Instrumental studies are often used in the diagnosis of diseases of the thoracic cavity. One of the most effective methods is CT of the mediastinum with contrast. Computed tomography allows you to visualize the structure of internal structures without invasive manipulation. The exception is the intravenous administration of a “coloring” iodine-containing solution.
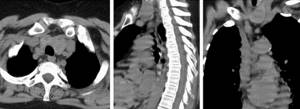
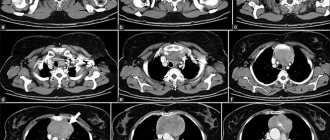
CT scan of the mediastinum, axial, sagittal and frontal projections
Ionizing flows are used to examine tissues. Unlike linear radiography, during CT a given area can be scanned at a certain depth. As a result, photographs of thin (from 0.5 mm) sections of the area under consideration are obtained. Computed tomography of hard tissues (bones, cartilage) and hollow organs is more effective. To increase the information content of scanning, bolus amplification is used.
CT scan of the mediastinum with contrast is prescribed for visualization of soft tissues, the vascular system, and neoplasms. The method provides a detailed study of the internal organs and anatomical structures of the chest cavity.
Several compelling reasons to do a mediastinal CT scan at NEARMEDIC
High professionalism of the medical staff
Specialists with experience of 10 years or more have professional knowledge not only in the medical field, but also in the field of computer technology.
Radiologists and radiologists skillfully set the required research parameters (degree of overlap of bands, voltage, current, etc.) and the mode of digital image processing. The reliability of the mediastinal CT result and the accuracy of the diagnosis depend on how accurately and competently the parameters are set. Innovative equipment
The CTE General Electric tomograph has the latest software, meets modern safety requirements, technical parameters and allows for expert-level research with reduced radiation exposure, while obtaining high-quality images.
The multi-slice device has several rows of receiving sensors, which makes it possible to examine the entire organ, as well as monitor its operation online. Thanks to the high quality of images and the creation of a three-dimensional model, the doctor identifies mediastinal formations on CT, studies the lesion in detail and prescribes effective treatment.
Publications in the media
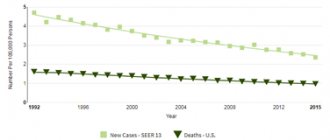
Benign mediastinal tumors are detected more often than malignant ones (4:1). Among benign neoplasms, the most common are teratomas and neuromas, and among malignant neoplasms, tumors of lymphoid tissue are most common. In the anterior mediastinum, tumors are registered 2 times more often than in the posterior one.
Classification • Benign tumors •• Thymomas •• Teratomas •• Neurogenic tumors (neurinomas) •• Connective tissue tumors (lipomas, chondromas) •• Vascular tumors (hemangiomas) •• Bronchogenic cysts •• Pericardial cysts • Malignant tumors •• Lymphomas •• Germinomas •• Neuroblastomas.
Tumors of the anterior mediastinum • Dermoid cysts (teratomas) •• Frequency. Teratomas are more often detected in adolescents. In 80% of cases, these tumors are benign •• Etiology. Teratomas arise from the same embryonic pharyngeal pouch as the thymus gland (III–IV pairs) •• Pathological anatomy. The teratoma includes derivatives of all germ layers, including elements of ectodermal, endodermal and mesodermal origin •• Diagnosis. Teratomas are diagnosed by radiography. On photographs they appear as smooth-walled cysts or dense homogeneous shadows, often with calcified walls. A variety of structures (for example, teeth) can be found inside the tumor. These cysts are usually asymptomatic until infectious complications or malignant changes develop ••
