RPR: When can a test give false positive results?
RPR is a non-treponemal test and is not strictly specific for syphilis.
Therefore, such an analysis is rare, but can still give a false positive result.
It is for this reason that RPR is not a diagnostic criterion for syphilis.
If positive results of a screening test are obtained, the analysis must be rechecked with treponemal tests.
Why does this happen?
The fact is that the lipoproteins of the causative agent of syphilis are similar to the lipoproteins of human tissue.
Therefore, in some cases, the test does not detect the result of the activity of Treponema pallidum.
The analysis can show specific changes in the body.
The following conditions are associated with a false positive reaction:
- Infectious diseases in the acute stage;
- Injuries;
- Myocardial infarction, especially fresh;
- Poisoning;
- Recent vaccination or vaccination;
- HIV and hepatitis;
- Antiphospholipid syndrome;
- Connective tissue diseases;
- Autoimmune diseases;
- Liver damage;
- Pregnancy.
In addition, food products can give a false positive result.
This occurs if consumed on the eve of analysis.
It is not recommended to take fatty and spicy foods or alcohol the day before the test.
What can affect the result
False positive results may be detected in the following cases:
- the patient has certain autoimmune diseases (for example, systemic lupus erythematosus, endocrine pathologies), oncological processes in the body, blood diseases;
- the patient has diabetes mellitus;
- injection of narcotic substances;
- in older people (over 80 years old);
- frequent blood transfusions;
- the presence of infectious diseases (leprosy, malaria, HIV infection, etc.).
False-negative serological tests for syphilis may occur in immunocompromised individuals.
In what cases is RPR negative but syphilis is present?
The absence of a positive reaction is possible even in the presence of illness.
This happens in three cases:
a) Syphilis is at an early, seroresistant stage;
b) The patient has tertiary syphilis;
c) The “prozone effect” is observed
In the first days after infection, the body does not yet have time to produce lipoproteins.
At the stage of tertiary syphilis, a person’s immunity is significantly weakened.
Therefore, it does not produce enough antibodies for a positive test.
The prozone effect is a rare condition when the test does not detect the presence of antibodies.
This is due to their titer being too high.
Interpretation:
- If anticardiolipin antibodies are detected, a “positive” response is given with a titer value. At very low titers, the answer is “doubtful, it is recommended to repeat the study after 10 - 14 days.” Positive: RPR - primary seropositive syphilis (infection occurred 1 - 3 months ago); secondary seropositive syphilis (infection occurred more than 3 months ago); tertiary seropositive syphilis (infection occurred more than 3 - 4 years ago); the first year after treatment of syphilis; seroresistance after treatment of syphilis; APS is probable (if syphilis is excluded). False positive reaction (see interference).
- In the absence of anticardiolipin antibodies, the answer is “negative”. Negative: absence of infection, early primary (seronegative) syphilis cannot be excluded, late tertiary syphilis cannot be excluded.
Sample result (PDF)
What is done if RPR is positive during pregnancy?
As already mentioned above, a positive RPR during pregnancy is not a reason to panic.
During pregnancy, a woman undergoes screening tests for syphilis three times.
This is due to the need for early detection of infection.
This will be needed in the future to prevent damage to the fetus.
After a positive result of the RPR test, the woman is necessarily sent for additional studies.
In this case, specific treponemal tests are used.
Such analyzes guarantee an accurate result.
Treponemal tests are not used in advance due to their high cost and difficulty in performing.
If repeated tests indicate infection, the pregnant woman is given anti-syphilis therapy.
In this case, special antibiotics are selected with the least effect on the fetus.
Treatment of syphilis during pregnancy is necessary.
The potential harm from antibacterial drugs is significantly lower than the actual harm to the child.
general characteristics
Treponema pallidum has several antigens that cause the production of antibodies. One of them is similar to cardiolipin, which allows the latter to be used to detect immunity to treponema pallidum. RPR is a screening anticardiolipin test (non-treponemal) for detecting antibodies (reagins) of the IgG and IgM class to lipoid and lipoprotein-like material released from damaged cells of a patient with syphilis. Antibodies are detected in 70 - 80% of people with primary syphilis and in almost 100% of patients with secondary and early latent syphilis. In most cases, a positive RPR reaction is observed 7 - 10 days after the appearance of primary chancre or 3 - 5 weeks after infection, then titers decrease. About 30% of patients with late syphilis become non-reactive on the RPR test. A decrease in RPR titer by 4 or more times within 1 year after therapy confirms its effectiveness. In 90 - 98% of cases after treatment of syphilis, the result of the RPR test becomes negative. The test is not specific, so false-positive reactions may occur. Antilipoid antibodies can appear frequently in autoimmune diseases. If a positive result is obtained in the RPR test, the patient should be examined by a dermatovenerologist with an additional blood test - antibodies to Treponema pallidum IgG/IgM. These two studies are complementary; the combination of RPR and the IgG, IgM ELISA test represents the best screening test for detecting or excluding syphilis at all stages.
