Magnetic resonance imaging (MRI) is a non-invasive diagnostic method that allows you to establish a diagnosis with maximum accuracy and develop an effective treatment regimen.
To visualize the brain and its detailed examination, exposure to powerful magnetic fields and high-frequency pulses is used. The computer program then processes the results obtained and produces information in the form of a picture that can be transferred to paper or electronic media.
The procedure is completely painless and safe for humans. During an MRI scan, the patient is not exposed to x-rays. The examination can be carried out repeatedly, even for children over 3 years of age and senior citizens. Using MRI, it is possible to detect a variety of brain diseases in the early stages of development, which is the key to their successful treatment in the future.
Indications
The resulting layer-by-layer images of brain structures allow specialists to study in detail the condition of tissues and blood vessels, identify the pathological focus, its location, shape, size, assess the degree of prevalence, etc.
No other diagnostic method (radiography, ultrasound or computed tomography) provides as much information and in such a volume as MRI.
You can undergo the examination yourself or as prescribed by a neurologist in the following conditions:
- constant (frequent) headaches, dizziness;
- suspected brain tumor (regardless of malignancy);
- examination before brain surgery;
- assessment of the condition of structures and meninges after surgical treatment;
- infectious diseases (encephalitis, meningitis);
- decreased vision and hearing not associated with eye or inner ear disease;
- acute cerebrovascular accidents (stroke);
- neurological disorders (frequent fainting);
- pathological changes in blood vessels (aneurysm, stenosis);
- diseases of the nerves (auditory, visual);
- deterioration of memory, concentration;
- congenital malformations of the brain;
- diffuse (extensive) changes (Alzheimer's disease, multiple sclerosis);
- epilepsy (including post-alcohol epilepsy);
- various injuries;
- monitoring (control) of the condition of the cancer site after treatment;
- inability to perform a computed tomography scan.
In addition to the above conditions, children are also prescribed MRI in the following cases:
- delay in psychomotor development;
- speech disorders (stuttering);
- inappropriate behavior in everyday life and society without justified reasons;
- convulsive syndrome;
- frequent fainting conditions.
Contraindications
The procedure is based on the effect of magnetic fields, so MRI is strictly prohibited for people with pacemakers, ferromagnetic endoprostheses, metal staples on brain vessels, electronic implants in the middle ear, and foreign objects (metal fragments) in the tissues of the eye. The presence of these objects can affect the examination result, and the magnetic field, in turn, can disrupt the operation of, for example, a pacemaker. It is also not possible to perform an MRI on people who are overweight (the diameter of the MRI capsule tunnel is 60 cm).
Relative contraindications (conditions in which MRI is considered possible):
- pregnancy (first trimester);
- claustrophobia (fear of closed spaces);
- wearing braces and dental crowns;
- using an insulin pump;
- tattoos with paint containing iron;
- metal foreign objects not localized in the head area.
What is MRI?
Magnetic resonance imaging is a diagnosis based on a magnetic field and radio frequency waves. The information obtained during the study is processed by a computer, which converts it into a 3D image. MRI has proven effective in detecting pathologies that cannot be detected with other types of examination.
Like the previous type of examination, this procedure requires preliminary preparation. You can’t eat on the eve of it. The last meal should be approximately 6 hours before the MRI. Drinking plenty of fluids is also necessary. Before the procedure itself, all metal objects and cosmetics are removed from patients.
How is an MRI performed?
Before the examination itself, the patient is placed on a couch, which is pushed into the tomograph and the examination begins. The procedure is comfortable for the patient, and he will only hear loud noise.
Types of MRI
Depending on the part of the body or organ being examined, the following types of MRI are distinguished:
- vascular angiography;
- examination of the spine, brain, abdominal cavity or all organs simultaneously.
Indications for MRI
This procedure is prescribed for the diagnosis of almost all systems and organs of the human body. It is prescribed when it is necessary to draw up an informative clinical picture.
Contraindications for MRI
Despite the fact that MRI is considered a safe diagnosis, not everyone can undergo the study. This diagnosis cannot be carried out in the following cases: with renal failure, pregnancy, claustrophobia and psycho-emotional disorders, as well as with a pacemaker.
