False positive reaction to syphilis
Today, a false positive result is quite often observed when identifying treponema pallidum.
It is known that syphilis is a very serious and dangerous disease that is difficult to cure.
Despite advances in medical technology, syphilis remains a disease that frightens many patients and doctors.
Receiving a positive test makes you panic.
It should be taken into account that a false positive result is possible.
There are cases when, after contact with a patient, infection does not occur.
The main reason for this phenomenon is the small amount of treponema in the infectious material.
Laboratory tests help detect syphilis.
The leading diagnostic methods include serological studies.
These types of tests show the presence of antibodies in the blood serum.
There are two types of serological testing.
This can be treponemal or non-treponemal analysis.
Non-treponemal studies include the Wasserman reaction.
This reaction is based on associating a compliment.
Treponemal analysis is usually performed to confirm the diagnosis.
This research method is suitable if the non-treponemal test gives a false positive result.
The treponemal test is not as sensitive as the RW test.
This type of analysis is expensive and requires special laboratory equipment.
What is a false positive result?
A false positive occurs when a diagnostic test is positive when there is no disease present.
This result may appear in several cases.
One of them is oncology or the presence of infectious processes in the body.
In addition, a false response to syphilis is possible during pregnancy.
An enzyme-linked immunosorbent assay is used to make an accurate diagnosis.
This is a new diagnostic research method that eliminates false results.
Note! If you suspect syphilis, you should visit a specialist. He will conduct an examination and give a referral for laboratory diagnostics.
When you first visit the clinic, nonspecific research methods are most often prescribed.
If the result is doubtful, specific tests are performed.
There is no pathological process, both tests showed positive results.
What to do in this situation?
Remember! The result of any test is not a diagnosis.
Serological tests are aimed at detecting antibodies.
As is known, the immune system is capable of provoking the production of immunoglobulins for other infectious diseases.
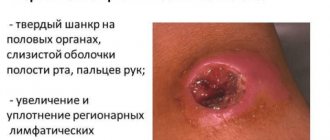
Diagnosis of syphilis can give a false positive result:
- 1. For allergies
- 2.After suffering from syphilis
- 3. For a cold
- 4.For autoimmune diseases
- 5. For antiphospholipid syndrome
All of the above reasons may affect the reliability of the result.
How else can you confirm the presence of infection?
Diagnostics can be carried out using PCR testing.
It is usually used after serology.
You can perform these tests simultaneously.
In the absence of symptoms of syphilis, it is used as an additional test.
This type of diagnosis is aimed at determining the DNA of the pathogen in pathological material.
After a comprehensive study, an accurate diagnosis can be made.
Sometimes this diagnostic method is not able to give a reliable answer.
A questionable result is possible if the patient has a chronic disease.
Remember! If the result for syphilis is positive, you should be tested again.
If the result is positive again, it is recommended to undergo a full examination to clarify the reasons for this result.
Timely diagnosis will allow you to prescribe an effective course of therapy and avoid complications.
It must be remembered that syphilis is highly treatable at the first stage.
Modern diagnostic methods today make it possible to detect the disease, even in the absence of clinical symptoms.
You should regularly undergo preventive medical examinations, including tests for syphilis.
Is a person infected with a false positive test?
A false positive result does not indicate the presence of syphilis.
Such a reaction can cause any other infectious process.
You should undergo an examination to determine an accurate diagnosis.
Errors in diagnosing syphilis in the practice of doctors of various specialties
Syphilis is a socially significant infection from the group of sexually transmitted diseases, and is characterized by a long course, systemic lesions, and the ability to lead to irreversible damage to internal organs and the nervous system, disability and death. The high incidence rate and clinical diversity of manifestations observed in recent years indicate the undoubted relevance of the problem and determine the control of syphilitic infection as a priority in global health [1–4].
