For greater reliability, the scheme provides for additional indicators - the Calvet and Shenton lines. The first of them connects the upper edge of the femoral neck with the outer edge of the ilium, and normally it should be continuous. If the line is interrupted, this may indicate a lack of integrity of the articular apparatus.
Shenton's line is a continuation of the circumference of the acetabulum, in the form of a projection onto the medial surface of the femoral neck. Its rupture means lateral-proximal displacement of the femur.
There are also auxiliary schemes for deciphering radiographs of the joint in children - the Reinberg scheme and the Ombredan scheme.
How is an X-ray of a child’s hip joint interpreted using the Reinberg scheme?
This image interpretation technique uses the midsacral line, a horizontal line through the apices of the Y-shaped cartilages and the centers of the ossification nuclei in the femoral heads (line A), and a vertical line through the superolateral prominence of the acetabulum (line B) . In addition, determining the normal condition of the joint is associated with the location of the lower edge of the femoral neck - with normal development of the joint, it crosses the lower contour of the groin bone.

An auxiliary line B1 is drawn between line B and the median sacral line, the length of which helps to assess the condition of the joint.
Dysplasia is determined if the proximal end of the femur is above line A and as if outside of plane B.
What is the Ombredan scheme?
In the process of examining the results of radiography, the doctor draws a horizontal line along the synostoses in the image, connecting the pubic and ilium bones. A vertically lowered perpendicular is drawn to the outer edge of the acetabulum of the joint. This perpendicular divides the articular cavity into equal segments, in relation to which the compliance of the anatomy of the joint with normal indicators is assessed.
Normal and deviations in the image of the hip joints
The resulting image of the joint, if it is in a normal state, visualizes the head of the femur located in the glenoid cavity, which has the appearance of a notch. In the center, the head is attached to the surface of the cavity by the round ligament and joint capsule. From above, the head is held in its normal position by the limbus, a cartilaginous plate. The entire articular apparatus is supported externally by the muscular corset of the thigh.
Dysplasia in the image is characterized by a delay in the development of ossification. Ossification nuclei are small in size compared to normal. Dislocation or subluxation can be detected by the lateral and vertical displacement of these nuclei, thanks to the use of Ombredan, Reinberg, and Hilgenreiner schemes.
Features of x-ray of the upper extremities
X-rays of the elbow are also prescribed after injuries - severe bruises, dislocations, fractures - or if various pathologies are suspected. It allows you to obtain information about the joint space and its narrowing, about the condition of the ends of the bones of the humerus and forearm. The specialist also receives data about the areas adjacent to the elbow joint, which facilitates diagnosis. After all, the cause of pain is not always arthrosis of the elbow, arthritis or bursitis: it often has a spreading nature and a completely different source.
Shoulder pain often occurs against the background of neurological and vascular diseases, but the cause may also be shoulder arthrosis, as well as systemic inflammatory diseases of the shoulder joint. X-rays are mainly prescribed if a dislocation or fracture is suspected. The image also shows adjacent formations - the collarbones and shoulder blades. It is also informative for arthrosis and arthritis, necrosis of the humeral heads, tendonitis and other diseases.
Osteoarthritis of the upper extremities is often discovered by chance on an X-ray
X-ray is a simple, quick, painless diagnostic method that provides information about the condition of bones and joints. When arthrosis is detected, additional instrumental methods are often prescribed to examine the deep structures of soft tissues and study the condition of the cartilage. However, MRI and CT scans are expensive and not always necessary. Therefore, if the orthopedist insists on an x-ray, you should not refuse.