Preparation
MRI is not time-sensitive and can be performed both in the morning and in the afternoon/evening hours. No special preparation is required. The patient only needs to have identification documents (passport), a referral from a doctor and the results of previous examinations, if any.
Eating and taking medications before the procedure is not prohibited. If claustrophobia is present, the patient is given light sedation (injection of a sedative) immediately before the examination.
Brain MRI technique

The examination can be carried out both on an outpatient basis and in a hospital setting. The duration of the procedure is from 15 minutes to half an hour.
The patient is placed on the sliding table of the MRI unit. To ensure complete immobility, the patient’s body is fixed with bolsters and belts, and the head is fixed with special clamps.
If it is necessary to administer a contrast agent (for more effective visualization of the structures being examined), the nurse installs an intravenous catheter for the patient.
Important! The administered substance is absolutely safe and does not in any way affect the health and well-being of the patient.
After this, the table, together with the patient, slides inside the magnetic capsule, and the medical staff leaves the office. A two-way communication system involves communication between the doctor and the patient. At certain moments the doctor may ask you to hold your breath or inquire about the well-being of the person being examined. The patient, in turn, reports all his sensations and changes in health status by pressing the button to turn on the intercom inside the capsule.
At the end of the study, the patient is released from the fixing devices, the intravenous catheter is removed and asked to wait for a while outside the office doors while the doctor performs a preliminary analysis of the images. If poor quality images are obtained, the procedure may need to be repeated.
Indications for magnetic resonance imaging
Symptoms that require an MRI of the lumbar spine:
- backache;
- increased temperature during periods of pain;
- numbness or weakness in the legs;
- instability of the bladder.
Most diseases are identified by the listed symptoms even at an early stage, when treatment is most effective. If surgery is necessary, MRI of the spinal cord or other components is performed twice: before surgery and after (to confirm the results and monitor recovery).
Is MRI dangerous for the body?
MRI is one of the safest diagnostic techniques, as there are no harmful radiations. It is even used on small children.
And you won’t be bored – in most cases the procedure will take 30 minutes. During this time, the doctor is in direct access, monitoring the operation of the device and the patient’s condition.
Possible complications during and after MRI
To date, no complications have been observed after MRI of the brain. During the procedure, the patient may experience psychological discomfort from being in a confined space. This condition is easily eliminated by pre-administration of sedatives.
Children are required to be provided with headphones or earplugs to drown out the noise of the operating scanner. Adult patients usually request them themselves. In some clinics, light music is played for the patient to create a favorable atmosphere inside the capsule.
At the moment the contrast agent is injected into the vein, the patient may feel a rush of heat or, conversely, a feeling of cold flowing through the veins. Some people experience an iron taste in their mouth. This is a normal reaction and there is no need to worry about it.
During insertion and removal of an intravenous catheter, the subject feels physical discomfort, the same as when an injection into a vein. But all this is survivable and does not require special treatment. Even a small hematoma at the puncture site will resolve on its own in a few days, leaving no mark on the skin.
It is possible that the temperature of the area of the body under study may increase; with MRI of the brain, the head. This is also only a temporary effect that will not cause harm to health. But if this causes great concern to the patient, he is simply obliged to inform the doctor about his condition.
There is also a small risk of developing an allergic reaction (hives or itchy eyes) or nausea after contrast injection. In this case, the medical staff of the MRI room will immediately provide the necessary medical assistance.
Alternative Methods
Magnetic resonance imaging has left radiography and ultrasound far behind in terms of information content and accuracy of results. Only computed tomography (CT) can compete with MRI. But there are significant differences between the two modern diagnostic methods.
- MRI is good at identifying the pathology of soft tissues and blood vessels of the brain, CT scans at the bone structures of the skull and cavities filled with cerebrospinal fluid (CSF);
- MRI does not carry radiation, CT uses radioactive radiation;
- The quality of MRI images is much better, since they are not subject to the shielding effect of the skull bones, as with CT;
- Gadolinium-based MRI contrast is much less likely to cause allergic reactions than iodine-based CT contrast.
Despite the abundance of advantages, MRI is not always indicated for everyone. Therefore, computed tomography, as well as other, slightly outdated, research methods are widely used as an alternative method in modern diagnostics.