One of the serious issues of syphilidology, requiring special attention, study and attitude, has been and remains diagnostic errors. They contribute to the spread of infection, the development of severe, often disabling lesions of the patient’s internal organs and nervous system, and make it difficult to control the epidemiological situation [2–7]. According to Russian authors, the frequency of diagnostic errors in syphilis is about 30% in relation to the number of registered patients, with the majority (84.5–99.7%) occurring in early forms of the disease [8–11]. The most common errors are made by obstetrician-gynecologists (22.5–35.3%), therapists (20–35.3%), and dermatovenerologists (14–24%), which is explained by the more frequent visits of patients to these specialists. Especially many mistakes are made in relation to patients with extragenital location of syphilides, specific lesions of internal organs and the central nervous system (CNS), and the presence of other sexually transmitted infections (STIs) [3, 7, 12–15].
Materials and research methods
A structural analysis of diagnostic errors was carried out based on the observation of 387 patients with early manifest syphilis and 108 patients with a latent form of the disease. The examination complex included direct detection of Treponema pallidum using dark-field microscopy; microprecipitation reaction (MPR); immunofluorescence reaction (RIF) in modifications: RIF-abs (RIF with absorption) and RIF-200 (the test serum is diluted 200 times before the reaction); enzyme immunoassay (ELISA); passive hemagglutination reaction (RPHA). To diagnose STIs, microscopy, culture, passive immunofluorescence (PIF), polymerase chain reaction (PCR), and amine test were used. Statistical, mathematical and graphical processing of the obtained data was carried out using the statistical software package Statistica 6.0, Biostat, Microsoft Office Excel 2007 and Microsoft Office Word 2007.
Results and its discussion
According to our data, diagnostic errors were made in 39 (10.8%) of 387 patients with early manifest syphilis. Moreover, in relation to the named 39 patients, 47 diagnostic errors were made: 12 by dermatovenerologists, 9 by obstetricians-gynecologists, 8 each by surgeons and therapists, 3 by otolaryngologists, 2 by urologists, 1 each by an oncologist, a phthisiatrician, a pediatrician, a proctologist, and an ophthalmologist. After misdiagnoses, 24 patients received various types of local and systemic therapy. Inadequate treatment lengthened the diagnostic route and in 3 cases worsened the patients' condition in the form of a complication of contact dermatitis. 2 patients underwent unnecessary surgical intervention (foreskin circumcision and laparoscopy).
Of the 12 patients with syphilis who turned to dermatovenerologists, in 3 cases the diagnosis was made: pyoderma, 2 each - scabies and alopecia, 1 each - mycosis of the feet, rectal fissure, allergic dermatitis, herpes, lichen planus.
When contacting doctors of other specialties (27 patients), the following diagnoses were put forward as erroneous: submandibular lymphadenitis, acute respiratory diseases, pyoderma, herpes, hemorrhoids, colpitis, rectal fissure, adnexitis, influenza, phimosis, trichomoniasis, ectopic pregnancy, urticaria, inguinal dermatitis, sore throat, sulfur plug, uveitis, cystitis, candidiasis, chronic bronchitis.
It should be noted that quite often the manifestations of the disease were missed due to the negligence of specialists: incomplete examination (25.7%) and failure to carry out rapid laboratory diagnosis of syphilis (18.3%). However, in the majority of patients (56.0%), the errors were the result of insufficient knowledge of the clinic of syphilis. Moreover, in 72.5% of cases, experts incorrectly interpreted its clinical manifestations. Extragenital chancre was regarded as pyoderma, rectal fissure, or herpes. Inguinal lymphadenitis was defined by gynecologists as adnexitis and even ectopic pregnancy. Patients with prodromal symptoms were diagnosed with acute respiratory infections and influenza. Erosive papules were mistaken for herpes, inguinal dermatitis, roseola rash - for urticaria. In 27.5% of cases, syphilides were positioned as symptoms of banal inflammation: submandibular lymphadenitis, tonsillitis, phimosis, uveitis.
A comparative analysis of the frequency of recording diagnostic errors in different groups revealed a significant predominance (p < 0.05) of patients with extragenital localization of hard chancre (table). It should be noted that 3 out of 7 errors were made by dermatovenerologists.
As examples, we provide observations from our own practice.
