Intubation
(lat. in in, inside + tuba tube) - the introduction of special tubes into the lumen of the larynx, trachea and bronchi in order to restore and improve the patency of the airways or to provide inhalation anesthesia.
For the first time in 1858, Bouchut (JAE Bouchut) came up with the idea of intubation at a meeting of the Paris Academy. The essence of the method he proposed was to introduce a hollow silver cylindrical tube into the larynx using a laryngeal curved catheter. However, this idea was not approved. O'Dwyer (J. R. O'Dwyer) in 1885 published the original work on Intubation, proposing a rubber tube for this, after which Intubation became widespread, first in America and then in Europe. In Russia, the first intubation was carried out by K. A. Rauchfus in 1890. In Moscow, intubation was introduced by A. A. Polievktov (1899) in the clinic of N. F. Filatov. INTUBATION under vision control was proposed by A. F. Pushkin; later it was used by A.I. Kolomiychenko, V.A. Ratner, and it was introduced into wide practice. Bronchial airway is used for one-pulmonary anesthesia, first developed and put into practice by Gall and Waters (I. Gall, R. Waters, 1932). Separate I. of the main bronchi was used to study lung function by Jacobeus, Frenckner and Bjorkman (H. Yacobaeus, R. Frenckner, S. Biorkman, 1932). Depending on the method of insertion of the endotracheal tube, I. are distinguished: orotracheal, nasotracheal, I. through tracheostomy; depending on the time - single, extended (i.e. over several days); depending on the goals - endobronchial, one-pulmonary, separate I. of the main bronchi.
Carefully performed and correctly carried out intubation allows you to ensure adequate external respiration and avoid tracheostomy (see). I. has certain advantages over tracheostomy - the absence of complications inherent in the latter (aspiration pneumonia, bleeding, emphysema).
Promotion! Free consultation with a gastroenterologist
For patients who undergo endoscopic examination at our Center, we have launched a special offer.
Complete any endoscopic examination in our Center and receive a consultation with a gastroenterologist as a gift!
Since the patient cannot independently interpret the results of the examination, we offer a consultation with gastroenterologists at our clinic for FREE!
Not only will the results of the service provided be explained to you, but treatment will also be prescribed, if necessary.
The promotion is held at the medical branch at 65 Yu. Gagarin Ave. (Zvezdnaya, Moskovskaya)
Details and registration by phone 325-03-05
We will perform fibrogastroscopy of the stomach (FGDS) in St. Petersburg - in 2-3 minutes, without pain (if desired, under anesthesia), with minimal discomfort using modern equipment.
Types of gastroscopy
FGDS as a method of diagnosis and treatment of the digestive tract is divided into the following main types:
- diagnostic and therapeutic (according to intended purpose);
- planned and emergency (according to the degree of urgency).
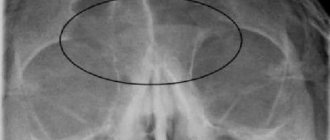
Routine fibrogastroduodenoscopy is prescribed as a method for diagnosing problems with the stomach and duodenum (inflammation, ulcers, neoplasms, etc.), as well as for analyzing the condition of the mucous membrane of the digestive tract in case of disease of the gallbladder and pancreas.
Endoscopy is also indicated as a method for diagnosing atrophic gastritis, gastric polyps, Menetrier's disease and precancerous diseases. Emergency endoscopy of the stomach is performed to determine the site of bleeding in the digestive tract, remove foreign bodies, and differentially diagnose complex surgical conditions in the case of diseases of the digestive system.
The therapeutic purpose of FGDS is, first of all, to stop bleeding in the gastrointestinal tract, remove polyps, cryo-freeze ulcers, and remove foreign bodies.
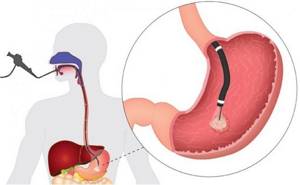
What is fibrogastroscopy (FGDS)?