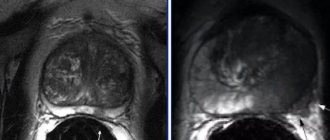
How many patients with a normal MRI have prostate cancer?
V.V. Khvorov, Ya.I. Potapov GBUZ MO "Mytishchi City Clinical Hospital"; Russia, Moscow region, 141009 Mytishchi, st. Comintern, 24
Introduction
Currently, there is growing interest in multiparametric magnetic resonance imaging (MRI) as a method for diagnosing clinically significant prostate cancer (PCa), used after negative results of the first biopsy [1]. As an alternative approach, multiparametric MRI is considered before biopsy in those patients for whom it is indicated according to standard criteria [2, 3]. Recent studies have shown impressive results using multiparametric MRI in the diagnosis of clinically significant prostate cancer [4, 5]. In addition, awareness of Russian patients about the possibilities of MRI and the refusal of Western medicine to screen for prostate cancer based on measuring the level of prostate-specific antigen (PSA) is growing. Our study aims to determine how many cases of prostate cancer we would miss (and how many of them are clinically significant) if we relied only on multiparametric MRI results; that is, to determine its sensitivity in real clinical practice.
Materials and methods
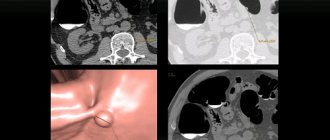
The study involved men over 40 years of age referred for suspected prostate cancer to the clinical diagnostic center of the Mytishchi City Clinical Hospital in 2016–2017. Indications for biopsy were considered to be a PSA level >4 ng/ml (up to 60 years of age >2.5 ng/ml) with 2 measurements or the presence of a solid lesion identified by digital rectal examination in combination with a PSA level >2 ng/ml. The reasons for first PSA measurement or digital rectal examination (lower urinary tract symptoms, spontaneous screening, or diagnosis of rectal pathology) were not included. In some patients, multiparametric MRI was performed before referral to the clinical diagnostic center. In the absence of previous MRI results, in patients without obvious manifestations of metastatic PCa theoretically suitable for radical treatment, we recommended that multiparametric MRI be performed before biopsy. If the patient had indications for a biopsy according to standard criteria, it was performed regardless of the presence of an MRI report.
From January 1, 2021 to December 31, 2021, 412 prostate biopsies were performed in 401 patients in the urology department of the Mytishchi City Clinical Hospital. The biopsy was performed through a transrectal approach; samples were collected from at least 12 different locations. Of all the patients for whom the first pancreatic biopsy was indicated, multiparametric MRI of the pelvis was performed in 249. Scanning with a device of at least 1 T was considered valid if there was a conclusion with a gradation according to the PI-RADS v scale. 2 (Prostate Imaging Reporting and Data System, version 2, prostate imaging system, version 2) [6] and a CD with recorded images if the MRI was not performed at our institution.
Version 2 of the PI-RADS scale was introduced in 2015 and has become widely accepted as a useful predictive tool for assessing focal changes in the pancreas. The system is based on assessing the degree of signal reduction from a lesion in the pancreas (from 1 to 5) during a sequential study of all MRI modes. The MRI result was considered negative if the score was <3 on the PI-RADS v scale. 2, while in the primary analysis we relied on the existing opinion of the radiologist, without re-analysis of the images by the reference specialist. Based on the biopsy results, clinically significant prostate cancer was defined as prognostic group 2 or higher according to the criteria of the International Society of Urological Pathology (2014).
results
Of the 249 patients admitted to the department for an initial prostate biopsy, the results of a previously performed MRI were negative in 174. In other words, in the majority (70%) of patients, prostate cancer was not detected on MRI before receiving the biopsy result.
In 117 out of 249 patients, prostate cancer was detected by biopsy. Of the 117 patients diagnosed with prostate cancer, MRI results were negative in 46 (40%). Of these patients, clinically significant prostate cancer was diagnosed in 23 (20%) (Fig. 1).
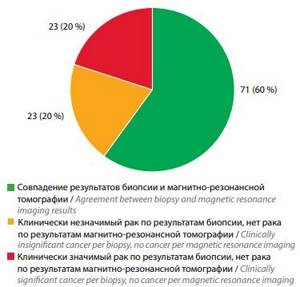
Rice. 1. Probability of negative magnetic resonance imaging results for prostate cancer
Of the 174 patients with negative pre-biopsy MRI findings, PCa was detected in 46 (26%) and clinically significant PCa in 23 (13%) (Fig. 2).