What symptoms and signs can there be with a positive test for syphilis?
Syphilis is a disease with a clear clinical picture.
Although lately subclinical and atypical forms of the disease have become increasingly common.
This is due to the indiscriminate use of antibiotics.
Another reason is the improvement in the standard of living of modern people.
Adequate nutrition, regular rest, and absence of heavy exercise lead to the strengthening of overall immunity.
Most often, syphilis manifests itself with clear and specific symptoms.
It varies depending on the stage of the disease.
Remember!
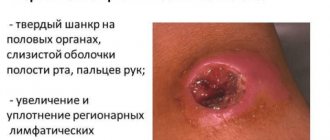
The main symptom of primary syphilis is chancre.
This is a round ulcer, it does not itch or cause pain.
Chancre appears 3 to 6 weeks after infection.
It is located at the site of infection.
Syphiloma often forms on the genitals, in the mouth, and in the anus.
Its appearance is accompanied by an increase in regional lymph nodes.
On palpation they are soft and painless.
This symptom is called syphilitic bubo.
The chancre heals on its own and leaves no traces behind.
It is not easy to detect the disease at this stage.
Since chancre does not cause discomfort, it is often ignored.
In addition, today chancre is often small in size.
They remain unnoticed in the folds of the skin.
Therefore, syphilis at the first stage of the disease is rarely detected by symptoms.
Secondary syphilis gives more vivid symptoms and is difficult to miss.
After the chancre heals, a specific syphilitic rash appears on the human body.
It can cover the entire body.
The elements of the rash, despite their severity, do not itch or hurt.
Later the rash disappears without a trace.
Important!
The disappearance of the rash does not mean a cure for syphilis.
The body simply accumulates a sufficient amount of antibodies and begins to resist infection.
The body cannot completely rid itself of syphilis.
Therefore, the rash returns, and this phenomenon is called recurrent syphilis.
Patients usually see a doctor at this stage.
Symptoms of tertiary syphilis mainly consist of destruction of tissues and organs.
Because of treponemas, tertiary syphilomas, or gummas, are formed.
The bulk of the pathogen is concentrated in them.
Therefore, a person with tertiary syphilis is less contagious than in the first two stages.
With tertiary syphilis, changes in organs can become irreversible.
During and after treatment, additional therapy from specialists is required.
Syphilis. Enzyme immunoassay for the detection of total antibodies of class M and G to the causative agent of syphilis
What kind of analysis is this? This is the detection of total class M and G antibodies to the causative agent of syphilis, which can be used as an effective ultra-sensitive screening test for diagnosing early syphilis infection.
At the moment, the Wasserman reaction is considered outdated, and since 2006 it has hardly been used to diagnose syphilis. It has been replaced by more sensitive and modern tests. However, the forms still display the unchanged “RW”. The signature “RW” is a tribute to tradition, a small unspoken rule among doctors: leaving the old signature, they now have in mind new modern tests for syphilis.
What biomaterial can be used for research? Venous blood
Treponema pallidum (treponema pallidum) is a bacterium that causes syphilis, a chronic venereal infectious disease that is most often transmitted sexually, for example, through direct contact with a syphilitic ulcer (chancroid), intrauterine infection is also possible.
The source of infection is a sick person. Syphilis is easily curable, but can lead to serious health problems if left untreated. An infected mother can transmit the disease to her fetus, which may develop serious and irreversible changes.
Syphilis is classified as a classic sexually transmitted disease (sexually transmitted disease). The causative agent is Treponema pallidum. Syphilis is characterized by a slow progressive course. In later stages, it can lead to severe damage to the nervous system and internal organs
Symptoms of syphilis
The symptoms of syphilis are very varied. They vary depending on the stage of the disease. There are three stages of syphilis:
Primary syphilis occurs after the end of the incubation period. At the site of penetration of the pathogen into the body (genital organs, oral mucosa or rectum), a painless ulcer with a dense base (chancroid) appears. 1-2 weeks after the onset of the ulcer, the nearest lymph nodes enlarge (if the ulcer is localized in the mouth, the submandibular nodes enlarge; if the genital organs are affected, the inguinal ones become enlarged). The ulcer (chancroid) heals on its own within 3-6 weeks. after occurrence.