Treatment: thoracotomy, complete removal of the tumor. • Thymomas (tumors of the thymus gland) •• Frequency. Among neoplasms of the anterosuperior mediastinum in adults, thymomas are most often detected. Thymomas can occur at any age, most often at 50–60 years of age. In 40–50% of patients, thymoma causes concomitant pseudoparalytic myasthenia gravis •• Morphology ••• Thymus tumors, by cellular nature, can be lymphoid, epithelial, spindle cell or mixed ••• 2/3 of thymomas are regarded as benign; of these, 10% are represented by simple cysts ••• With epithelial thymomas the prognosis is unfavorable, with spindle cell thymomas it is much better ••• It is easiest to distinguish a benign tumor from a malignant one by its tendency to damage adjacent tissues. Benign tumors are encapsulated. Malignant tumors are invasive, they grow into nearby organs or pleural cavities. Distant metastasis is relatively rare •• Diagnosis ••• Most patients with thymomas are asymptomatic; The tumor is discovered accidentally during a chest x-ray. The appearance of symptoms is due to invasion of a malignant tumor. Chest pain, shortness of breath, and superior vena cava syndrome occur ••• Abnormalities detected during X-ray, CT, or MRI of the chest organs help in the diagnosis; concomitant pseudoparalytic myasthenia gravis. In such circumstances, it is necessary to examine the mediastinum for the presence of a thymic tumor. The greatest help is provided by lateral radiography of the chest organs, since in the direct projection, small tumors can be hidden in the shadow of large vessels •• Surgical treatment. Most thymic tumors are removed through a median sternotomy approach (thoracotomy is possible) ••• Thymomas not accompanied by myasthenia gravis: mediastinal examination and tumor removal are necessary ••• Benign tumors are removed ••• Malignant tumors. If possible, all areas of tumor spread should be removed. When an infiltrating thymic tumor cannot be completely or partially removed, postoperative radiation therapy is resorted to. Chemotherapy and immunotherapy have no clinical benefit ••• Thymomas associated with myasthenia gravis should be removed en bloc along with the rest of the thymus.
• Connective tissue tumors •• Frequency. They occupy third place among mediastinal tumors •• Morphology. Tumors are represented by fibromas, lipomas, chondromas, myxomas •• Diagnosis. Usually patients have no complaints. Typically, such tumors are detected by x-ray. Tumors are localized in both the upper and lower parts of the anterior mediastinum. They often do not have clear boundaries, their capsule is not expressed in all parts •• Treatment is surgical •• The prognosis is favorable.
Tumors of the posterior mediastinum • Neurogenic tumors (neurinomas) •• Frequency. They occupy the second place among mediastinal tumors. Neuromas can be a manifestation of neurofibromatosis (von Recklinghausen's disease) •• Etiology. Tumors develop from the nerve elements of the sympathetic trunk, branches of the vagus nerve, meninges and intercostal nerves. Most often located in the upper mediastinum •• Morphology. Schwannomas, neurolemmomas, ganglioneuromas, neurofibromas •• Diagnosis. Most patients with neuromas have no complaints. When a tumor grows in the lumen of the spinal canal (in the form of an hourglass), neurological symptoms are possible. The diagnosis is made radiographically, using a CT scan of the chest. On photographs, tumors appear as round, clearly defined shadows located in the area of the costovertebral angle •• Treatment - thoracotomy, tumor removal ••
The prognosis is favorable. • Vascular tumors (hemangiomas, lymphangiomas) are quite rare •• Etiology. Tumors develop from elements of the wall of blood or lymphatic vessels •• Morphology. Tumors are represented by vascular formations. Quite often their malignant transformation occurs •• Diagnosis is made by x-ray and CT scanning •• Treatment is surgical. • Bronchogenic cysts are detected quite rarely, more often in women •• They develop from mixed germinal buds of the foregut or tracheal kidney •• Morphology. Thin-walled formations filled with transparent (sometimes mucous) contents. The inside of the cyst wall is lined with ciliated epithelium •• X-ray diagnosis •• Surgical treatment.
• Pericardial cysts are thin-walled formations with transparent contents that easily rupture when released. The inside of the cysts is lined with single-layer squamous or cubic epithelium and is located in the lower parts of the mediastinum. Malignant tumors of the mediastinum
• Lymphoma. In 50% of patients with lymphomas (including Hodgken's disease), the mediastinal lymph nodes are involved in the process. Of these, only 5% are affected exclusively by the mediastinum •• Symptoms: cough, chest pain, fever and weight loss •• Diagnosis is confirmed by radiography and lymph node biopsy. The latter is performed with mediastinoscopy, anterior mediastinotomy or thoracoscopy •• Surgical treatment is not indicated. Patients are subject to combined chemotherapy and radiation therapy.