Patient M., 18 years old, applied for an outpatient appointment with a dermatovenerologist due to the appearance of an ulcer on the chin. After a negative rapid examination for syphilis (treponema pallidum was not detected twice, MRP was negative), streptococcal ecthyma was diagnosed and local antibacterial therapy was prescribed, which had no positive effect. A spotty rash that appeared on the skin of the torso 6 weeks later forced M. to go to the clinic of another dermatovenerological dispensary, where upon examination a scarring ulcer on the chin, a profuse roseola rash on the skin of the torso, submandibular and axillary lymphadenitis were discovered. After soaking with saline solution, treponema pallidum was found in the ulcer discharge; serological tests for syphilis were positive. Based on the above, the patient was diagnosed with secondary syphilis of the skin and mucous membranes.
Patient G., 45 years old, noticing erosion on the lower lip, went to the dermatovenerological dispensary (VD), where he was examined for treponema pallidum and rapid diagnosis of syphilis with a negative result. A diagnosis was made: herpes of the lower lip, and antiviral ointment was prescribed. After 3 weeks, due to the enlargement of the submandibular lymph glands against the background of non-healing erosion, G. turned to an oncologist, who performed a puncture of the node and prescribed parenteral antibiotic therapy, after which the body temperature increased to 39.0 ° C, a rash appeared on the torso and abdominal pain . The patient was hospitalized in the surgical department, he underwent diagnostic laparoscopy and routine examination for syphilis. After receiving positive results, the patient was transferred to the skin and venereal disease hospital. On the day of admission, he had remnants of a hard chancre on the lower lip, a roseola rash on the chest and abdomen, and polyadenitis. Secondary syphilis of the skin and mucous membranes was diagnosed, and specific therapy was carried out.
In both cases, the non-sexual localization of example-affects entailed a violation of the standard examination of patients for syphilis: repeated sampling of material from the pathological focus until its complete epithelization or scarring using a lotion with an isotonic solution. Serological examination was limited to screening tests. The recommended clinical and serological observation was not carried out within 2 months from the date of presentation.
Patient P., 36 years old, went to the KVD clinic with complaints of the appearance of a “sore” on the back of his right hand. A dermatovenerologist diagnosed the patient with pyoderma; local treatment with syntomycin emulsion was prescribed; rapid testing for syphilis was not performed. A week later it turned out that P. was the sexual partner of a patient with secondary syphilis. On re-examination, treponema pallidum was found in the discharge from the lesion; serological tests were positive. Diagnosis: primary syphilis of other localizations. Violation of the regulated examination of an outpatient for syphilis was the reason for the late diagnosis of the disease.
As presented in the table, patients with concomitant dermatoses (p < 0.05) are in second place in the frequency of registration of diagnostic errors, in whom in most cases (71.4%) syphilis copied the clinical picture of an existing skin disease.
Here is my own observation.
Patient M., 25 years old, a rural resident who suffered from mycosis of the hands and feet, turned to the district dermatovenerologist with complaints of the appearance of “red spots” on the skin of the groin area. With a diagnosis of intertriginous athlete's foot, onychomycosis of the feet, he received desensitizing therapy and external antimycotic agents for a month. Due to the lack of a positive effect, he was sent for consultation to the Republican Internal Affairs Committee. Upon examination, the patient was found to have two ulcerative hard chancres at the root of the penis, erosive papules in the perianal area, condylomas lata in the inguinal-femoral folds, maceration and weeping of the skin of the interdigital spaces of the feet, and polyadenitis. At the same time, the patient had clinical manifestations of mycosis of the hands and feet (Fig. 1, 2). Serological reactions to syphilis are positive, treponema pallidum was found in the discharge from the surface of hard chancre and erosive papules. Elements of a fungus were found in scrapings from the nail plates. Diagnosis: secondary syphilis. Mycosis of the hands and feet. Onychomycosis.