Secondary syphilis begins 4-10 weeks after the appearance of the ulcer (2-4 months after infection). It is characterized by a symmetrical, pale rash over the entire body, including the palms and soles. The appearance of a rash is often accompanied by headache, malaise, and fever (as with the flu). Lymph nodes throughout the body enlarge. Secondary syphilis occurs in the form of alternating exacerbations and remissions (asymptomatic periods). In this case, hair loss on the head is possible, as well as the appearance of flesh-colored growths on the genitals and in the anus (condylomas lata).
Tertiary syphilis occurs in the absence of treatment many years after infection. This affects the nervous system (including the brain and spinal cord), bones and internal organs (including the heart, liver, etc.).
If infected during pregnancy, the child may develop congenital syphilis.
Complications of syphilis
According to scientific research, in the absence of treatment, about a third of patients develop tertiary syphilis. About a quarter of patients die because of it. Congenital syphilis can cause severe damage or death to the child.
Treatment of syphilis
It is quite complex and requires further long-term observation. It is worth noting that treatment of syphilis in the early stages is not particularly difficult in terms of choosing drugs. The peculiarity of Treponema pallidum is that it still retains sensitivity to penicillin , which is the drug of choice for syphilis.
In case of an allergy to penicillin, antibiotics from a number of macrolides (erythromycin, clarithromycin) or cephalosporins (ceftriaxone, etc.) are prescribed. The drugs are prescribed intramuscularly or in tablets. Treatment of active forms of the disease takes place in an inpatient setting; patients with a latent form can receive outpatient therapy. The duration of treatment depends on the stage of the disease and can take from several weeks to several years.
Antibodies to the causative agent of syphilis
When a person comes into contact with T. pallidum, their immune system reacts by producing antibodies to the bacterium. Two types of antibodies to Treponema pallidum can be detected in the blood: IgM and IgG. In response to T. pallidum infection, IgM antibodies to T. pallidum are the first antibodies produced by the body. They are detected in most patients at the end of the second week of the disease and are present in them in the primary and secondary stages. Class G immunoglobulins to T. pallidum appear in detectable quantities in the blood 3-4 weeks after infection. Their concentration increases and in the 6th week begins to prevail over the concentration of IgM, reaching a maximum, and then remains at a certain level for a long time. Starting from the 4th week, the amount of both types of immunoglobulins in the blood increases, which leads to a positive test result for total antibodies to T. Pallidum. This allows this test to be used for early diagnosis of T. pallidum infection. After effective treatment, the concentration of immunoglobulins gradually decreases, but this happens slowly; in some cases, antibodies can be detected after a year or more. Syphilis can be treated with antibiotics, and it is preferable to use penicillin derivatives. At an early stage, the disease is treated easier and faster. Longer therapy may be needed for patients infected for more than a year.
Why is the analysis carried out?
Increasing and decreasing indicators
For the diagnosis of syphilis. For examination of all pregnant women for preventive purposes (preferably at the first appointment with a gynecologist, when registering).
When is the study scheduled? For symptoms of syphilis, such as chancroid on the genitals or throat. When a patient is being treated for another STD, such as gonorrhea. When managing pregnancy, because syphilis can be transmitted to the developing fetus and even kill it. When it is necessary to determine the exact cause of the disease if the patient has nonspecific symptoms that are similar to syphilis (neurosyphilis). If the patient is infected, they should repeat the syphilis test after 3, 6, 12 and 24 months to ensure that treatment has been successful.
Results/Normal/Transcript of analysis
Reference values (normal values)
Result: negative. S/CO ratio (signall/cutoff): 0 - 0.9.
A positive result means that the patient has a recently acquired infection. However, a negative result does not always mean that the patient does not have syphilis.
Positive result
A positive result in a previously seronegative patient, as well as a significant increase in titers in paired sera taken at an interval of 7 days, indicates a primary infection. Detection of antibodies to treponema in the blood of a newborn helps confirm the diagnosis of congenital syphilis. In addition, the cause of a positive result may be tertiary or latent syphilis.
Negative result
A negative test result may indicate the absence of infection or its early stage when an immune response has not developed. At the same time, the absence of antibodies in a baby born from an infected mother does not exclude a congenital disease, since antibodies may not yet have formed at the time of the study.
Preparing for the test
Do not smoke for 30 minutes before donating blood
What can affect the result of the analysis?
False-positive results may occur with diseases such as HIV, Lyme disease, malaria, systemic lupus erythematosus, some types of pneumonia, as well as drug addiction and pregnancy. And many other somatic diseases.
Important Notes
- The examination for syphilis must be comprehensive and include taking into account the medical history, clinical picture and confirmation of the diagnosis by laboratory data.