• Germinomas are tumors arising from embryonic germs that normally differentiate into sperm and eggs. These neoplasms account for less than 1% of all mediastinal tumors. Their metastases are recorded in the lymph nodes, pleura, liver, bones and retroperitoneum •• Histological types ••• Seminoma ••• Embryonic cell sarcoma ••• Teratocarcinoma ••• Choriocarcinoma ••• Endodermal sinus tumor •• Symptoms: chest pain, cough and hoarseness due to damage to the recurrent laryngeal nerve •• Diagnosis. Various methods of radiation diagnostics are used (radiography, MRI, CT of the chest organs) •• Surgical treatment . If possible, complete removal of the tumor •• Adjuvant therapy. Seminomas are very sensitive to radiation. For other cell types, chemotherapy gives good results.
ICD-10 • C38 Malignant neoplasm of the heart, mediastinum and pleura • C78.1 Secondary malignant neoplasm of the mediastinum • D15.2 Benign neoplasm of the mediastinum
CT scan of the mediastinum - indications, advantages and features of the procedure
The mediastinum area includes the trachea, esophagus, aorta, heart and its great vessels, thoracic lymphatic duct, vagus and phrenic nerves, main bronchi, and thymus. Between these organs and structures is the mediastinum itself - fibrous connective and fatty tissue with small blood and lymphatic vessels and nerves.
If pathology in the mediastinum is suspected, the doctor may prescribe radiography as a primary diagnostic procedure, but only CT provides the maximum possible information.
Anatomy and physiology of the thyroid gland
The thyroid gland is a hormone-secreting organ, which is a vascular encapsulated structure consisting of the right and left lobes, which are connected along the midline by an isthmus. The main role of the organ in question is the production of hormones (triiodothyronine (T3) and thyroxine (T4)) responsible for metabolic processes (metabolism), growth and development of the body, mental health, sexual functions, immunity and activity of the cardiovascular system. The production of these biologically active substances is regulated by the pituitary gland, which synthesizes thyroid-stimulating hormone (TSH). The higher its level, the larger the size of the thyroid gland.
The production of TSH is inhibited, in turn, by T3 and T4. This is an interconnected system, so the concentration of hormones in the blood is almost constant.
The difference between radiography and CT
X-rays clearly show the condition of the lungs, but other organs of the mediastinum in the images are represented by an undifferentiated shadow, the density and shape of which does not say anything about the patient’s condition. Unlike radiography, a multi-slice computed tomograph provides layer-by-layer images in which all structures of the mediastinum are clearly visible and distinguishable from each other.
Conventional x-ray shows only significantly enlarged or calcified lymph nodes, while mediastinal CT reveals lymph nodes with even slight changes.
During a CT scan, the areas of the body being examined are scanned with X-rays that have special characteristics. This allows you to obtain layer-by-layer clear images of the heart, lungs, bronchi, lymph nodes, parts of the esophagus, and blood vessels. The mediastinum and respiratory organs are represented in the resulting images with the highest accuracy. Thanks to such detail, when decoding the results of the study, the specialist determines the presence of pathology in the patient with the greatest possible accuracy.
For what symptoms can an MRI of the thyroid gland be done?
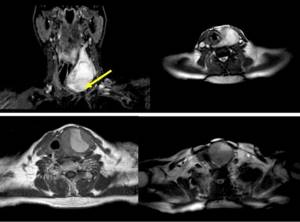
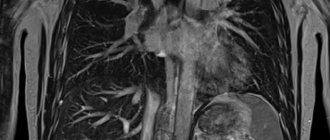
View of the thyroid gland on MRI tomograms (the arrow indicates the area of pathological changes)
Symptoms for which an MRI of the thyroid gland is recommended include:
- enlargement of the organ upon palpation or visible to the naked eye;
- the appearance of a tumor mass in the neck;
- difficulty swallowing;
- unexplained weight fluctuations, both down and up;
- enlargement of the cervical, subclavian and supraclavicular lymph nodes;
- hoarseness of voice;
- insomnia, tearfulness, mood swings, rapid heartbeat (symptoms characteristic of hyperthyroidism).
Magnetic resonance imaging will help clarify the situation if there are changes in clinical and laboratory parameters: an increase or decrease in the level of thyroid hormones in the blood serum (hyper- and hypothyroidism), the presence of a large number of specific antibodies (Hashimoto's disease, Graves' disease, thyroiditis, type 1 diabetes , rheumatoid arthritis).
