Uterine fibroids are a tumor disease of the female reproductive system. It occurs in every fifth patient over 30 years of age and is often asymptomatic. Ultrasound examination will help identify the disease and prescribe treatment. In order for the ultrasound results for fibroids to be as accurate as possible, it is necessary to properly prepare for the procedure.
How are uterine fibroids determined by ultrasound?
When to do an ultrasound to get the right result
If fibroids are found, how often should an ultrasound be done?
Ultrasound for fibroids in a paid clinic
Submucous (submucosal) uterine fibroids
Such nodes are located under the mucous membrane and grow into the uterine cavity. Submucosal fibroids are the most unpleasant in terms of symptoms, since they lead to heavy periods, during which a woman loses a lot of blood, uterine bleeding, infertility, miscarriages, and premature birth.
A small nodule—only 2–3 cm in diameter—can lead to severe symptoms. Sometimes the bleeding is so severe that the woman has to be hospitalized and receive a blood transfusion.
Chronic bleeding from submucosal fibroids leads to anemia. Characteristic manifestations of this condition: pallor, constant feeling of fatigue and weakness, headaches and dizziness, shortness of breath, tinnitus, fainting, rapid heartbeat.
Causes of the disease
As with fibroids of other localizations, the main etiological factor in the appearance of benign cervical tumors is hormonal imbalance. Until recently, scientists considered the main cause of fibroids to be an increased amount of estrogen in the body. However, recent studies have demonstrated that excess progesterone also plays an important role in the development of uterine fibroids. You need to understand that excess hormones are important only in the early stages of fibroid growth. After reaching 3-4 cm in diameter, the tumor acquires the ability to autonomously regulate growth.
In addition to hormonal imbalance, the appearance of fibroids is promoted by:
- traumatic childbirth, accompanied by ruptures of cervical tissue;
- frequent instrumental abortions;
- diagnostic and therapeutic interventions accompanied by cervical dilatation;
- acute and, especially, chronic endocervicitis;
- absence of childbirth or late birth of the first child;
- refusal of breastfeeding;
- burdened heredity;
- uncontrolled use of hormonal drugs;
- early puberty and late cessation of menstruation;
- diseases of the endocrine glands;
- obesity.
In addition, excessive psycho-emotional stress plays an important role in the development of fibroids.
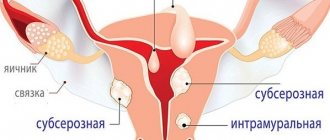
Subserous fibroid
Unlike submucosal nodes, subserous nodes are usually “quiet”. They can grow large without causing symptoms. When people talk about giant fibroids, the size of a melon or a watermelon, they are usually talking about subserous nodes. They grow outward into the abdominal cavity - there is much more space there than in the uterine cavity.
When a subserous myomatous node, which can be located on the anterior or posterior wall of the uterus, reaches a large size, it begins to compress neighboring organs: the bladder, rectum. A woman is worried about frequent urination and constipation.
Risk group
Most often, fibroids appear in women during pregnancy and the premenopausal period. This is explained by the fact that fibroids are a hormone-dependent tumor and occur when the hormonal balance in the body is disturbed.
In some women, upon the onset of menopause or after childbirth, fibroid nodes sharply decrease or even disappear altogether. However, counting on a favorable course of the disease is a frivolous matter, since nutrition in the fibroid node can be disrupted at any time, which will lead to dangerous changes. The acute form of the disease is characterized by pain, rapid tumor growth (due to edema), and symptoms of intoxication. In this case, immediate surgery to completely remove the uterus is required.
The larger the node, the higher the risk of pathological changes. The size of fibroids - a disease that leads to infertility or miscarriages - is, bitterly ironically, usually measured in weeks of pregnancy, by analogy with the size of the developing fetus. The method of treatment depends on the size of this tumor.
Intramural fibroids
Intramural, or interstitial, uterine fibroids are located in the thickness of the organ wall. By and large, all nodes initially grow as intramural, closer to the cavity or outer surface of the uterus, but then they begin to predominantly protrude into the uterine cavity or towards the abdominal cavity, depending on the nature of growth.
Until interstitial fibroids reach a critical size, they usually do not cause symptoms. In the future, it can begin to protrude into the uterine cavity and lead to uterine bleeding, like submucosal nodes.
What is fibroid?
Myoma is a tumor that forms in the muscular layers of the uterus. This tumor often develops very slowly. There are the following types of fibroids:
- subserous (forms under the upper layer of the uterus, and development proceeds towards the abdominal cavity);
- interstitial (grows inside the muscular layer of the uterine cavity);
- intraligamentous (formed in the uterus between the broad ligaments);
- submucous (appears under the mucous layer of the uterus, development - into its lumen);
- cervical (grows in the muscles of the cervix).