- People who are sexually active should consult a doctor about any suspicious rashes or pain in the genital area.
- If a patient is diagnosed with infection, he/she needs to inform his/her sexual partner so that he/she can also undergo examination and, if necessary, treatment.
- With syphilis, the risk of contracting other sexually transmitted diseases increases, including the risk of contracting HIV, which leads to AIDS.
• Syphilis can also be transmitted through blood transfusion through contaminated medical instruments, so testing before hospital admission is very important.
Shapilova N.V.
Prognosis and complications of syphilis
Detection of syphilis at an early stage is the key to successful treatment and absence of consequences of the disease.
The less time the bacteria stays in the body, the less harm it will cause to health.
At the stage of primary syphilis, the course of treatment, dosage of antibiotics and the severity of complications are minimal.
When treating at the second stage, the increased amount of pathogen in the blood should be taken into account.
Because of this, damage to organs from Treponema pallidum will be more significant.
Tertiary syphilis is the most severe stage of the disease.
At this stage, organ damage may be irreversible.
This is especially true for neurosyphilis.
In this case, gummas are formed in the brain and spinal cord.
As a result, the effects of the disease may not go away after treatment.
Because of this, disturbances in movement, sensitivity and psyche are possible.
The same prognosis applies to partially or completely damaged tissues.
Extensive wounds after gumma breakthrough do not heal on their own without leaving a trace.
If the defect is severe, the patient may require the services of a plastic surgeon.
This specialist corrects cosmetic defects.
How do test titers change?
RPR titers indicate the amount of antibodies in a blood sample.
The more syphilis pathogen in the blood, the higher the titer.
The highest rates are observed in the acute phases of the disease, with primary and secondary syphilis.
At the third stage of the disease, titers drop.
Titers are an important indicator of the effectiveness of antibacterial therapy.
Therefore, RPR is a screening test also during treatment.
Thanks to it, the doctor can understand how effective the prescribed treatment regimen and drug are.
Sometimes titers do not begin to decrease after starting therapy.
This means that this strain of Treponema pallidum is resistant to the prescribed drug.
In this case, the doctor changes the antibiotic and adjusts the treatment regimen.
Detailed description of the study
One of the mechanisms of immune defense is normally the production of antibodies (immunoglobulins, Ig), which belong to the gamma globulin fraction of serum proteins. By their nature, antibodies are glycoproteins (molecules containing carbohydrate and protein) and are divided into five classes: IgA, IgM, IgG, IgE, IgD. They differ in structure and functions, but have a similar structure. When immunoglobulins react to the structures of the body’s own, they are called autoantibodies.
Antiphospholipid syndrome (APS) is an autoimmune disease that includes recurrent thrombosis and obstetric pathology. APS is based on the synthesis of antiphospholipid antibodies, which stimulate thrombus formation processes in various ways. These immunoglobulins come in several types, the main ones being:
- Lupus anticoagulant;
- Anticardiolipin antibodies;
- Antiphosphatidylserine antibodies;
- Antibodies to phosphatidic acid and beta-2 glycoprotein 1.
This study evaluates antibodies (IgA) to cardiolipin.
Antiphospholipid syndrome is one of the types of acquired thrombophilias. Thrombophilias are conditions in which thrombosis of blood vessels develops. With APS, blood clots occur in both the venous and arterial beds, and can also recur (recur) in 70-80% of cases in the same place. Deep vein thrombosis is dangerous due to the high risk of developing pulmonary embolism.
Thrombocytopenia may also occur with antiphospholipid syndrome. Thrombocytopenia is a condition in which the number of platelets in the blood is less than 150 × 109/L. People with thrombocytopenia have an increased risk of bleeding and bleeding. Numerous small purple dots may appear on the skin as a result of multiple hemorrhages, which is why the disease is called thrombocytopenic purpura.
There are primary and secondary APS. Primary is diagnosed when the cause of the increase in antiphospholipid antibodies is unknown. Secondary APS is diagnosed when an underlying disease is known, which causes an increase in the formation of antiphospholipid antibodies and is often associated with chronic stimulation of the immune system. The main four groups of reasons for such stimulation are:
- Autoimmune diseases;
- Taking medications (estrogen-containing oral contraceptives, psychotropic drugs);
- Infectious diseases (viral and bacterial, the production of antiphospholipid antibodies is especially common in HIV infection and syphilis);
- Malignant neoplasms.
A number of drugs increase the concentration of antiphospholipid antibodies, including phenothiazines and other drugs that cause drug-induced lupus: chlorpromazine, hydralazine, phenytoin, procainamide and quinidine.
