PCR diagnostics of herpes virus (HERPES SIMPLEX VIRUS 1,2)
A study to identify the causative agent of herpes viral infection types 1 and 2 (HerpesSimplexVirus 1.2), during which the genetic material (DNA) of the herpes simplex virus is determined using the real-time polymerase chain reaction (RT-PCR) method.
Research method
Real-time polymerase chain reaction.
What biomaterial can be used for research?
Venous, capillary blood, cerebrospinal fluid, smear from the pharynx (oropharynx), urogenital scraping, urogenital scraping with prostate secretion, saliva, scraping, the first portion of morning urine, ejaculate.
How to properly prepare for research?
- Women are recommended to donate biomaterial (urogenital smear or urine) before menstruation or 2 days after its end. You should not urinate for 2 hours before taking a urogenital smear. Do not wash yourself before the examination.
- Men should not urinate for 2 hours before taking a urogenital smear or urine test. Do not wash yourself before the test.
General information about the study
The most common are types 1 and 2 of herpes. Both are contagious and contribute to the appearance of small bubbles (vesicles) on the mucous membranes, which burst, forming open wounds. With HSV-1, blisters appear around the mouth and in the oral cavity, while HSV-2 usually affects areas around the genital area.
The herpes simplex virus is sexually transmitted and can be transmitted through skin-to-skin contact in the presence of vesicles on the skin, and sometimes in the absence of visible lesions on the skin.
What is the research used for?
- To detect herpes viral infection of the genital organs in men and women and monitor its treatment.
- To check a woman for herpes before and during pregnancy.
What do the results mean?
Reference values: negative.
Positive result
- The body is infected with a virus.
Negative result
- Most often, there is no infection of the genitals with the herpes virus.
What can influence the result?
- Antiviral therapy can reduce the amount of virus in epithelial cells, however, due to the high sensitivity of the PCR method, this rarely leads to false negative results.
Important Notes
- Herpes is most dangerous for newborns who are infected from their mother, and for patients with weakened immune systems.
- The herpes simplex virus in combination with the papilloma virus increases the risk of developing cervical cancer.
Herpes
11Mar To the list of articles 12442
Category: Pregnancy and childbirth, Gynecology, Urology
— Natalia Nikolaevna, let’s start, as they say, with the basics. What is herpes and why does it appear in humans?
— The disease is caused by viruses - very ancient microorganisms that can adapt and survive in various conditions. Today, scientists count more than a hundred representatives of the herpes virus, but of this number, only eight are found in humans.
the source of a herpes viral infection is a patient or a virus carrier who can transmit the virus by contact, airborne droplets, blood transfusion, or during pregnancy from mother to fetus. Once the pathogen enters the body, it remains there for life.
— Is this disease contagious?
— In 40% of cases, primary infection with the herpes simplex virus occurs in early childhood, and the source, as a rule, is family members who have signs of herpes infection. To penetrate the body, the virus does not have any big problems; microtrauma on the skin or mucous membrane is enough. From the site of entry into the body, the virus moves along nerve fibers to the central organs of the nervous system.
— Where is herpes most common?
— The most famous is fever on the lips, which is caused by herpes type I, with the blood flow it penetrates into the brain and trigeminal nerve nodes. It can also affect the eyes, which leads to blindness, the larynx, pharynx - herpetic sore throat. Often severe pain occurs along the trigeminal nerve, in the ear canal, jaw, pain syndrome such as cervical radiculitis or angina.
Another known localization is genital herpes, or herpes type II. The virus hides in the nerve cells of the lumbar region, which are the reservoir of the disease. As soon as immunity decreases, the virus awakens and along the same nerve fibers again enters the skin and mucous membranes - this is how a relapse begins. Herpes type II causes damage to the genital organs. Women who are carriers of this virus often cannot get pregnant, carry and give birth to a healthy child, they experience miscarriages or the birth of children with defects. Reproductive function also suffers in men - sperm maturation is disrupted, urethritis and prostatitis develop. Moreover, sperm can be carriers of viral genes. Genital herpes can cause severe pain in the perineal area in both women and men. During an exacerbation, there can be no question of a normal life, exhausting pain and rashes disrupt the normal rhythm, the psycho-emotional sphere suffers - depression occurs.