As fibroid nodes grow, the size of the uterus itself increases, just as during pregnancy. This is the reason that the size of fibroids is usually indicated in weeks (5, 8, 12, 16 weeks, etc.), similar to the gestational age, which corresponds to the size of the uterus. For example:
- Uterine fibroids
were diagnosed . That is, the size of the uterus has increased to the same size as during pregnancy at 12 weeks; - Uterine fibroids at 16 weeks
correspond to the size of the uterus at 16 weeks of pregnancy.
There are also cases when not one node is identified, but several at once, and their size may vary. This is called multiple uterine fibroids.
The neoplasm grows and develops under the influence of female sex hormones. Because of this, due to a decrease in the level of sex hormones in the female body (after menopause). It should also be noted that fibroids often decrease in size, and sometimes may disappear altogether.
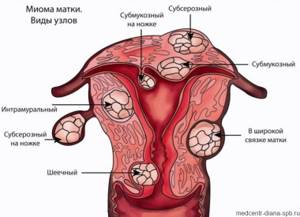
Classification of the International Federation of Obstetrics and Gynecology
The division of myomatous nodes into three types - submucosal, intramural and subserous - is a somewhat simplified classification. In fact, fibroids can occupy different positions and protrude to varying degrees into the uterine cavity or abdominal cavity. In order to cover all options, the International Federation of Obstetrics and Gynecology has developed a special classification. In accordance with it, ten types of fibroids are distinguished:
Submucosal nodes:
- Type 0 is a pedunculated submucosal fibroid located in the uterine cavity.
- Type 1 - the node protrudes into the uterine cavity by more than half.
- Type 2 - the node protrudes into the uterine cavity by less than half.
Other types:
- Type 3 is an intramural fibroid that does not protrude into the uterine cavity, but is adjacent to its mucous membrane.
- Type 4 is an intramural fibroid, which is located deep in the muscles.
- Type 5 is an intramural subserosal node that protrudes less than half of the way out on the surface of the uterus.
- Type 6 is an intramural subserosal node that protrudes more than half of the surface of the uterus.
- Type 7 is a pedunculated subserosal node that is entirely above the surface of the uterus.
- Type 8 - fibroids that have a specific localization (for example, in the cervix).
- Hybrid nodes that affect both the mucous membrane of the uterus and its outer surface. They are designated by two numbers.
The best treatment is prevention
To prevent the development of the disease, it is necessary to regularly, at least twice a year, be examined by a gynecologist and conduct a routine ultrasound examination. This is especially true for women at risk. Myoma often occurs against the background of infertility, repeated miscarriages, menstrual dysfunction, genital infections, and endometriosis. Excess weight, a sedentary lifestyle and a lot of stress are also provoking factors.
The development of this benign tumor is largely influenced by inflammatory diseases and abortions. Uterine fibroids are much more common in nulliparous women. In 30–40% of cases, the tendency to form uterine fibroids is inherited: from mother to daughter. There are so-called “familial forms” of fibroids, when all women in the family suffer from this disease.
It is possible to detect fibroids in the first and second stages, when the rudiments of future nodes begin to form, only with the help of microscopic examinations. From the beginning of fibroid growth to the appearance of the first symptoms, it can take from 5 to 8 years. At the third stage, nodes can already be detected during inspection. To do this, the doctor palpates the abdomen and conducts a vaginal examination. A more informative method - ultrasound of the pelvic organs - allows you to more accurately determine the location, size and condition of the nodes, as well as classify fibroids. Uterine fibroids are also detected using computed tomography (CT) or magnetic resonance imaging (MRI).
Classification depending on the number of fibroids
Depending on the number of nodes, there are three types of fibroids:
- Single - 1-2 nodes, which can have different sizes.
- Multiple. More than 3 nodes are detected. Treatment usually helps reduce symptoms, but it is often not possible to remove all fibroids, and some may grow large over time.
- Mixed. There are many fibroids, but at least one of them is large and dominant. For example, multiple fibroids with a large subserous node may be diagnosed. It can be removed, but another node may grow strongly in the future. Multiple and mixed fibroids pose a particularly big problem in women of reproductive age before menopause, since sex hormones promote the growth of nodes.
Tactics for choosing a treatment method for uterine fibroids
The problem of treating patients with uterine fibroids continues to be an urgent problem in modern gynecology, due to the high frequency of this pathology (20-30%), as well as due to its negative impact on the reproductive system and the general health of women. The pathogenetically based concept of treating this disease is a combined effect - surgical and medicinal. Therefore, despite the emergence of new surgical technologies (the use of endoscopic techniques, minilaparotomy, uterine artery embolization, lasers, electro- and cryosurgery), hormonal therapy has not yet lost its significance. For this purpose, gonadotropin-releasing hormone agonists (a-GnRH), gestagens, androgens, and antiandrogens are currently widely used.
Where in St. Petersburg can you treat uterine fibroids without surgery?