In third place in terms of the number of diagnostic errors were patients in whom syphilis occurred as a combined infection (p < 0.05). The examination of this group revealed a significant decrease (p < 0.05) in the effectiveness of the method of direct detection of Treponema pallidum in comparison with patients without concomitant STIs. This caused 6 diagnostic errors. Patients with co-infection also significantly more often complained of itching (p < 0.05), which is not characteristic of syphilis, and therefore misled specialists in 8 cases.
As an example, we give an observation from our own practice.
Patient V., 18 years old, went to the antenatal clinic to register for pregnancy. She complained of itching in the genital area, and therefore was referred for consultation to a dermatovenerologist. During examination, rashes were detected in the anogenital zone, treponema pallidum was not detected, and vaginal discharge contained Trichomonas vaginalis and mycelial threads. A diagnosis was made: genital warts, urogenital trichomoniasis, candidiasis. Only a week after receiving a positive result of serological tests, secondary syphilis was verified in the patient.
Neurosyphilis was diagnosed in 7 patients with early manifest syphilis. At the same time, 5 of them turned to specialists of a different profile for the first time. Despite the fact that these patients had manifest manifestations of syphilis on the skin and mucous membranes, verification of the diagnosis occurred with a significant delay.
Here is an observation from our own practice.
Patient M., 49 years old, went to the local clinic with complaints of hearing loss. At the same time, she noted hair loss and the appearance of a rash on the genitals. I considered myself sick for two weeks. An otolaryngologist at the clinic identified the presence of cerumen and prescribed local treatment. Due to the lack of effect, the patient returned to the otolaryngologist at the local clinic a month later. On the day of treatment, the wax plug was removed, and a rapid examination for syphilis was carried out. After the procedure, the hearing did not recover, and after 5 days the patient returned for an appointment, from where, due to the positive result of the MCI, she was sent to the hospital. Upon examination, the patient was found to have diffuse hair loss, a positive Grigoriev–Fournier and Pincus sign, and lenticular papules on the palms, soles, and labia majora. In the Romberg position there is instability, sluggish reaction of the pupils to light, nystagmus, asymmetry of the nasolabial folds. The patient was consulted by an ophthalmologist, neurologist, and otolaryngologist. Diagnosis: secondary syphilis of the skin and mucous membranes. Specific meningoencephalitis. Retinal angiopathy. Left-sided salpingootitis. After specific therapy, the rashes on the skin and mucous membranes disappeared, hair growth began, and hearing was restored.
In 1/3 (30.8%) of cases when examining patients with primary seropositive and secondary syphilis, the cause of errors was false negative MRI results.
As an example, here is an observation from my own practice:
Patient G., a resident of the village, applied to the district hospital with complaints of swelling in the crown of the head, headaches that worsened at night, and the presence of a small-spotted rash on the abdomen. She was examined by a dermatovenerologist and a therapist, examined for syphilis using the MCI method with a negative result. With a diagnosis of intracranial pressure; pityriasis rosea" was sent to the neurosurgical department of the Republican Clinical Hospital, where she remained for 5 days with a suspected brain tumor. During this time, she was consulted by a neurosurgeon, neurologist, and gynecologist, whose medical history reflected the presence of a rash on the torso. On the fifth day of hospitalization, after receiving a positive result of a serological examination for syphilis, she was taken to the dermatovenerological dispensary, where examination revealed: a painful infiltrate of testy consistency measuring 3 × 4 cm in the parietal region on the right, a roseolous rash on the torso, erosive papules on the mucous membrane of the vestibule, in which Treponema pallidum was detected. Diagnosis: secondary syphilis of the skin and mucous membranes. Diffuse syphilitic periostitis of the right parietal region.
Both early and late forms of syphilis can manifest not only as syphilides on the skin and mucous membranes, but also by damage to other organs and systems. Due to the lack of specific symptoms, diagnostic errors are especially common in such patients. A retrospective analysis of 108 medical records of inpatients (form No. 003 1-y) of patients with latent infection showed that in 3.7% of cases, patients had objective symptoms of damage to the central nervous system in the form of basal meningitis, early meningovascular syphilis and ischemic stroke. All of them were identified when contacting the general somatic network with complaints of decreased hearing, vision, severe headaches, and increased blood pressure. However, they were diagnosed with early latent syphilis, according to which treatment was prescribed according to the recommended regimens for the early latent period, which in 2 cases led to serious consequences.