-What if herpes appeared during pregnancy?
— A pregnant woman who once suffered a herpes infection has antibodies to it. If an exacerbation develops, then it can be successfully treated. But the appearance of rashes on the genitals on the eve of childbirth may be an indication for a cesarean section. This will give the baby the opportunity to avoid exposure to the virus at birth.
If a woman gets herpes for the first time during pregnancy, especially in the early stages, this can contribute to the development of a severe intrauterine infection in the child with multiple lesions.
— You mentioned eight types of herpes virus, what other diseases can they cause?
— The most famous is cytomegalovirus infection, it is caused by type V herpes virus. The salivary glands are affected, the kidneys, bone marrow, lymph nodes, gastrointestinal tract, genitals, blood cells, and nervous system can be infected. The pathogen is usually isolated from saliva, urine, semen, genital secretions, and breast milk.
The group of herpes viruses also includes the Epstein-Barr virus, which causes the development of infectious mononucleosis. The causative agent of this disease is transmitted in the same ways as other herpes viruses, but most often with saliva. Therefore, by kissing a person infected with mononucleosis or using his dishes or towel, you are highly likely to become infected with this virus. the first signs of the disease - fever, sore throat, loss of strength, swollen lymph nodes - may not appear immediately, but 2 months after the virus enters the body. With infectious mononucleosis, the liver and spleen are always affected - they increase in size and become painful when pressed.
The herpes zoster virus is the cause of chickenpox in children and shingles in adults, and the skin rash can go away in one month, but pain along the nerves will remain for years.
All herpes viruses have oncogenic activity; they are dangerous for humans because, by multiplying in the cells of various organs and blood, they lead to a decrease in immunity.
— Does herpes infection always manifest as rashes?
— Quite often it occurs latently, that is, without clinical manifestations. Exacerbations can be triggered by hypothermia, excessive exposure to the sun or solarium - insolation, stress. The frequency and intensity of exacerbations of recurrent herpes depend on the virulence of the pathogen and the state of the human immune system. The disease can be local in nature, that is, blistering rashes on the skin and mucous membranes, or widespread.
If, along with herpetic rashes, a person experiences general weakness, malaise, low-grade fever, enlarged and painful lymph nodes, this indicates dissemination - prevalence - of the infectious process. This is very dangerous for the health and life of the patient.
Currently, atypical, non-vesicular forms of herpes, especially genital, are often encountered: colpitis, endocervicitis - inflammation of the cervix, swelling, hyperemia in the genital area, accompanied by pain, and sometimes only itching. In such cases, it is necessary to consult a doctor and be examined not only for urogenital infections, but also for the herpes virus.
— What examination for the herpes virus is usually prescribed?
— The main and most reliable method for diagnosing sexually transmitted diseases, including the herpes virus, is PCR diagnostics, that is, determining the DNA of the virus.
(based on materials from the newspaper “Health”, correspondent Elena Maryina)
Share
Tweet
Our advantages
- Own PCR diagnostics department;
- In the laboratory diagnostics department of the National Medical Research Center of Oncology named after. N. N. Petrova, the PCR diagnostics department is geographically located on the basis of the bacteriological laboratory, which allows us to combine diagnostic search efforts and reduce the time required to identify the causative agent of the infectious process.
- Material for PCR can be submitted to the CDC, which is located in the city center near the metro.
- Convenient operating hours of the Center - daily, including on public holidays, on weekdays from 9.00 to 20.00, on weekends until 18.00.
- The material is collected by experienced and qualified specialists.
What factors predispose cancer patients to infection?
- Neutropenia
- Disorders of cellular and humoral immunity
- Damage to anatomical barriers, mainly mucous membranes and skin
- Tumor obstruction
- Various invasive procedures, etc.