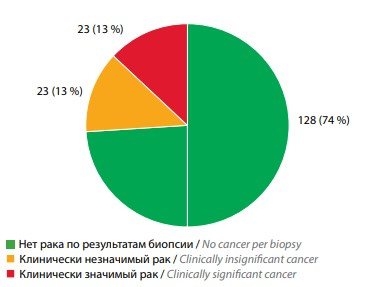
Rice. 2. Probability of prostate cancer if magnetic resonance imaging is negative before biopsy
Discussion
“Doctor, my PSA is slightly elevated, but according to the MRI there are no signs of cancer. I feel great. Do I really need a prostate biopsy? There are more and more patients asking this question. In the absence of mass PSA screening in Russia, we, in fact, perform it on patients who come to us with symptoms of the lower urinary tract. “Where is your PSA test?” - this is where we now begin examining such a patient. On the other hand, many patients have heard about the abolition of PSA screening in Western countries, but, not being specialists, may misperceive this information as an absolute lack of need for PSA testing. Finally, the widespread development of private diagnostic medicine allows patients to independently undergo pelvic MRI without a doctor’s prescription.
Having the data from our study, we can quite specifically answer the patient’s question about the advisability of a biopsy in case of elevated PSA and negative MRI results. We find prostate cancer in every 4th patient, and clinically significant prostate cancer in 13% of cases. The patient has the right to weigh his own risks and make an informed decision.
To be fair, it is worth noting that of the 23 patients with clinically significant prostate cancer and negative MRI, the majority (n = 19) were in prognostic group 2, and only 4 in group 3. However, this conclusion is based only on biopsy data, and an increase in the score on the scale Gleason in pathohistological examination after prostatectomy is a known phenomenon.
Limitations of our study include its retrospective nature, small number of observations, and lack of expert opinion on MRI. However, the latter reflects real clinical practice as closely as possible.
conclusions
Among patients who are indicated for a primary biopsy of the prostate according to standard criteria, with a normal MRI picture, clinically significant prostate cancer was detected in 13% of cases.
Literature
- Kossov F.A., Chernyaev V.A., Akhverdieva G.I. and others. The role and significance of multiparametric magnetic resonance imaging in the diagnosis of prostate cancer. Oncourology 2017;13(1):122–33. . DOI: 10.17650/1726-9776-2017-13-1-122-133.
- Moldovan PC, Van den Broeck T., Sylvester R. et al. What is the negative predictive value of multiparametric magnetic resonance imaging in excluding prostate cancer at biopsy? A systematic review and meta-analysis from the European Association of Urology Prostate Cancer Guidelines Panel. Eur Urol 2017;72(2):250–66. DOI: 10.1016/j. eurouro.2017.02.026. PMID: 28336078.
- Delongchamps NB, Zerbib M. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. Eur Urol 2012;61(3):622–3. DOI: 10.1016/j. eurouro.2011.12.038. PMID: 22289974.
- Filson CP, Natarajan S, Margolis DJ et al. Prostate cancer detection with magnetic resonance-ultrasound fusion biopsy: the role of systematic and targeted biopsies. Cancer 2016;122(6):884–92. DOI: 10.1002/cncr.29874. PMID: 26749141.
- De Rooij M, Hamoen EH, Fütterer JJ et al. Accuracy of multiparametric MRI for prostate cancer detection: a metaanalysis. AJR Am J Roentgenol 2014;202(2):343–51. DOI: 10.2214/AJR. 13.11046. PMID: 24450675.
- Weinreb JC, Barentsz JO, Choyke PL et al. PI-RADS prostate imaging – reporting and data system: 2015, version 2. Eur Urol 2016;69(1):16–40. DOI: 10.1016/j.eururo.2015.08.052. PMID: 26427566.
The article was published in the journal “Andrology and Genital Surgery”, issue No. 4 2021, pp. 67-69
Topics and tags
Prostate cancer
Magazine
Andrology and genital surgery 2021 No. 4
Comments
To post comments you must log in or register