Patient Z., 61 years old, a rural resident, applied for a therapeutic appointment at the Central District Hospital with complaints of headache, dizziness, and increased blood pressure for two months. Due to positive serological tests, she was sent to the Republican Clinical Internal Affairs Department, where a diagnosis was made: latent early syphilis, hypertension. On the first day after the prescription of penicillin therapy, numbness and weakness of the left extremities, severe headache, and nausea appeared. With a diagnosis of ischemic stroke in the form of left-sided hemiparesis and motor aphasia, she was transferred to the neurological department, where, despite the treatment measures taken, she died. Lumbar puncture: 3 ml of cerebrospinal fluid, cytosis - 3, protein - 0.099‰, serological testing was not performed. At autopsy: ischemic infarction in the brain stem and the right lobe of the cerebellum against the background of general atherosclerosis with predominant damage to the aorta and cerebral arteries. This observation is worthy of special attention, since an incorrect diagnosis, unrecognized damage to the central nervous system and inadequate therapy led to the death of the patient.
Patient P., 36 years old, a village resident, while working in the field, felt a severe headache, dizziness, darkening of the eyes, and then lost consciousness. He was taken to the Republican Clinical Hospital. During examination by the doctor on duty, a diagnosis was made: subarachnoid parenchymal hemorrhage? Right-sided hemiparesis. Episyndrome. Brain swelling. Coma. After resuscitation measures, the patient's condition improved. Due to sharply positive serological reactions to syphilis, he was examined by a dermatovenerologist. Diagnosis: latent early syphilis. Treatment with bicillin-3 was prescribed on an outpatient basis. Two months later, his condition sharply worsened again, and P. was hospitalized in the neurological department of the Central District Hospital with a diagnosis of status epilepticus, 2nd degree coma. When examining the cerebrospinal fluid, a complex of serological reactions to syphilis was found: ++++, pleocytosis of 6 cells per 1 mm3, protein 0.6 g/l. The patient was transferred to the Republican KVD, where, with a diagnosis of “early meningovascular neurosyphilis,” he received specific treatment in combination with vascular and nootropic drugs. After penicillin therapy, there was a rapid regression of neurological symptoms and normalization of cerebrospinal fluid readings. The patient was discharged for clinical and serological control in satisfactory condition. This observation confirms the ineffectiveness of treating patients with late forms of syphilis with durant penicillin drugs, since they poorly penetrate the blood-brain barrier and do not lead to the elimination of the pathogen.
conclusions
Thus, diagnostic errors are most often associated with a carelessly collected anamnesis, an incomplete or inattentive initial examination, a highly professional approach to the patient, insufficient knowledge of the clinic of syphilis, the pathomorphosis of the infection, and the lack of comprehensive laboratory diagnostics. The absence of signs of banal inflammation, the typicality of the clinical picture, and the presence of regional scleradenitis should alert the doctor to a syphilitic infection. The proportion of diagnostic errors is significantly higher in groups of patients with significant deviations from the standard course of the disease: with concomitant STIs, dermatoses and extragenital localization of syphilides.
Literature
- Akovbyan V. A., Prokhorenkov V. I., Novikov A. I. et al. Syphilis. M.: Medkniga, 2002. 300 p.
- Astvatsaturov K.R. Syphilis, its diagnosis and treatment: A guide for doctors. M.: Medicine, 1971. 432 p.
- Department of Health and Human Services, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006 // MMWR, 2006, vol 55, 94 p.
- Prokosch V. Ophthalmological symptoms as key findings in neurosyphilis-diagnosis and therapy // Klin Monatsbl Augenheilkd. 2009. V. 226, No. 3. P. 184–188.
- Katunin G.L., Frigo N.V., Rotanov S.V. et al. Analysis of the incidence and quality of laboratory diagnostics of neurosyphilis in the Russian Federation // Bulletin of Dermatology and Venereology. 2011; 3: p. 18–26.