Antiphospholipid antibodies are elevated in many acute infections, both viral and bacterial. However, in these conditions the increase is transient (short-term). Various chronic infectious diseases and especially HIV infection also provoke the formation of such autoantibodies. It is worth noting that in such patients the level of antiphospholipid immunoglobulins is not associated with the severity or stage of HIV infection.
As a rule, infectious patients with elevated levels of antiphospholipid antibodies do not have an increased risk of thrombosis. However, in some cases with viral infections, this rare complication occurs. More often, thrombotic complications are found in patients with autoimmune diseases (for example, systemic lupus erythematosus).
Obstetric pathology in APS is associated with the characteristics of miscarriage. Miscarriage caused by increased concentrations of antiphospholipid antibodies can occur at any stage of pregnancy. But most often it occurs in the second or third trimester. Fetal death is a consequence of thrombus formation in the small vessels of the placenta, due to which the latter ceases to perform its functions and further pregnancy becomes impossible.
AT to cardiolipin IgA.
Anticardiolipin immunoglobulins are found, according to various estimates, in healthy people with a frequency of 0-14%. Assessment of AT (IgA) to cardiolipin provides diagnostic reliability, allowing identification of the disease (APS) in the case when other screening tests show a negative result. This made it possible to include this study in international clinical guidelines for the diagnosis and treatment of antiphospholipid syndrome.
When to take RPR after infection?
It is important to remember that you should not get tested immediately after suspected infection.
In the early stages of the disease, the body does not produce enough antibodies.
Tests don't detect them.
During the serological window, negative results are possible even in the presence of infection.
Testing should be done at least 3 weeks after contact with an infected person.
This is necessary for reliable test results.
Prevention for family and partner in case of positive RPR test
Syphilis is rarely transmitted through household contact.
But this option is still possible.
Members of the patient's family are at risk if they live with him.
The elderly, young children and those with weakened immune systems are at greatest risk.
The risk of infection especially concerns a sexual partner - Treponema pallidum is highly contagious.
Important!
If RPR is positive, you should start taking precautions immediately.
The person should use separate dishes, cutlery and personal hygiene items.
Sexual contacts must be completely abandoned.
This applies to all types of sex and petting, as well as deep kisses.
A breastfeeding woman should transfer her baby to artificial feeding until final results are obtained.
If treponemal tests confirm the diagnosis, loved ones should be fully screened for syphilis.
In addition, people in contact with the patient undergo preventive treatment.
This is necessary to eliminate all risks of transmission of infection.
Usually it consists of a single or double injection of high doses of antibacterial drugs.
The exact scheme of preventive treatment and its need can only be determined by the attending physician.
Treatment regimen for syphilis with positive tests
At the stage of a positive RPR test, no treatment is prescribed.
Therapy is started only when the results of RPR are confirmed by specific treponemal tests.
Antibiotics are used to treat syphilis.
The penicillin group remains the most effective.
The drugs are usually administered intramuscularly.
The number of injections and the frequency of their administration depend on the chosen drug.
The treatment period ranges from 10 days to two weeks.
In some cases, the treatment time may increase to 28 days.
This occurs with late congenital syphilis or in the third stage of the disease.
If you are intolerant to penicillins, use antibacterial drugs from other groups:
- Tetracyclines;
- Cephalosporins;
- Macrolides;
- Azalids.
Tetracyclines show high effectiveness against Treponema pallidum.
But it should be remembered that this drug is quite difficult for many people to tolerate.
Tetracyclines cannot be used to treat pregnant women.
This drug is toxic to the fetus.
Among cephalosporin antibiotics, only Ceftriaxone exhibits high activity against pathogens.
This drug is administered intramuscularly.
Novocaine cannot be used as a solvent.
It sharply reduces the antibacterial effectiveness of the drug.
It is optimal to dilute Ceftriaxone with water for injection.
Macrolides and azalides are other reserve drugs for the treatment of syphilis.
They are used in case of intolerance to other groups of antibiotics.
In addition, such antibiotics are prescribed when previous treatment is ineffective.
Macrolides are not used to treat neurosyphilis.
For this form of the disease, antibiotics of this group are ineffective.
Where to go if the test for syphilis is positive?
A dermatovenerologist treats syphilis.
You can contact such a specialist either free of charge or on a commercial basis.
Free treatment for citizens of the Russian Federation is carried out on the basis of services under the compulsory medical insurance policy.
You can contact a free dermatovenerologist at the dermatovenerology clinic at your place of residence.
If treatment at a municipal hospital is not possible, you should contact paid specialists.
The undoubted advantage of such observation will be maximum convenience for the patient.
In paid clinics, you can independently adjust your convenient appointment time.