This study is necessary to make a diagnosis for diseases of the digestive system. FGDS can be performed under intravenous anesthesia using analgesics. This is especially true when, together with FGDS, a study of the large intestine - colonoscopy - is carried out sequentially.
Gastroscopy is a study of the upper gastrointestinal tract, which is carried out using a special device (gastroscope). Thanks to this examination, the doctor has the opportunity to conduct a detailed internal examination of the intestine, assess the condition of all its parts and mucous membrane, and also timely diagnose most diseases in the shortest possible time. If necessary, during the examination a biopsy is taken - a piece of the mucous membrane of the examined part of the digestive tract or its pathological formations is absolutely painlessly pinched off and sent to a special laboratory for study. This helps reduce the risks of complications and the progression of diseases into acute and chronic forms. In addition, the optimal treatment is selected and the time spent on treatment is reduced.
Indications and contraindications
The previously existing most common indication for the so-called. classical Intubation - diphtheria croup - has become a rarity in modern wedge practice. I. of the trachea and bronchi are most widely used for anesthesia and resuscitation.
Tracheal intubation is indicated for major surgical interventions that require the regulation of vital body functions, during operations and manipulations accompanied by impaired external respiration functions, and during the provision of resuscitation care. There are no absolute contraindications to I. during anesthesia and resuscitation; diseases of the pharynx and larynx (acute inflammatory processes, tuberculosis, cancer, etc.) are relative.
In otorhinolaryngological practice, I. is indicated for stenosis of the larynx, trachea and bronchi, acute laryngotracheitis of viral etiology, and the initial period of bilateral paralysis of the lower laryngeal nerves, when there are still no inflammatory changes in the mucous membrane of the larynx. I. is also indicated for the edematous-infiltrative form of acute laryngotracheitis. According to I.B. Soldatov et al., extended I. is necessary during the period of transition from the stage of incomplete compensation of laryngeal stenosis to the stage of decompensation. Carrying out I. in the terminal stage of laryngeal stenosis is ineffective, because by this time irreversible changes have developed in the patient’s body. I. is contraindicated for bedsores, ulcers, specific granulomas, injuries and neoplasms of the larynx. Repeated I. must be abandoned when the endotracheal tube is repeatedly coughed up or when it quickly becomes blocked with films, crusts, or thick sputum. When the endotracheal tube is in the trachea for a long time (from 4 to 6 days), in some cases a tracheostomy is indicated.
What diseases does FGDS detect?
The FGDS method makes it possible to identify the following pathologies:
- diverticula and polyps,
- diagnose Hirschsprung's and Crohn's diseases,
- oncological diseases and colitis,
- establish the causes of regular bowel movements, abdominal pain, etc.
- benign tumors of the mucous membrane of the gastrointestinal tract and submucosal layer;
- inflammation of the esophagus: esophagitis, gastritis, duodenitis;
- hiatal hernias.
Most often, gastritis is detected during gastroscopy, and a visual examination determines the form of the disease, the extent of the lesion, and its severity.
The need for gastroscopy is determined by the doctor in cases where the patient is concerned about:
- stomach ache
- heartburn
- belching
- vomit
- swallowing disorder
- feeling of a lump behind the sternum
- unexplained weight loss
- loss of appetite.
When it is necessary?
It is necessary to do an FGDS in the case when a gastroenterologist has doubts about the correct functioning of the digestive organs. As we have already said, FGDS allows the doctor to most accurately assess the condition of the mucous membrane of all organs of the gastrointestinal tract.
Despite the effectiveness of this procedure, the scope of its use is strictly regulated. The fact is that in some cases, endoscopy is associated with difficulties due to the physical condition of the patient, and sometimes it is simply impossible for the same reasons.
If the drug effect on the organs of the digestive system gives a positive result, then the need for an FGDS automatically disappears. However, prolonged gastritis, ulcerative erosions, gastroduodenitis and other diseases make FGDS of the stomach and adjacent organs a mandatory procedure.