- Kubanova A. A., Lesnaya I. N., Kubanov A. A. et al. Development of a new strategy for controlling the spread of sexually transmitted infections in the Russian Federation // Bulletin of Dermatology and Venereology. 2009; 3: p. 4–12.
- Mavlyutova G.I., Yusupova L.A., Minullin I.K. Practical aspects of the evolution of clinical markers of syphilitic infection. Training manual for doctors. Kazan: Medok. 2013. 36 p.
- Dmitriev G. A., Dolya O. V., Vasilyeva T. I. Syphilis: phenomenon, evolution, innovation. M.: Binom, 2010. P. 367.
- Frishman M.P. Errors in the diagnosis of syphilis. Kyiv: Health, 1983. 136 p.
- Lewis DA, Young H. Syphilis // Sex Transm Infect. 2006, 82(Suppl IV): 13–15.
- Norris SJ, Pope V., Johnson RE, Larsen SA Treponema and other human host-associated spirochetes. In Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, eds. Manual of Clinical Microbiology. Washington DC: American Society for Microbiology, 2003: 995–971.
- Chebotarev V.V. Syphilis. Stavropol: Printing house “Seventh Heaven”. 2010. P. 445.
- Cubillan LD, Cubillan EA, Berger TG et al. Syphilitic uveitis and dermatitis // Arch. Ophthalmol. 1996. V. 114 (8). P. 1017–1018.
- Hama K., Ishigushi N., Tuji T. et al. Neurosyphilis with meziotemporal magnetic resonance imaging abnormalities // Intern med J. 2008; 47; 1813–1817.
- Thin P. Clinical syphilis - modern management // JEADV. 1997. V. 9 (1). R. 20.
G. I. Mavlyutova1, Candidate of Medical Sciences L. A. Yusupova, Doctor of Medical Sciences, Professor
GBOU DPO KSMA Ministry of Health of the Russian Federation, Kazan
1 Contact information
What set of tests should I take if I receive a false positive response to syphilis?
A false result requires additional diagnostic methods.
To clarify the diagnosis, treponemal studies are used.
They are specific and give a more accurate result.
These are the following testing methods:
- ELISA
- RPGA
- REEF
- RIBT
If the result is positive, you should contact a venereologist.
He may order additional studies or repeat tests.
Features of the study
Depending on what analysis is carried out, its pricing policy will fluctuate. If we are talking about donating blood for a routine examination at a dispensary, then usually the price is purely symbolic - payment for the syringe itself for collecting biological material. But the cost of such a study in private centers, or assessing the patient’s condition using innovative techniques, may turn out to be much more expensive. Therefore, it is better to find out exactly how much the manipulation costs in advance.
To determine the pathogen, as well as the stage of development of the lesion, the reagin and treponemal tests will still have to wait. It is believed that detection of antibodies is effective only after at least three weeks. Ideally, you should wait about five weeks after unprotected sex before going to the hospital.

Otherwise, achieve a true clinical picture. But not everyone understands why we have to wait about another month before dealing with the truth. The reason lies in the fact that the delivery coincides with approximately the tenth day after the appearance of the first characteristic sign of pathology. This is a syphilitic ulcer that forms at the site of infection entering the body.
Against this background, some potential infected people want to take a roundabout route, using express methods. But before the expiration of the specified time frame, conducting a preliminary assessment will only end in a waste of money.
Having figured out how many days it is necessary to wait in quarantine mode, a person should also become familiar with the algorithm for collecting biological material. Large vessels become the main source for monitoring. It is most convenient to take blood from a large vein in the elbow area.
Sometimes a bruise then forms at the injection site, or during the process of collecting material a person experiences a sensation similar to a burning sensation. But such phenomena are a completely normal reaction of the body to external interference.
Some victims are concerned about whether a complete blood test will show the presence of a syphilis infection. But for a thorough check, the biological material collected from a finger will simply not be enough. Due to the fact that the finger contains only capillaries, delivering the volume required for assessment will be problematic.