Commercial medical institutions send tests for research to modern laboratories.
This ensures high speed of results readiness.
Self-medication for syphilis is unacceptable.
Without special knowledge and regular control tests, a person will only harm himself.
The Treponema pallidum strain is capable of developing resistance to antibacterial drugs.
This happens with incorrect and inadequate therapy.
In the future, all this will greatly complicate the treatment of the disease.
In severe cases, syphilis can become incurable.
Remember!
After completing the course of treatment, the patient remains under observation for some time.
During this period, he undergoes control tests and regularly consults with his doctor.
Such precautions are aimed at eliminating the possibility of relapse of syphilis.
Is RPR given to children?
A nonspecific antiphospholipid test can be performed on a person at any age.
This also applies to children.
This analysis is an analogue of the Wasserman reaction, only the RPR method was developed later.
The test allows you to determine immunoglobulins of classes G and M to a lipoprotein-like substance in patients with syphilis.
The study allows you to identify the primary disease or re-infection.
The substrate for the study is blood.
It will not be difficult for a doctor to collect fluid from a child.
Therefore, there are no age restrictions for manipulation.
Before taking the test, parents should prepare their child:
- The sampling should be carried out on an empty stomach; you should not feed the child before taking it;
- Active physical activity is not recommended half an hour before the procedure;
- do not take medications during the test;
- Children under 5 years old must drink up to 300 ml of water per half hour.
Parents follow these rules when preparing their child for RPR analysis.
It is very important to comply with everything, since improper preparation will distort the result of the study.
This will inconvenience parents and make them nervous.
It is better for adults to immediately fulfill all the conditions correctly.
When to do RPR for a child
A child should donate blood and undergo testing if there is a suspicion of Treponema pallidum infection.
There may be several situations.
The child was just born, the mother was sick with syphilis.
The baby should be tested for RPR in the maternity hospital to exclude intrauterine transmission of infection.
The child may develop congenital syphilis.
It is manifested by various developmental defects.
Clinical symptoms are noticeable immediately at birth.
Remember!
Sometimes they appear by the age of three years of the baby’s life.
The immune system of newborns and children is imperfect, the disease is dangerous.
At any age, a child is diagnosed with syphilis, including RPR analysis.
This happens if someone in the household is diagnosed with a disease.
Since children are at risk, they are examined immediately.
Such an analysis is required.
If there are any symptoms of syphilis in a baby, the disease is diagnosed immediately.
RPR analysis is one of the first to be done and is an accurate diagnostic method.
Children are more susceptible to infection from their parents than other people.
This happens because the immune system is not developed.
Syphilis RPR, anticardiolipin test
Syphilis (lues)
- an infectious disease caused by Treponema pallidum, transmitted mainly through sexual contact, prone to chronicity and affecting most organs and systems of the body.
RPR
is a nonspecific screening test (modification of RW) that detects immunoglobulins of the IgG and IgM classes against phospholipids released from damaged cells of a patient with syphilis.
The RPR test is recommended by order of the Ministry of Health of the Russian Federation for primary screening and monitoring the progress of syphilis therapy.
Antiphospholipid antibodies
Antiphospholipid antibodies detected by RPR are found in 70–80% of patients with primary syphilis and in almost 100% of patients with secondary and early latent syphilis. Most often, a positive RPR reaction is observed 3–5 weeks after infection or 7–10 days after the appearance of the primary chancre. In 90–98% of cases, after treatment for syphilis, the RPR test result becomes negative.
The RPR test is nonspecific, so false-positive reactions may occur. Antiphospholipid antibodies appear not only as a result of syphilis, but also in response to the development of non-treponemal diseases of an acute or chronic nature, in which tissue damage is observed (for example, in autoimmune diseases).
Upon receipt of a positive RPR test, the patient must be examined by a venereologist with a repeat blood test using a specific treponemal test to diagnose syphilis Treponema pallidum.
Rarely, RPR can give a false-negative result (this is due to an ultra-high titer of antiphospholipid antibodies); this situation is eliminated when RPR is prescribed simultaneously and the diagnosis of T. pallidum syphilis is performed. The combined use of the RPR test and the IgG/IgM ELISA test represents the best screening test for detecting or excluding syphilis at all stages.
Indications:
- initial examination for suspected syphilis (with confirmation of positive reactions in any treponemal test);
- diagnosis of latent syphilis (with confirmation of positive reactions in two treponemal tests);
- donor examination (in combination with treponemal test);
- screening examination.
Preparation
It is recommended to donate blood in the morning, between 8 am and 12 pm. Blood is drawn on an empty stomach, after 4–6 hours of fasting. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
Interpretation of results
Reference values: negative.