The most common causative agents of viral infections in cancer patients:
- herpes viruses (herpes simplex virus, Varicella-Zoster virus, cytomegalovirus, etc.)
- common respiratory viruses (respiratory syncytial virus, influenza A and B viruses, parainfluenza viruses, etc.).
Molecular Biological Research
Real-time polymerase chain reaction (Real Time PCR) is the highest quality and fastest research method. The PCR method is universal - one portion of biological material allows you to conduct research for the presence of pathogens of a number of diseases.
Why is PCR diagnostics so valuable?
One of the significant advantages of the PCR method is its high sensitivity - from 95 to 100%.
PCR in the diagnosis of infections
The advantages of the PCR method (sensitivity and specificity) determine a wide range of applications in modern medicine. The PCR method is automated and allows you to obtain analysis results within one business day. PCR is used in obstetrics, gynecology, neonatology, pediatrics, urology, venereology, nephrology, infectious diseases clinic, ophthalmology, neurology, phthisiopulmonology, etc.
- The main areas of application of PCR diagnostics:
- 1. diagnosis of acute and chronic infectious diseases of various localizations
- 2. monitoring the effectiveness of therapy
- 3. clarification of the type of pathogen
The PCR method makes it possible to diagnose many infectious diseases with a complex serological picture, determine the “viral load” in the patient’s blood, and identify dysbiosis of the urogenital tract in women and men.
The main focus is DIAGNOSIS of sexually transmitted infections (STIs).
Bacterial (gonorrhea, chlamydia, ureaplasmosis, mycoplasmosis, gardnerellosis), viral (herpes, cytomegalovirus, hepatitis), protozoal (trichomoniasis) and fungal (candidiasis) infections can be sexually transmitted.
For a quick, complete and inexpensive diagnosis of sexually transmitted infections, a comprehensive PCR analysis was developed for 6, 10 and 11 main pathogens.
- Molecular biological studies using real-time PCR:
- Diagnosis by real-time PCR of bacterial and viral infections of the urogenital tract;
- Complete screening study by PCR for 11 infections (mycoplasma hominis, mycoplasma genitalium, ureaplasma urealyticum/parvum, gardnerella vaginalis, neisseria gonorrhea, chlamydia trachomatis, trichomonas, candida albicans, cytomegalovirus, herpes simplex virus, Epstein-Barr virus);
- Abbreviated screening study using PCR for 6 infections (mycoplasma hominis, mycoplasma genitalium, ureaplasma urealyticum/parvum, gardnerella vaginalis, chlamydia trachomatis, trichomonas);
- Screening study using PCR for 6 infections in ENT diseases (mycoplasma hominis, chlamydia trachomatis, candida albicans, cytomegalovirus, herpes simplex virus, Epstein-Barr virus);
- Diagnosis by real-time PCR of viral infection in blood and tissues;
- Real-time PCR diagnostics of clinically significant levels of human papillomavirus infection and genotyping;
- Diagnosis by real-time PCR of viral hepatitis, their genotyping (qualitative and quantitative determination);
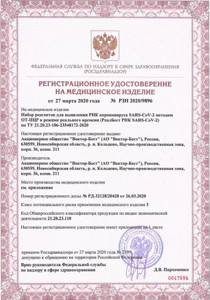
- Detection of SARS-CoV-2 coronavirus RNA using real-time RT-PCR. (

,
,
). - Determination of IL28B gene polymorphism associated with resistance to interferon and ribavirin therapy in patients with hepatitis C, genotype 1B. Identification of factors influencing the success of treatment, including genetic ones, is of great importance, both for the doctor, who needs objective criteria for predicting the effectiveness of treatment, and for the patient, who, before starting standard therapy, must be informed about the likelihood of its success and side effects antiviral drugs used. Determining the patient's genotype for IL28B will help in making a decision on the use of a standard course of treatment for chronic hepatitis C with PEG IFN/RIB and, if necessary, individual optimization of therapy by including protease inhibitors - telaprevir and boceprevir.
- Molecular genetic studies using real-time PCR molecular genetic studies that identify predisposition to various diseases
- For healthy, successful people who have made it a rule to plan their lives and calculate all possible risks, including health-related risks.
- For caring parents who want to assess the risk of certain diseases in their children.
- For expectant mothers seeking to minimize threats to the normal development of the fetus.
- For people with a hereditary history of cancer, cardiovascular and other diseases who want to know how great the risk of these diseases is for them.
- Molecular genetic diagnosis of hereditary predisposition to widespread diseases (osteoporosis, diseases associated with calcium metabolism disorders, obesity, hypertension, diseases associated with folate cycle disorders and the risk of developing thrombophilia).
- The main direction of the laboratory's work is the study of genetic factors of predisposition to thrombophilia. Thrombophilia is a pathological condition of the body characterized by an increased tendency to intravascular thrombus formation due to a congenital, hereditary or acquired disorder of the hemostasis system, leading to the loss of one of its main functions - maintaining circulating blood in a liquid state.
- A study of genetic predisposition to thrombophilia is indicated in the following cases:
- A history of two or more early pregnancy terminations;
- A history of severe pregnancy complications (preeclampsia, fetal growth retardation, intrauterine fetal death);
- The presence of relatives with thrombotic manifestations under the age of 50 years (myocardial infarction, stroke, pulmonary embolism, deep vein thrombosis of the lower extremities, etc.);
- Several unsuccessful IVF attempts;
- Increased levels of antiphospholipid antibodies and/or homocysteine;
- Planning of gynecological surgical interventions;
- Prescription of oral hormonal contraceptives (OCs). Women with an episode of venous thromboembolism receiving oral contraceptives;
- Prescribing hormone replacement therapy. Women with an episode of venous thromboembolism receiving hormone replacement therapy;
- Smoking men under 50 years of age with an episode of venous thromboembolism;
- The presence of thrombophlebitis.
- hereditary predisposition to hypertension,
- genetic predisposition to hypertension and atherosclerosis,
- genetic predisposition to obesity with impaired lipoprotein metabolism,
- disorders of calcium metabolism,
- hereditary predisposition to osteoporosis,
- genetic predisposition to the development of breast and ovarian cancer of the BRCA1 and BRCA2 genes.
- Determination of genetic polymorphisms:
Schedule for issuing results of molecular biological and cytogenetic studies |
| PCR research for 2-4 working days Thrombosis + folates (code 73038), hypertension (code 73044), obesity (code 74044B) – 7 working days Interleukin (code 73045) – results are issued every Thursday Calcium metabolism (code 7061) – 4 working days BRCA (code 73039), osteoporosis (code 74063), extended panel (73060) – 14 working days The day of material collection does not count Cytogenetic studies are completed within 14-18 working days |
Back
share information
0
Social buttons for Joomla
Human Herpes Virus 6, IgG
IgG antibodies to human herpes virus type 6 (HHV-6) are produced by the immune system starting from the second week after infection with the virus and persist throughout life. Their detection provides reliable evidence of HHV-6 infection.
What is this analysis used for?
To establish HHV-6 infection and the nature of the infection:
- primary infection (acute course, latent course, carriage),
- secondary infection (chronic course, exacerbation/relapse, reinfection).
When is the study scheduled?
- In the differential diagnosis of childhood infections occurring with high fever and rash.
- When diagnosing infectious mononucleosis negative for the Epstein–Barr virus.
- In a complex of examinations of patients with lymphoproliferative diseases and hematological malignancies.
- In a complex of examinations of organ and tissue recipients before and after transplantation.
- When diagnosing virus-associated diseases in HIV-infected people and other immunodeficiency conditions (chronic fatigue syndrome).
Synonyms Russian
IgG class antibodies to HHV-6, class G immunoglobulins to human herpes virus type 6.
English synonyms
Anti-HHV-6 IgG, Human Herpes Virus type 6 IgG antibodies, Anti–Human Herpes Virus 6 IgG, HHV-6 Antibodies.
Research method
Enzyme-linked immunosorbent assay (ELISA).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before donating blood.
General information about the study
Human herpes virus type 6 (HHV-6) was first isolated relatively recently, in 1986 (in the blood cells of patients infected with HIV). It has now been established that HHV-6 infection is widespread and has 2 subtypes - A and B - which differ genetically and epidemiologically: subtype B is more common, and subtype A is usually found in patients with immunodeficiencies. Subtype B is the main cause of sudden exanthema, a childhood illness accompanied by high fever and rash. In addition, the herpes virus can be asymptomatic and in the form of a nonspecific febrile illness. In some cases, complications from the central nervous system are observed (convulsions due to high fever, rarely other neurological complications, including encephalitis, meningoencephalitis, serous meningitis).
IgG antibodies to this virus are detected in 70-90% of adults. Primary HHV-6 infection in adults is rare and may be associated with fulminant hepatitis or infectious mononucleosis negative for the Epstein–Barr virus.
The most likely route of transmission of infection is airborne droplets, with saliva; “vertical” transmission is not excluded - from mother to child during pregnancy. The virus tends to infect lymphocytes. Replication of the virus occurs mainly in T-lymphocytes, but it can also be detected in other cells - monocytes, B-lymphocytes - as well as in brain tissue, liver, salivary glands, and endothelium.
Like other herpes viruses, HHV-6 after primary infection is able to persist in the body, becoming activated when the immune system is suppressed. Stem cell transplantation and internal organ transplantation increase the risk of infections caused by HHV-6 (in most cases, this appears to be due to reactivation of latent infection as a result of immunosuppression during immunosuppressive therapy).
Testing for HHV-6, along with testing for cytomegalovirus and Epstein–Barr virus, is recommended for the earliest possible detection of virus-associated diseases and the success of transplantation.
Currently, the possible role of HHV-6 in the development of multiple sclerosis, chronic fatigue syndrome, lymphoproliferative diseases, and its effect on the course of HIV infection is being actively studied.
To diagnose HHV-6, detection of virus-specific IgG antibodies is widely used, which are divided into subclasses:
1) IgG antibodies to early (non-structural) proteins of HHV-6
These antibodies appear in response to the activation of the virus in the cell it has infected. They are very specific, so there are no false positive results when they are detected. The presence of IgG to early early proteins of HHV-6 is an unambiguous sign of virus activity. They are produced both during primary acute infection and during relapse of chronic infection and reinfection with HHV-6.
2) Low-avidity IgG antibodies to HHV-6
10-14 days after the initial infection with HHV-6, a person without immunodeficiency develops IgG antibodies with low avidity (weak binding force of HHV-6 antigens), while the avidity of IgG antibodies constantly increases, and the proportion of low-avidity IgG antibodies decreases, so that they are completely disappear after 1-3 months. The detection of more than 50% low-avidity IgG to HHV-6 among IgG is an unambiguous sign of primary infection with this virus.
3) High-avidity IgG antibodies to HHV-6
They begin to be produced almost simultaneously with low-avidity IgG antibodies and circulate in the blood of the HHV-6 carrier throughout his life.
An analysis for IgG to HHV-6 with their classification into the subclasses described above is, of course, very informative, but is rarely used because it requires expensive immunodiagnostic kits. In this regard, the standard test for IgG antibodies to HHV-6 is an enzyme-linked immunosorbent assay (ELISA) of blood serum with the determination of the diagnostic titer of all virus-specific IgG in general and taking into account its changes.
Primary infection
Primary infection with HHV-6, as a rule, occurs in childhood (up to 3 years) and in most cases (70-80%) does not lead to an acute infectious process, but passes into a latent, asymptomatic course (virus carriage). However, the human immune system responds to the invading virus by producing antibodies. IgG appears in the 2nd week after infection in a small concentration, which continuously increases and reaches a maximum after a month. In the absence of active replication of the virus, the achieved level of specific IgG antibodies is maintained throughout life with minor fluctuations. It follows from this that if the analysis does not detect virus-specific IgG or they are found in a low titer, then a repeat test is necessary 2 weeks after the first.
If after the initial infection the virus begins to actively multiply, an acute primary HHV-6 infection develops, which in the vast majority of cases is manifested by large skin rashes and fever. In this case, virus-specific IgG antibodies also reach a peak after a month, but their titer is 2-4 times higher than during a latent course. After neutralization of active viruses, the titer of virus-specific IgG begins to gradually decrease and after 1-1.5 months approaches the level of antibodies during a latent course.
Secondary infection
The chronic (latent) course of HHV-6 may be accompanied by exacerbations of the primary latent process or relapses of the primary infection. In addition, rarely, when, as a result of antiviral therapy and effective immune defense, the primary infection with HHV-6 has resulted in the elimination of the virus, re-infection with HHV-6 or reinfection is possible.
All cases of secondary infection are characterized by the presence in the body of pre-existing IgG antibodies to HHV-6. Nevertheless, exacerbation, relapse and reinfection stimulate additional production of virus-specific IgG, and their titer begins to increase on the 1st-3rd day of the infectious process. However, since a secondary infection develops, as a rule, due to a decrease in existing antiviral immunity, the titer of IgG antibodies may be significantly lower, and the time to reach the peak of their production is significantly longer than that observed with a normally functioning immune system. As with a primary acute infection, after neutralization of active CC-6 viruses, the IgG level begins to decrease and reaches the initial value 1-1.5 months after the onset of clinical remission.
Thus, if IgG antibodies to HHV-6 are detected in the blood, the test should be repeated 2 weeks after the previous one and 1-1.5 months after remission.
What do the results mean?
Reference values
Result: negative.
CP (positivity coefficient): 0 - 0.79.
Positive result
A single positive result clearly indicates the presence of HHV-6. However, given the widespread distribution of this virus in an inactive form among the population, to determine the nature of the chronic viral infection (active/inactive), a repeat IgG test is required 2 weeks after the previous one. An increase in antibody titer by at least 1.5-2 times compared to the previous one indicates the activity of HHV-6. To confirm remission of the viral infection, two more repeat tests are required: the first is performed when symptoms are in remission, the second is performed 1 month after the previous one. The decrease in the titer of virus-specific IgG in the second study by at least 1.5 times compared to the previous one allows us to speak with confidence about the absence of active HHV-6 and the onset of remission of the viral infection.
Negative result
- A single negative result may indicate the absence of HCH-6 or an early stage of infection (up to two weeks). It is necessary to re-test in at least 2 weeks.
- A repeated negative result clearly indicates the absence of ICH-6.
What can influence the result?
In addition to violations associated with the collection, storage, transportation of biomaterial and the conduct of the study, the state of the immune system affects the result. Due to the fact that the immune system of newborns and young children is unstable, and blood, tissue and organ donors are subject to immunosuppressive therapy, the immunity of such patients at the time of the study is weakened (compromised). In this case, the production of IgG antibodies may be reduced, leading to a false negative test result.
Important Notes
With a viral infection mediated by HHV-6, the main thing is to determine the nature of its course (active/inactive). For this purpose, if HHV-6 is suspected, it is necessary to monitor the dynamics of the level of IgG antibodies - for any result of the first test, a repeat test is required at least 2 weeks later. For patients with a suspected compromised immune system, serological testing should be complemented by detection of the viral genome using real-time PCR.
Also recommended
- Human Herpes Virus 6, DNA [real-time PCR]
Who orders the study?
Virologist, immunologist, serologist, obstetrician, gynecologist, infectious disease specialist, pediatrician, neurologist, hematologist, transplantologist.
Literature
- Salahuddin SZ, Albashi DV, Markham PD, et.al., (1986) Isolation of a new virus, HBLB, in patient with lymphoproliferative disorders. Science 234:596–601.
- Kruegar GRF, Koch B., Ramon A., et al. (1988) Antibody prevalence to HBLV (human herpesvirus-6, HHV-6) and suggestive pathogenecity in the general population and in patients with immune deficiency syndromes. J Virol Methods 21:125–131.
- Yamanishi K., Okuno T., Shiraki K., et al. (1988) Identification of human herpesvirus-6 as a casual agent for exanthem subitum. Lancet 1:1065–1067.
- Asano Y., Yoshikawa T., Kajita Y et al. (1992) Fatal encephalitis/encephalopathy in primary human herpesvirus-6 infection. Arch. Dis. Child. 67:1484-1485.
- Asano Y., Yoshikawa T., Suga S., et al. (1990) Fatal fulminant hepatitis in an infant with human herpesvirus-6 infection. Lancet 335: 862-863.
- Preziozo PJ, Cangiarella J, Lee M, et al. (1992) Fatal disseminated infection with humanherpesvirus-6. J Pediatrics 120:921–923.
- Steeper TA, Horwiitz CA, Ablashi DV et al. (1990) The spectrum of clinical and laboratory findings for Human Herpesvirus-6 (HHV-6) in patients with mononucleosis-like illness not resulting from Epsein-Barr virus or cytomegalovirus. Am.J.Clin.Pathol. 93:776-783.
- Dubedat S. and Kappadoga N. (1989) Hepatitis due to human herpesvirus-6. Lancet 2:1463–1464.
- Eizuru Y., Minematsu T., Minamishima Y., et al. (1989) Human herpesvirus-6 in lymph nodes. Lancet 1:40.
- Drobyski WR, Dunne WM, Burd EM, et al. (1993) Human herpesvirus-6 (HHV-6) infection in allogenic bone marrow transplantant recipients: Evidence of a marrow-suppressive role for HHV-6 in vivo. J.Inf.Dis. 167:735-739
- Gautheret-Dejean, A. J. Virol Methods. 2002 Feb;100(1-2):27-35. Development of a real-time polymerase chain reaction assay for the diagnosis of human herpesvirus-6 infection and application to bone marrow transplant patients.
- Buchwald D., Cheney PR, Peterson DL, et al (1992) A chronic illness characterized by fatigue, neurologic and immunologic disorders, and active human herpesvirus-6 infection. Ann.Intern.Med. 116:103-113.
- Dr. KN Ward, JJ Gray, ME Joslin, MJ Sheldon Avidity of IgG antibodies to human herpesvirus-6 distinguishes primary from recurrent infection in organ transplant recipients and excludes cross-reactivity with other herpesviruses Journal of Medical Virology Volume 39, Issue 1, pages 44– 49, January 1993.
- Krueger GR, Ablashi DV, Josephs SF, Salahuddin SZ, Lembke U, Ramon A, Bertram G. Clinical indications and diagnostic techniques of human herpesvirus-6 (HHV-6) infection.n Vivo. 1991 May-Jun;5(3):287-95.
- T. Sloots, John Kapeleris, I. Mackay, M. Batham, and P. Devine. Evaluation of a Commercial Enzyme-Linked Immunosorbent Assay for Detection of Serum Immunoglobulin G Response to Human Herpesvirus 6 JOURNAL OF CLINICAL MICROBIOLOGY, Mar. 1996, p. 675–679 Vol. 34, No. 3.
Material for research
Any biological fluid and body tissue obtained from the site of the supposed localization of the infectious process, that is, the place of the highest concentration of the virus or microorganism.
- Whole blood
- Pleural, cerebrospinal, synovial fluid punctures
- Sputum
- Scraping or smear from the urogenital tract, etc.
PCR refers to direct diagnostic methods that reveal the direct cause of the pathological process.

The material being tested reveals a unique DNA fragment characteristic of this pathogen. PCR helps to detect infectious agents even in cases where other types of tests (bacteriological, immunological, microscopic) are not possible.
The use of PCR is very effective against not only acute, but also sluggish, latent infections.