The level of calcitonin in the blood is higher with a certain type of thyroid cancer, but the same result may be present in other diseases - chronic renal failure, disorders of calcium metabolism. In this case, MRI will help confirm or refute tumor pathology and direct the diagnostic search in the right direction.
Pathologies of the thyroid gland can be asymptomatic or manifested by a variety of complaints.
Advantages of mediastinal CT
Maximum awareness
Unlike conventional x-rays, CT images provide specialists with the opportunity to recognize those abnormal changes in the mediastinum that are not visible on x-rays.
Minimal contraindications
Computed tomography has virtually no contraindications (with the exception of pregnancy); examination is prescribed even for children.
The painless CT procedure
of the mediastinum is absolutely painless and allows you to replace such complex and quite unpleasant diagnostic methods for the patient as endoscopic examinations of the bronchi, esophagus, and trachea.
Safety
When performing a CT scan, the risk of complications is minimized. The X-ray radiation used during the procedure has low intensity and is therefore safe for humans. The radiation dose reduced several times allows CT scanning of the mediastinum to be performed up to 3 times a year. The contrast used in some cases also does not pose any threat to human health (in the absence of a predisposition to allergies - hypersensitivity).
Alternative Methods
As an alternative for CT examination of organs and tissues of the chest, MRI is conditionally suitable. However, this diagnostic method is not always relevant. The use of MRI to examine the chest is possible only in exceptional cases, for example, for a detailed study of the diaphragm or the apices of the lungs. In general, MRI of the chest is not a very good solution in diagnosing diseases in this area.
Sometimes a chest CT scan can be replaced with a standard x-ray. It allows you to better study large tumors, foci of infectious diseases, characteristic signs of pleurisy and other disorders.
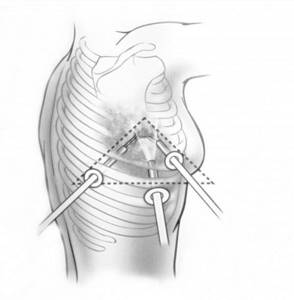
The mediastinal organs can be examined invasively. To do this, they resort to mediastinoscopy. The endoscope is inserted into the chest, which is then examined from the inside. The study is difficult for the patient to tolerate and is dangerous in terms of complications.
CT scan of the mediastinum with contrast
When mediastinal tumors are detected, a CT scan with contrast is prescribed - intravenous enhancement. In atypical cells, metabolic processes are highly intense. By actively delaying contrast, abnormal cells thus reveal themselves in the photographs.
Pharmacological preparations based on iodine are used as a special contrast agent. The body frees itself from the drug on its own within a few days. It is excreted naturally, by the kidneys, so contrast studies are not prescribed for patients with renal failure.
How to prepare for research
MRI of the thyroid gland does not require special preparation; it is enough to remove all metal jewelry, watches, hairpins and choose comfortable clothes (including underwear) without buttons, zippers or fasteners.
It is necessary to warn the doctor about possible or existing pregnancy and installed implants: pacemakers, terminals, insulin pumps, structures, etc. Fixed dentures are not a contraindication to MRI.
There are drugs (including herbal ones) that, when taken for a long time, affect the functions of the thyroid gland and can change its parameters. These include:
- acetylsalicylic acid;
- steroid hormones;
- thyroid medications;
- diuretics;
- St. John's wort.
If you are taking anything from this list, notify your doctor.
Take with you all the results of previous instrumental studies and blood tests for thyroid hormones, if any, were performed.
Treatment
Due to the variety of possible causes, mediastinal tumors are treated depending on the type of tumor:
- Thymomas require surgical treatment. In high-grade cases, surgery is followed by radiation therapy. Various approaches are used to remove the tumor: both minimally invasive and robotic surgeries, as well as open “major” surgeries (thoracotomy and sternotomy).
- Lymphomas are treated with chemotherapy and radiation therapy. Surgery in this case is used as a diagnostic method, not a therapeutic one.
- Neurogenic tumors are removed surgically.
- Some tumors, if they are not clinically apparent and are benign, can be kept under observation.