Positively:
- RPR - primary seropositive syphilis (infection occurred 1-3 months ago);
- secondary seropositive syphilis (infection occurred more than 3 months ago);
- tertiary seropositive syphilis (infection occurred more than 3–4 years ago);
- the first year after treatment of syphilis;
- seroresistance after treatment of syphilis;
- antiphospholipid syndrome is probable (if the test was used to diagnose antiphospholipid syndrome and syphilis is excluded);
- false positive reaction during: 1) pregnancy;
 2) diabetes mellitus; 3) tuberculosis; 4) oncological diseases; 5) autoimmune (systemic) diseases; 6) gout; 7) alcoholism; drug addiction; 9) carriage of non-syphilitic treponemes; 10) infectious mononucleosis; 11) enteroviral infections; 12) viral hepatitis; 13) pneumonia; 14) after vaccination.
2) diabetes mellitus; 3) tuberculosis; 4) oncological diseases; 5) autoimmune (systemic) diseases; 6) gout; 7) alcoholism; drug addiction; 9) carriage of non-syphilitic treponemes; 10) infectious mononucleosis; 11) enteroviral infections; 12) viral hepatitis; 13) pneumonia; 14) after vaccination.
Negative:
- absence of infection;
- early primary (seronegative) syphilis cannot be excluded;
- Late tertiary syphilis cannot be excluded.
The child has a positive answer: what to do?
If a child's PRP test is positive, parents do not need to panic.
This test is non-treponemal and does not detect Treponema pallidum in the blood.
The technique is not specific for detecting syphilis.
It is quite accurate, but there are errors in this analysis.
The mother should remember whether she properly prepared the child for blood donation.
A false positive result can be caused by several factors.
These include the baby’s medication intake, recent vaccinations, and illnesses.
But the presence of syphilis in a child should not be ruled out.
Parents with a baby should consult a doctor.
He will order other laboratory tests.
They will allow you to refute or confirm the disease.
Treponemal tests are aimed at detecting the pathogen itself.
They will allow you to accurately diagnose the disease.
They will detect if the bacteria is in the body.
In this case, you need to start treatment immediately.
Your doctor will prescribe drug therapy.
Interpretation of analysis results (for specialists!*)
The result of the study is qualitative.
RMP is positive in primary syphilis in 59-87% of cases, secondary - 100%, late latent - 79-91%, tertiary - 37-94%. RMP is usually negative in the first 7-10 days after the appearance of chancre.
To differentiate congenital syphilis from passive carriage of maternal infection, newborns need to undergo a series of studies to determine the antibody titer: a rise in titer within 6 months after birth indicates congenital syphilis, while with passive carriage, antibodies disappear by the third month.
When assessing the results of bladder cancer in infants with congenital syphilis, it is necessary to remember the prozone phenomenon. The essence of this phenomenon is that for agglutination of antigens and antibodies in these reactions it is necessary that antigens and antibodies be in the blood in appropriate quantities. When the number of antibodies significantly exceeds the number of antigens, agglutination does not occur. In some infants with congenital syphilis, serum antibody levels are so high that undiluted serum does not agglutinate the antibodies and nontreponemal antigens used to diagnose syphilis (BC is nonreactive). Therefore, in children examined for the purpose of diagnosing congenital syphilis, the prozone phenomenon may occur.
False-positive bladder cancer can be:
- for rheumatic diseases (SLE, rheumatoid arthritis, scleroderma);
- infections (mononucleosis, malaria, mycoplasma pneumonia, active tuberculosis, scarlet fever, brucellosis, leptospirosis, measles, mumps, lymphogranuloma venereum, chicken pox, trypanosomiasis, leprosy, chlamydia);
- pregnancy (rare);
- in old age (about 10% of people over the age of 70 years may have a false-positive MR);
- chronic lymphocytic thyroiditis, hemoblastosis, taking certain antihypertensive drugs, with hereditary or individual characteristics.
To interpret the study results, contact your doctor!
Reference values (norm): not detected.
* Interpretation of the results is intended for your attending physician, who will determine an accurate diagnosis and prescribe a treatment regimen, taking into account the results of not only this analysis, but also the entire range of studies for your specific case. Do not diagnose yourself - be sure to consult a doctor!
Positive RPR in an elderly person: why?
In older people, the body wears out over the years.
It is rare to meet a completely healthy elderly person.
Many pensioners have chronic diseases, and malignant neoplasms are not uncommon.
Such diseases may give a positive PRP test reaction.
This is not a very specific study and is not a treponemal test.
Therefore, the pathogen itself is not looked for with this technique.
And antibodies against other diseases can masquerade as syphilis.