Because of this, doctors prefer larger veins, which does not exclude the possibility of taking a finger prick test for a screening examination. It acts as an auxiliary tool for identifying the dynamics of recovery. This approach could also be something of a trial measure.
If, during standard testing, causes for concern are discovered, then a detailed analysis of the ulnar vein is performed.
One more point will help avoid unnecessary retakes for those who prepare for the diagnosis incorrectly. According to the protocol, the victim must come to the appointment on an empty stomach. This means that the last meal should be taken at least eight hours before the scheduled intervention.
If this principle is ignored, the material will be unsuitable. Sample deterioration occurs due to dissolved fatty components of ingested food entering the biological fluid.
In order not to redo everything again due to your own carelessness, preparation should be carried out especially carefully.
False-positive syphilis: is it necessary to treat?
If you receive a false result, it is recommended to undergo additional research.
This will allow you to make an accurate diagnosis.
If the repeated examination shows a negative result, treatment for syphilis is not carried out.
A positive result requires mandatory drug treatment.
In this case, it is necessary to begin treatment for syphilis as soon as possible.
Antibacterial therapy, immunostimulating drugs, hepatoprotectors and eubiotics are prescribed.
How to treat syphilis?
The treatment regimen and type of drug are determined by a specialist based on the results of the study.
The basis of therapy is antibacterial drugs.
They are selected individually.
The following groups of antibiotics can be used in treatment:
- 1. Macrolides
- 2.Penicillins
- 3.Tetracyclines
- 4. Cephalosporins
Most often, the basis of treatment is penicillin.
This drug effectively copes with the disease.
Medicines Bicillin-1,3,5, Ampicillin and Oxacillin can be used.
If the causative agent of syphilis is resistant to penicillin drugs or an allergic reaction develops, drugs from other groups are used.
This may be Doxycycline, Ceftriaxone or Erythromycin.
The drugs can be given as injections or tablets.
After treatment, the effectiveness of the course of therapy is monitored.
At the end of the course of therapy, control studies are required.
Attention! Throughout the course of treatment, any sexual intercourse should be abolished.
Your sexual partner should definitely undergo examination and treatment.
Even after undergoing therapy, traces of Treponema pallidum will be noted in the blood.
Therefore, when conducting research, the result may give a positive answer.
Antibodies to syphilis can persist for a long time.
Blood test
Depending on the specific stage of development the pathology is at, subsequent therapy will differ. But to establish the stage, it is impossible to do without an appropriate clinical trial.
The name of each phase will indicate the severity of the disease. Thus, primary syphilis indicates the formation of a specific ulcer. In professional terminology, it is called chancroid. At the same time, the victim’s lymph nodes become inflamed.
If you donate blood from a vein at the initial stage of the lesion, you will be able to achieve the highest productivity of the subsequent therapy program. But if you ignore the primary alarming symptoms, you can only reach secondary syphilis.
It is characterized by the appearance of a special skin rash. The victim also becomes extremely contagious, posing a significant threat to others. Since the internal reserve of strength goes to fight the infection, the immune system gradually weakens. This suggests that catching hepatitis or any other disease of this kind is becoming much easier.
The latent course, when there are no typical signs of damage, is considered separately. Only a specific laboratory test can detect them. But being asymptomatic does not mean that the victim has ceased to be infectious. Particularly dangerous is the possibility of transmitting the infection from mother to fetus.
The final stage, called tertiary, includes severe skin lesions, destruction of the brain, bones and internal organs. This happens to approximately a third of all those infected, most of whom simply waited until the last minute or were not treated properly.
The basis for modern tactics of examining a prospective patient is not only a survey and examination, as it was a hundred years ago. Now the main tool in establishing an accurate diagnosis is a specific test, which requires the victim’s blood.
We are talking about testing for antibodies of the IgG and IgM classes. The first option indicates possible identified antibodies to the pathogen. It is not for nothing that among doctors it is briefly called simply the “treponemal test.”