At the Diana Clinic, gynecologists have extensive experience in diagnosing and treating uterine fibroids of various locations. If the presence of this neoplasm is suspected, patients are prescribed a full range of studies to determine treatment tactics.
We use only safe, modern techniques that allow us to completely restore a woman’s sexual and reproductive health. You can make an appointment with a gynecologist at a convenient time - the clinic is open seven days a week and without lunch breaks.
CLICK TO SIGN UP
If you find an error, please select a piece of text and press Ctrl+Enter
Worth being wary
If you do not start timely treatment of subserous uterine fibroids, you can get a frightening chain of facts that follow and follow from each other:
- Torsion of the tumor stalk.
- Lack of nutrition for the nodular neoplasm.
- Necrosis of nodule tissue.
- The occurrence of a purulent-inflammatory process in nearby structures.
The body will signal such complications in the form of acute pain, fever, dizziness, increased sweating, and weakness. All this is a reason to contact the clinic as soon as possible.
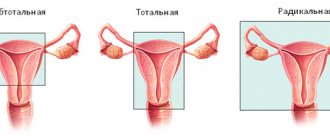
Drastic measures
Today, when treating fibroids, doctors try to avoid such a radical method as removing the uterus (hysterectomy). After all, this organ plays an important role in a woman’s endocrine system. In addition, its removal may cause psychological trauma to the patient. After a hysterectomy, some women may experience disturbances in hormonal levels and vegetative-vascular regulation, and the risk of developing dangerous diseases increases.
Myomectomy is an alternative method in which only part of the uterus is removed along with fibroids. Myoma less than 10 weeks old can be removed without incisions - laparoscopically (through 3 punctures of the abdominal wall). Unfortunately, in 30% of cases after myomectomy, nodes recur.
Uterine artery embolization (UAE) is a relatively new effective method of combating fibroids, after which this tumor can no longer regenerate.
This technique is used for fibroids of almost any size. The advantages of embolization include minimal invasiveness and a short recovery period. As a result of this procedure, fibroid nodes are reduced by 50–80% and no longer grow.
A scalpel and general anesthesia are not required - the procedure is performed under local anesthesia. In this case, the uterus is not removed or cut, which means that the patient retains reproductive function. The patient spends only three days in the hospital. By puncturing the femoral artery, a catheter with a diameter of 1.5 mm is inserted into the vessel, which is advanced into the uterine artery. The catheter transmits tiny (up to 0.5 mm) embolization particles made from an inert medical polymer into the uterine artery. These particles cover the entrances and exits of the vessels that feed the fibroids.
As a result, the tumor is replaced by scar tissue and shrinks or disappears. In this case, the healthy part of the uterus is not affected.
Characteristic signs
Nodular subserous uterine fibroids make themselves felt only if the size of the tumor increases and there is pressure on the tissues and organic systems located next to this formation.
Symptoms of subserous uterine fibroids:
- increased incidence of constipation;
- formation and inflammation of hemorrhoids;
- painful urination, frequent urge to go to the toilet;
- increased sweating;
- dizziness;
- pain in the lower abdomen and lower back (while standing or sitting);
- aching pain in the lower abdomen, lumbar spine, pubic area.
Prolonged standing and significant physical activity can lead to the fact that when subserous uterine fibroids are diagnosed, its symptoms begin to manifest themselves more clearly, for example, increased or modified pain. Unpleasant sensations can become cramping and debilitating; this may indicate tumor growth, torsion of the leg or a change in location.
If you discover signs of subserous uterine fibroids, you should contact a gynecologist to clarify the diagnosis and under no circumstances self-medicate.
Symptoms of fibroids
In approximately 20-30% of cases, symptoms of uterine fibroids are not expressed. The disease is detected by chance during a preventive medical examination or during an ultrasound scan prescribed for completely different reasons.
The presence of uterine fibroids can be suspected if:
- Increased menstrual bleeding, in which clots often appear.
- The appearance of acyclic (irregular, outside the cycle) bleeding of varying intensity.
- the occurrence of pain in the lower abdomen, a feeling of heaviness or discomfort.
- Pain during sexual intercourse.
- Miscarriages (miscarriages), missed pregnancies and infertility.
The pain becomes most intense when a complication occurs in the form of torsion of a subperitoneal myomatous node. The doctor can feel the large size of the tumor by pressing on the abdomen.
Treatment
To effectively combat a benign tumor, the attending physician must take into account all the points: the growth rate of nodular formations, their location, the patient’s age, and her state of health.
Monitoring fibroids is one of the main points in carrying out therapeutic measures. If there is no growth and a threat to vital organs, the tumor can be left at the control level (ultrasound after three months).
Treatment of subserous uterine fibroids with medium and slow rates of emergence of new tumors consists of taking hormonal drugs and carrying out symptomatic therapeutic measures.
The administration of hormones can act as a deterrent and stop (in some cases reduce the size of the tumor) the process.