But there is no need to rule out syphilis; the person may have it.
To determine the presence of Treponema pallidum in an elderly person, additional tests need to be performed.
In any case, if a positive RPR test is detected, it is recommended to visit a doctor.
The patient then undergoes one of the treponemal tests for an accurate diagnosis.
It will identify bacteria in the blood.
This will be a reliable, accurate sign of infection.
Syphilis is a serious sexually transmitted infection.
It requires immediate treatment.
The disease occurs at any age from children to the elderly.
Is RPR done in a public clinic?
This test is common in private medical centers and laboratories.
Conducting such a study is possible in a regular clinic.
The study is performed as a screening method.
It all depends on the installed equipment.
The laboratory technician chooses the specific method of conducting the examination.
Therefore, the doctor will not be able to guarantee that testing will be performed using one method or another.
RPR analysis is also performed in large scientific centers or specialized high-pressure chambers.
The person decides where to go.
Visiting a private laboratory will not always be convenient.
The patient will have to go to another institution after consulting a doctor.
Then you need to take the test result and go to the doctor again.
It is more convenient to contact a dermatovenerologist at a specialized medical center.
There, a specialist will conduct a consultation and immediately refer you for research.
In our center, tests are carried out as quickly as possible.
Dermatovenerological clinics and scientific institutes have highly qualified personnel.
There is no doubt about their competence.
RPR blood test - interpretation of the result
This study is qualitative, not quantitative, so after conducting it you can get only 2 results - positive and negative.
If the result is positive, the doctor makes a conclusion about the possible development of syphilis.
He orders an additional in-depth study.
Which consists in determining antibodies directly to the causative agent of syphilis (usually performed using ELISA - enzyme-linked immunosorbent assay) and other tests.
This is necessary due to the fact that the RPR blood test is a nonspecific reaction.
Therefore, the appearance of antiphospholipid antibodies may indicate the development of other diseases (autoimmune processes, tuberculosis, systematic use of psychoactive substances, HIV infection).
If the RPR analysis is negative, then it has several interpretations:
- I. The causative agent of syphilis is absent in the body.
- II. After infection, a short period of time passed during which the accumulation of antiphospholipid antibodies had not yet occurred. It is recommended to take the test again after 1.5-2 weeks.
- III.Tertiary syphilis, in which 30% of patients may not have specific antiphospholipid antibodies in the blood.
The need for additional research in case of a negative PRP analysis is determined by the venereologist on an individual basis.
Based on data from a clinical examination of the patient (questioning, examination of the skin and mucous membranes, palpation of regional lymph nodes).
If you need an examination for syphilis, contact the author of this article - a venereologist, a urologist in Moscow with 15 years of experience.
References
- Guyton, A., Hall, J. Medical physiology / ed. IN AND. Kobrina. - M.: Logosfera, 2008. - 1296 p.
- Internal diseases in 2 volumes: textbook / ed. ON THE. Mukhina, V.S. Moiseeva, A.I. Martynova, 2010. - 1264 p.
- Reshetnyak, T.M. Antiphospholipid syndrome: diagnosis and clinical manifestations (lecture). Scientific and practical rheumatology, 2014. - No. 1.
- Secrets of rheumatology. St. Petersburg : “Publishing house BINOM”, 1999. - 768 p.
- Despierres, L., Beziane, A., Kaplanski, G. et al. Contribution of anti-β2glycoprotein I IgA antibodies to the diagnosis of anti-phospholipid syndrome: potential interest of target domains to discriminate thrombotic and non-thrombotic patients. Rheumatology, 2014. - Vol. 53(7). — P. 1215–1218.
- Frodlund, M., Vikerfors, A., Grosso, G. et al. Immunoglobulin A anti-phospholipid antibodies in Swedish cases of systemic lupus erythematosus: associations with disease phenotypes, vascular events and damage accrual. Clin Exp Immunol., 2021. - Vol. 194(1). — P. 27-38.
 2) diabetes mellitus; 3) tuberculosis; 4) oncological diseases; 5) autoimmune (systemic) diseases; 6) gout; 7) alcoholism; drug addiction; 9) carriage of non-syphilitic treponemes; 10) infectious mononucleosis; 11) enteroviral infections; 12) viral hepatitis; 13) pneumonia; 14) after vaccination.
2) diabetes mellitus; 3) tuberculosis; 4) oncological diseases; 5) autoimmune (systemic) diseases; 6) gout; 7) alcoholism; drug addiction; 9) carriage of non-syphilitic treponemes; 10) infectious mononucleosis; 11) enteroviral infections; 12) viral hepatitis; 13) pneumonia; 14) after vaccination.