A therapist or gastroenterologist pays special attention to the following series of symptoms: sudden weight loss, anemia, difficulty swallowing, deterioration and lack of appetite, dark-colored stools. These and a number of other symptoms may indicate the development of a tumor or bleeding in a particular area of the gastrointestinal tract.
To date, there is no adequate alternative to fibrogastroduodenoscopy. Even examination of the digestive tract organs using ultrasound does not provide a detailed picture of the condition of the intestinal walls, excluding cases of large ulcerative lesions. And if fibrogastroduodenoscopy is prescribed by a gastroenterologist, then it cannot be replaced by another form of diagnosis.
FGDS and colonoscopy procedures are often combined in one appointment.
Technologies
- Classical Esophagogastroduodenoscopy and Fibercolonoscopy
- Innovative high-precision diagnostics - Videoesophagogastroduodenoscopy and Videocolonoscopy
The FGDS procedure is carried out as follows:
- The root of the tongue and part of the larynx are treated with lidocaine. Such preparation for FGDS will reduce discomfort and eliminate spontaneous traumatic contractions (swallowing). Lidocaine is usually applied as a spray without any injections.
- After a few minutes, the doctor begins the examination. The patient lies on his side facing the doctor, with a pillow placed under his head.
- To prevent spontaneous clenching of the jaw and damage to the endoscope during FGDS, the patient is given a mouthpiece. It is simply impossible to clench your teeth with him.
- The doctor carefully inserts the endoscopic tube through the mouth, and asks the patient to swallow at this moment to simplify and speed up the procedure. These are the most unpleasant moments, but everything goes by very quickly.
- The endoscopist moves the tube along the esophagus, turning the tip of the endoscope with the camera in different directions to carefully examine everything. This is somewhat unpleasant, but not painful. You can reduce discomfort by breathing deeply through your nose and not trying to swallow saliva.
- If necessary, a biopsy is performed during the examination. This is a painless manipulation.
- At the end of the study, the doctor carefully and quickly removes the endoscope. After this, the patient gets up from the couch and waits to receive the results.
- After endoscopy, the patient is not limited in his activities and can even go to work.
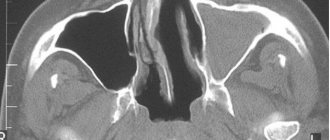
How is tracheobronchoscopy performed?
- On the eve of the procedure, the patient undergoes an examination by a doctor. If necessary, it is possible to prescribe a sedative at night, this will reduce the level of anxiety and allow you to get a good night's sleep.
- Sedative medications can be taken immediately before the start of endoscopy, but the decision remains with the doctor.
- Dentures must be removed; the flexible tube of the endoscope can displace them towards the respiratory tract.
- The neck should be free, so choose clothes that are loose at the top.
- During the preliminary examination, it is necessary to inform if there is a history of allergic reactions to medications or products.
- To ensure that the endoscope passes painlessly and a cough reflex does not occur, local anesthesia is applied to the mucous membrane of the nasal cavity and oropharynx using a sprayer.
- The position during the procedure is determined by the doctor. There are two options: lying on your back or sitting on a chair.
- At the end of the endoscope there is a camera that will allow the doctor to insert the instrument under visual control while simultaneously examining the lungs on both sides.
- Most often, the device is inserted through the nose, but sometimes through the oral cavity.
- Special forceps are used for biopsy. The procedure for taking a sample from the mucous membrane is painless and extends the time by only 1-2 minutes.
How to properly prepare for the procedure?
If you follow all the recommendations of the doctor who will conduct the study, you can avoid discomfort during the FGDS procedure:
- Dinner the night before the test should be light. It is recommended to avoid dishes that contain meat, mushrooms, animal fats, nuts and chocolate. Instead, you should give preference to fish, chicken breast with a side dish of vegetables or buckwheat.