The second version involves studying nonspecific antibodies. Here the basis is based on the detection of components that are released from cells destroyed by the causative agent of the disease.
This approach has several names, but they all retain the same general principle:
- nonspecific antiphospholipid test;
- nontreponemal anticardiolipin test;
- reagin test.

All of the above is based on the foundation laid in the RW algorithm, which means the Wasserman reaction.
Both clinical solutions are used not only for diagnosing pathology. They are used during potent therapy to assess the ongoing dynamics of recovery, and after treatment.
The only difference between the two procedures is the results of the examination of a person who has already successfully overcome the disease. Thus, non-treponemal results at the end of a successfully completed drug course will show the absence of a reaction. A negative response is explained by the absence of biological processes associated with the destructive effects of the pathogen on healthy cells of the body.
But the treponemal analogue, even after the period of successful treatment has ended long ago, will forever be positive. It follows that a positive response does not always guarantee relapse.
In addition to the two most popular diagnostics, there are several more that are used a little less frequently for various reasons, but they are still practiced in laboratories.
This is about:
- RPGA;
- RIBT;
- immunoblotting.
If a serological approach is relevant, the strategy can be expanded even further. It usually covers ELISA. But you should learn about the features of bladder cancer and MCI from your attending physician individually.
Decoding indicators
In the INVITRO laboratory, the results of the RPR test, in the case of a positive result, are expressed semi-quantitatively in titers (the maximum dilution of blood serum at which a positive reaction is detected). If anticardiolipin antibodies are detected, the answer is “positive” and the titer values are given in the commentary.
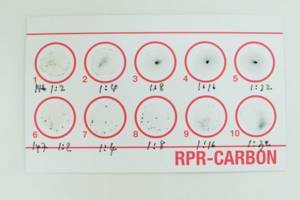
The titer value is used for subsequent monitoring of the effectiveness of treatment: after adequate treatment of primary and secondary syphilis, the titer should decrease by 4 times after 3-4 months and by 8 times after 6-8 months. In most patients treated early in the course of infection, titers may decline to trough levels or sensitivity thresholds after approximately one year.
In the absence of anticardiolipin antibodies, the answer is “negative”.
Additional examinations in case of deviation from the norm
The RPR test is accessible, inexpensive and has a fast turnaround time.
Therefore, it is used to screen for syphilis as a screening test. A positive RPR test cannot make a diagnosis of Syphilis; it must be confirmed by specific treponemal tests. The RPR test detects antibodies not to the pallidum itself, but to the material released from the cells of the macroorganism damaged during syphilis. Since cell destruction can also occur in other diseases, false-positive results may occur in laboratory tests based on cardiolipin antigen.
Any doctor can refer you for an RPR test:
- therapist,
- obstetrician-gynecologist,
- oncologist, etc.
All examined persons with a positive result of the RPR test should be referred to a venereologist, who, taking into account clinical data and anamnesis, decides on a further comprehensive serological examination. To clarify (confirm) the diagnosis, the following laboratory tests may be prescribed:
- Antibodies of the IgM class to Treponema pallidum (anti-Treponema pallidum IgM).
Negative result
The specificity of the test is 98%.
The sensitivity of the test depends on the stage of syphilis: for primary syphilis it is 86%, for secondary syphilis - 100%, for latent - 89%, for late - 73%.
Although a negative result indicates the absence of infection, it still does not exclude the presence of early primary syphilis or late tertiary syphilis.
After treatment, only receiving three consecutive negative RPR results after examination by specialists (neurologist, ophthalmologist, otolaryngologist) and liquorological examination according to indications allows the patient to be removed from the register.
Syphilis RPR (Rapid Plasma Reagin - anticardiolipin test)
You can take a blood test for syphilis at the nearest INVITRO medical office.
A list of offices where biomaterial is accepted for laboratory research is presented in the “Addresses” section. Blood for analysis is taken from a vein.
The material being tested is blood serum.
The determination method is flocculation (the RPR antigen used in the kits is a modification of the VDRL antigen).
Interpretation of study results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc.