Introduction
Ureaplasmas received their name due to the ability to break down urea in urine under the action of the produced enzyme urease (urina - urine, translated from Latin).
In the genus Ureaplasma spp there are two species – Ureaplasma urealyticum and Ureaplasma parvum. Differences between ureaplasmas and obvious pathogens
(sexually transmitted infections)
- found in 50-70% of healthy people
- may be detected in children
- often detected in only one of the two partners
- as a rule, they are very difficult to treat and are often diagnosed again after 2-3 courses of antibiotic therapy
Story
Microorganisms of this genus were discovered in the mid-20th century while studying bacteria living in the genitourinary tract. At the same time, it was suggested that they might be involved in the development of inflammation in this area in some cases. Then nothing was heard about them for several decades. This is due to the fact that, being small in size and unable to grow on nutrient media, there was no possibility of diagnosing them in practical medicine. And only with the advent of the PCR (polymerase chain reaction) diagnostic method in the 80s, they began to be identified and treated abroad. This was convenient for doctors, since sometimes not understanding the true cause of inflammation in the genitourinary organs, ureaplasma was almost always detected and was the basis for prescribing antibacterial therapy.
However, over time, their frequent detection and repeated presence in control tests after treatment made scientists think about the true pathogenicity of these microorganisms. Articles of that time talking about possible involvement in infertility, miscarriage, fetal pathology, inflammation in the genital organs did not have scientific validity and statistical evidence. Since approximately 2000, most progressive countries in Europe and North America have not carried out examination and treatment of ureaplasmas, considering them to be normal endogenous (internal) flora, which is often detected even in children.
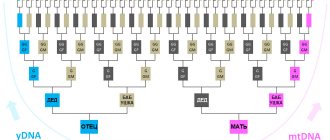
Pros and cons of PCR diagnostics and bacteriological culture
The PCR (polymer chain reaction) method allows you to get a quick and accurate result when identifying a disease, but it is not recommended to use it to check the results of treatment, since even after therapy the bacteria remain in the body for another 2-3 weeks, and the analysis can give a positive result . Therefore, PCR is prescribed on the 14-20th day after taking the last tablet.
Bacteriological culture is one of the most informative tests for ureaplasma. During it, a smear is taken from the mucous membrane of the urethra, vaginal vaults, as well as from the cervical canal, the contents of which are placed in a special environment favorable for the growth of the pathogen. If the culture result indicates the number of these organisms is more than 104 CFU/ml, treatment for ureaplasmosis is prescribed.
The additional value of bacteriological culture is that it helps to identify the sensitivity of ureaplasmosis pathogens to antibiotics, as well as to evaluate the results of therapy already carried out. However, in order to obtain the most reliable information about the presence of the disease and the extent of its spread, doctors often prescribe several laboratory tests at once.
When ureaplasmosis is detected, it is advisable to conduct tests for other sexually transmitted infections: bacteria often coexist with chlamydia, trichomonas and other microorganisms.
At the MLC, you can not only undergo culture and other types of tests for ureaplasma, but also, if necessary, receive effective doctor’s prescriptions.
Official information
Below, I quote verbatim excerpts from the fundamental document that should guide doctors (dermatovenereologists, gynecologists, urologists) in matters of diagnosis and treatment of ureaplasma. (Author's note - this document is in the public domain and can be easily found on the Internet)
“Federal clinical guidelines for the management of patients with urogenital diseases caused by Ureaplasma spp, Mycoplasma hominis”, Moscow, 2015.
Recommendations were developed by the Russian Society of Dermatovenereologists and Cosmetologists and the Russian Society of Obstetricians and Gynecologists.
Code according to the International Classification of Diseases (ICD-10) – A63.8 – Other specified diseases transmitted predominantly
sexually. (Author's note - the operative word here is "primarily")
Cause and epidemiology
Mycoplasma hominis and Ureaplasma spp. – opportunistic microorganisms that, when realizing their pathogenic properties, can cause urethritis (U.urealyticum), cervicitis (inflammation of the cervix), cystitis, pelvic inflammatory disease (PID), as well as complications during pregnancy and post-abortion complications.
For me personally, the big question is how to reliably determine that a pregnancy complication is caused by the presence of ureaplasmas, if statistically they occur in 50-70% of people.
The frequency of detection of Ureaplasma varies widely in different population groups, ranging from 10% to 50% (according to some authors - up to 80%, while usually true pathology does not exceed 10%). (Author's note - usually true pathology does not exceed 10%)
WHO experts (World Health Organization, 2006) identified U.urealyticum as a potential causative agent of urethritis in men, and possibly PID in women. At the same time, experts from the US Centers for Disease Control and Prevention (CDC, 2010) do not consider the presence of ureaplasma to be proven as a cause of the development of inflammatory processes in the genitourinary system.
Treatment
Regardless of the clinical case, treatment of ureaplasmosis is carried out in accordance with the following rules:
- Not only the patient, but also his sexual partner should be treated. Having a regular sexual partner, it is necessary to come for examination and receive therapy together. This helps prevent re-infection and spread of the disease;
- If concomitant infections are detected, therapy is selected according to an individual scheme. The attending physician at the MedArt clinic selects the most appropriate medications and their dosage;
- During the period of receiving therapy, you will need to abstain from any sexual relations (even using condoms);
- To consolidate the therapeutic result and prevent relapse, a follow-up examination is carried out.
Treatment of ureaplasmosis in men and women is carried out according to the same scheme. It involves an integrated approach that simultaneously affects different systems of the body. For this purpose they prescribe:
- A course of antibacterial drugs. Antibiotics can be taken either in tablet form or as vaginal suppositories. It is possible to administer medications using douching. To prevent disruption of the intestinal microflora, patients are prescribed probiotics to prevent disruption of the digestive tract;
- Immunostimulants. They strengthen immune defense, as a result of which the body intensively fights infection and its consequences;
- Temporary refusal of sex. This is a necessary measure that makes it possible to prevent the disease from becoming chronic or carrier. It also helps prevent reinfection and infecting other people;
- Diet. Since ureaplasmosis must be treated comprehensively, it is worth paying special attention to the diet. You will need to limit your consumption of fried, smoked and salty foods. It is also recommended to avoid alcoholic beverages (especially while taking antibiotics).
As mentioned above, to eliminate ureaplasma, it is necessary to examine and treat not only the patient, but also his sexual partners. After completing the therapeutic course, you will need to monitor the presence of the parasite for the first 3-4 months, so it is important to regularly visit the doctor on the appointed days.
In the absence of timely medical intervention, this disease can become chronic. In this case, the treatment regimen for ureaplasmosis changes. The patient is prescribed a long course of antibacterial drugs. In the absence of the desired therapeutic effect, it is possible to change the antibiotic group. Immunomodulators are also used to improve immunity. To improve the prognosis and well-being, patients are advised to undergo physiotherapy.
Symptoms of ureaplasma
Among women:
- mucopurulent discharge from the genital tract
- itching, burning, pain when urinating
- pain during sexual intercourse
- discomfort and pain in the lower abdomen
- swelling and redness of the vaginal and cervical mucosa
Classic signs of inflammation of the external genitalia and pelvic organs are described!
For men:
- mucopurulent discharge from the external opening of the urethra
- itching and burning in the urethra when urinating
- pain during intercourse
- frequent urination
- pain in the perineum
- swelling and redness of the external opening of the urethra
Classic symptoms of urethritis and prostatitis are described. In 18 years of my practice, I have never seen a patient have these symptoms and during the examination only ureaplasma was detected!!!
Diagnosis of ureaplasma
Indications for examination for Ureaplasma spp.
is the presence of clinical and laboratory signs of an inflammatory process in the area of the urogenital tract and reproductive system, vaginal dysbiosis in the absence of pathogenic pathogens.
I translate into Russian - if there are no complaints and no signs of inflammation in the genitourinary organs, there is no need to be examined for ureaplasma.
If there are complaints and signs of inflammation, then men are first examined for STIs (sexually transmitted infections - chlamydia, mycoplasma genitalium, gonorrhea, trichomonas), women - STIs, thrush, bacterial vaginosis, aerobic vaginitis. And if only after this examination it is not possible to identify the cause of the inflammation, then by the method of exclusion we can assume that this inflammation is caused precisely by ureaplasmas and suggest being examined for them.
In the absence of clinical and laboratory signs of the inflammatory process, the following are subject to examination:
- sperm donors
- patients diagnosed with infertility
- patients with a history of miscarriage and perinatal losses
Considering the difficulty of identifying the true causes of infertility and miscarriage, the wariness of doctors around the world in prescribing antibiotics in cases where there are no absolute indications for this, in this case I consider the prescribing of antibacterial drugs to be a greater evil than a benefit.
Where to treat
It is necessary to understand that it is almost impossible to cope with ureaplasmosis on your own. Moreover, self-medication can cause significant harm to health and only aggravates the course of the disease. Purchasing and taking antibacterial drugs without a medical prescription can lead to disruption of the intestinal microflora, as well as obtaining the status of a carrier of ureaplasma. In this case, the patient will not suffer from symptoms of the pathology (up to a certain point), but will be able to infect other people.
Therefore, it is strongly recommended to make an appointment with a doctor at the MedArt clinic if you identify the first signs of ureaplasmosis. An early visit to the doctor will help stop the progression of the pathological process and prevent the development of severe complications (including male and female infertility). The MedArt medical center has a diagnostic laboratory equipped with modern technical equipment. Thanks to this, specialists can make the correct diagnosis in the shortest possible time. Treatment is prescribed on an individual basis, depending on the characteristics of the body and associated factors.