- The last meal should be no less than 8 hours before the procedure, since any meal immediately before FGDS will make it difficult to examine the area being examined and may provoke an attack of vomiting, so the study will be impossible and will have to be scheduled for another day.
- You can drink no later than four hours before the start of the FGDS.
- It is recommended not to smoke on the day before the procedure, because nicotine sharply increases the secretion of gastric juice and strengthens gag reflexes.
- On the day of the examination, you must refrain from chewing gum.
- Immediately before the examination, removable dentures, etc. must be removed. (braces, piercing), glasses, tie.
After the study, it is not recommended to drink or eat food for 30 minutes. If you have had a biopsy, the food you eat on the day of the test should not be hot.
What can you do after bronchoscopy?
It will take about 20-30 minutes for the numbness in the throat to go away, then the patient is allowed to eat. Usually a person understands this himself when the feeling of a foreign body and cold disappears. If the endoscopy was accompanied by the collection of biological material for additional laboratory testing, then the time of meal intake is determined by the doctor.
By following the basic rules and recommendations of the doctor, the patient will not feel discomfort and will soon receive the results of the diagnostic procedure performed.
How to prepare for gastroscopy?
Morning examination:
- Preparation for FGDS requires that the last meal be taken approximately 8-12 hours before the diagnosis. Therefore, it is easier to examine the stomach in the morning
- Last meal on the eve of the study in the evening before 22:00
- In the morning - do not eat or drink
- If you have removable dentures, they will need to be removed immediately before the examination (to avoid damage to them and to prevent them from entering the esophagus or trachea)
Examination in the evening:
- Do not eat food for 8 hours before gastroscopy
- It is allowed to take a small amount (2-3 sips) of plain water, always without gas, 2-3 hours before the test
- Smoking is strictly prohibited 2-3 hours in advance - one of the requirements for preparing for gastroscopy of the stomach
Intubation instruments
The previously used solid tubes of O'Dwyer, Sevester, Bayeux, etc., as well as special sets (for example, Collen, Fruen, etc.), introducers, extubators have practically lost their importance and honey. are not produced by industry. Modern intubation instruments include endotracheal tubes, conductors, mandrels for them, intubation forceps for inserting and removing tubes, connectors for connecting tubes to an anesthesia or breathing apparatus, laryngoscopes with straight and curved blades, dental spacers to prevent compression of the lumen of the tubes.
Rice. 1. Schematic representation of endotracheal tubes for intubation: 1 - without inflatable cuffs; 2 — with inflatable cuffs; 3 - curved at an angle; 4 - reinforced tubes; 5-8 - children's (5 - Cole type; 6 - with a Laennec type limiter; 7 - curved at an angle; 8 - curved). Rice. 2. Schematic representation of endobronchial tubes for one-pulmonary anesthesia: 1 - Goll and Waters tube; 2-3—Rovenstein tube, which makes it possible to turn off the air movement at different levels; 4 - Gordon-Green tube; 5 - McIntosh and Literdel tube; 6 - Brompton tube. Rice. 3. Schematic representation of double-lumen tubes for separate intubation of the bronchi: 1 - VNIIR tube (Gebauer type), 2 - Carlens tube, 3 - Kubryakov tube, 4 - Bryce-Smith tube, 5 - White tube, 6-8 - Kiprensky tubes (6 and 7 - universal, 8 - for the right bronchus).
Hartmann forceps or forceps from the Friedel tracheobronchoscopic set can be used as intubation forceps (see Bronchoesophagoscope). The most common are endotracheal tubes made of thick rubber or plastic; less commonly used are endotracheal tubes made of metal or rubberized silk fabric. For various methods of I., tubes of various designs are used (Fig. 1). When carrying out one-lung anesthesia, special endotracheal tubes are used (Fig. 2), which make it possible to turn off one lung from the act of external respiration, and for separate I. bronchi, double-lumen tubes are used (Fig. 3), which make it possible to periodically block the right or left main bronchus. For endotracheal anesthesia and artificial ventilation (during resuscitation), plastic or rubber endotracheal tubes are used. The latter are available with or without inflatable cuffs; Children's tubes are produced without an inflatable cuff. When the cuff is inflated, a seal is created between the airway and the wall of the tube. In the absence of a cuff, sealing is created using tamponade of the pharynx and oral cavity with gauze swabs. The shape, length and diameter of the endotracheal tubes are determined by the intended I. technique and the individual topographical and anatomical features of the structure of the patient's respiratory tract. For endotracheal intubation, the end of the endotracheal tube should be located approximately 2 cm above the tracheal bifurcation. The length of the endotracheal tube for adults ranges from 19 to 26 cm, for children - from 10 to 21 cm, the outer diameter for adults - from 8.0 to 12.3 mm, for children - from 3.6 to 12.3 mm. The following numbers of endotracheal tubes are produced in the USSR: 000, 00, 0, 1, 2, 3, 4, 5, 6, 7, 8, 9.
Sterilization of rubber endotracheal tubes is carried out as follows: after extubation (removal) of the endotracheal tube from the trachea, it is thoroughly washed in running warm water and soap. The lumen of the tube is treated with a gauze swab (you cannot use a cotton swab or a “hedgehog” swab, since threads of cotton wool or bristles can be a source of infection if they enter the patient’s respiratory tract). After rinsing in warm water, remove the remaining grease (glycerin ointment) with ether. The tube is sterilized by autoclaving or boiling for 3 minutes. To maintain the strength and elasticity of thermoplastic tubes, they are kept in antiseptic solutions (chloramphenicol 1:1000, etc.) - Disposable tubes are often used.
Advantages
- New, modern equipment from Pentax, Japan (endoscope tube diameter is only 9 mm).
- The examination is performed by an experienced endoscopist.
- Possibility of simultaneous gastro- and colonoscopy under general anesthesia.
- Possibility to carry out the procedure on a day convenient for the patient.
- Possibility of accommodation before and after the examination in comfortable day hospital wards.
- Maximum comfort for the patient: the examination takes place without pain and complications due to the use of a flexible, ergonomic gastroscope and colonoscope tube.
Endoscopy is the most modern, highly informative and minimally invasive method of examination and treatment.
This type of diagnosis makes it possible to identify pathological changes at the earliest stages.
Modern equipment and qualified specialists of the department allow endoscopic examinations to be carried out with minimal discomfort for the patient and with a high level of image clarity.
Caring for an intubated patient
An intubated patient should be under constant supervision by medical staff. This is necessary because the relatively narrow lumen of the endotracheal tube can become clogged with pathological secretions from the respiratory tract at any time. In such cases, the secretion is suctioned with a catheter inserted into the tube; if ineffective, repeat I. To prevent the patient from removing the endotracheal tube (spontaneous extubation), it is necessary to fix the elbow joints with a splint, and the tube with an adhesive plaster to the cheek.
The patient eats and drinks through the mouth; if normal nutrition is not possible, tube feeding is used.
Bibliography
Nosov S. D. Intubation in the treatment of patients with diphtheria croup, M., 1958, bibliogr.; Ostrovsky G. G., Shagal E. L. and Shulman V. Shch. Tracheostomy and prolonged nasotracheal intubation in the treatment of severe forms of acute stenotic laryngotracheobronchitis, Zhurn. ear, nose and throats, Bol., No. 6, p. 48, 1975, bibliogr.; Sokolov V. M. Modification of the method of intubation of newborns, Obstetrics and Gynecology, No. 10, p. 77, 1967; Allen T. H. a. Steven IM Prolonged nasotracheal intubation in infants and children, Brit. J. Anaesth., v. 44, p. 835, 1972; Crysdale WS Nasotracheal intubation in management of delayed decanulation, Ann. Otol. (St Louis), v. 83, p. 802, 1974, bibliogr.; Ferlic RM Tracheostomy or endotracheal intubation, ibid., p. 739.
Intubation of the trachea and bronchi during anesthesia and resuscitation
- Bunyatyan A. A., Ryabov G. A. and Manevich A. 3. Anesthesiology and resuscitation, M., 1977; Zhorov I. S. General anesthesia, M., 1964; Kassil V. L. and Ryabova N. M. Artificial ventilation in resuscitation, M., 1977, bibliogr.; Mashin U. Pain relief during intrathoracic operations, trans. from English, M., 1967; Resuscitation, theory and practice of revival, ed. M. Sykha, per. from Polish, Warsaw, 1976; Guide to Anesthesiology, ed. T. M. Darbinyan, M., 1973.
O. A. Dolina (anest.), D. I. Tarasov (ENT).
Purpose of the procedure
Gastroscopy or esophagogastroduodenoscopy is a modern diagnostic method, thanks to which it is possible to determine the presence of pathological processes such as:
- Ulcerative lesions of the esophagus and stomach.
- The presence of polyps, benign and malignant tumors.
- Diagnose inflammatory diseases of the gastrointestinal tract.
However, the procedure is also carried out to take gastric juice for further research in the laboratory. And also, if necessary, perform a biopsy, biomaterial is taken through a gastroscope and sent for analysis.
In addition, this method is used for medical procedures, for example, laser cauterization of affected areas. And also for the purpose of removing polyps.
A more modern analogue of the study is choledochoscopy, which is a method of studying the mucous membranes of the upper gastrointestinal tract using special rays of a certain spectrum.
The following symptoms may be the reason for gastroscopy:
- Painful sensations, heaviness in the stomach.
- Bloating.
- Nausea, vomiting, heartburn.
- Decreased appetite and rapid weight loss.
For preventive purposes, the procedure is performed annually for patients with ulcers and gastritis. After polyp removal every three months. As well as persons predisposed to cancer.
An urgent procedure is prescribed for complications of a peptic ulcer, if internal bleeding is suspected, or if a foreign body has entered the esophagus.

results
The gastroenterologist issues a written conclusion on the study. Based on the data obtained, a treatment method is selected and prescriptions are made.
If material was taken during gastroscopy for further research, the test results are attached to the conclusion.
Unfortunately, today the prices for gastroscopy of the stomach in St. Petersburg are high. This leads to the fact that patients cannot undergo examination in most St. Petersburg diagnostic centers.
Meanwhile, in St. Petersburg there is a place where the gastroscopy procedure can be performed at a low cost. This is the Poem of Health multidisciplinary clinic, which is located near the Ozerki and Prospekt Prosveshcheniya metro stations. Experienced gastroenterologists and polite and friendly medical staff work here. The clinic is equipped with modern diagnostic equipment. The gastroscopy procedure is carried out using effective and safe anesthetics.
A price list is posted on the clinic’s website, which shows prices for all types of studies. You can make an appointment online and also consult with a gastroenterologist.
Advantages of EGDS (FGDS) at the N. I. Pirogov Clinic:
- experienced doctors carry out early diagnosis of diseases, which allows treatment to begin at the pre-surgical stage or to manage with organ-preserving operations with a short recovery period;
- modern equipment of the latest generation from leading Western companies ensures accurate diagnosis;
- attentive and responsible medical staff;
- the highest standards of equipment sterility and patient safety, meeting the requirements of regulatory authorities;
- use of the latest generation of anesthesia that does not cause any discomfort after the intervention;
- biopsy and removal of mucosal polyps directly during the EGDS procedure;
- carrying out analysis for Helicobacter pylori and its quick deciphering;
- the highest standards of equipment sterility and patient safety, meeting the requirements of regulatory authorities.
Sign up for a consultation and make sure that your health is not in danger!
Make an appointment