Plethysmography is a human research technique that allows you to accurately record changes in the volume of a separate organ or part of the body, in most cases used to determine the tone of the smallest blood vessels and the current blood flow in them. Plethysmography can be used to study the functioning of most internal organs, but recently it is more often prescribed when it is necessary to study the function of external respiration (RF).
Airborne plethysmography
For recording, special devices are used - plethysmographs. Today, several types of such recorders are common. Mechanical ones directly record the amount of change in the electrical characteristics of tissues. Electro-, rheo- or photoplethysmographs “observe” the changes that occur during the blood supply to tissues/organs, or changes in their light transmittance.
When is the plethysmography test completed?
Plethysmography may be ordered for several reasons. Some of them include:
- In diagnosis, one should distinguish between obstructive and restrictive lung diseases. (In some cases, it may be difficult to determine whether pulmonary disease is obstructive or restrictive (whether there is overlap in some pulmonary function tests), and plethysmography can help make this difficult distinction.
- To evaluate your response to treatment. For example, to see whether your lung disease is getting worse, improving, or staying the same.
- To evaluate your lungs to see if you will have lung cancer surgery.
In the diagnosis of venous diseases, duplex ultrasound scanning (DS) is important for describing the anatomical features of lesions in the venous bed. Its data serves as the basis for a complete description of the patient using the CEAP classification[1]. However, using ultrasound DS it is impossible, or at least difficult, to assess the function of the venous system [2]. Plethysmographic methods, assessing fluctuations in the volume of the limb, in combination with DS, provide more complete information about the state of venous outflow [3-6]. The simplest option is photoplethysmography. It is based on assessing the intensity of light reflection from the subcutaneous venous plexus, which indirectly indicates the volume of blood in the skin and muscles of the limb. First described by A. Hertzman [7] in 1937, the technique was initially used to study arterial blood flow and was then adapted to study venous pathology [8]. The standardization of the method was carried out by V. Wienert and V. Blazek [9]. The main parameter assessed by photoplethysmography is the blood filling time and the percentage of emptying in 3 s. There is a strong correlation between the time of blood filling and the magnitude of venous pressure when directly measured [10], however, as some authors point out [11, 12], there is no direct connection between the time of blood filling and the severity of venous pathology.
The purpose of the study is to study clinical and instrumental parallels in various clinical classes of chronic venous diseases (CVD) using plethysmography.
133 patients were examined and divided into three groups. Group 1 included 90 patients with primary venous disease (Ep), mainly varicose veins, as well as telangiectasia and reticular varicose veins. Group 2 included 22 patients with postthrombotic disease with a disease duration of more than 3 months and with signs of chronic venous insufficiency - CVI (secondary venous disease - Es) [13]. Group 3 included 21 patients who had deep vein thrombosis in the period from 1 to 3 months before inclusion. There were no patients in the study groups who had previously operated on the venous system of the lower extremities.
In addition to physical examination, all patients underwent D.S. In case of bilateral lesions in patients with varicose veins, data on the limb with a large clinical class were taken into account. The characteristics of the groups are presented in Table. 1.
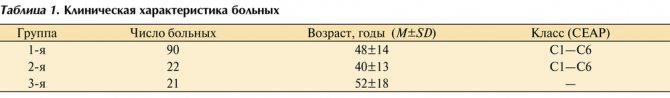
Table 1. Clinical characteristics of patients
In groups 1 and 2, class C1 (telangiectasia, reticular varicose veins) was detected in 7 (7.8%) and 2 (9.1%) patients, respectively.
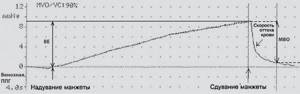
All patients underwent plethysmography (Doppler analyzer Smart Dop 30 EX with additional photo- and pneumatic sensors (Hadeco). Photoplethysmography determined the indicator of total venous reflux. On the plethysmographic curve (Fig. 1), the time of venous blood filling (VBF) and the half-venous time were calculated blood filling (½VVC). To study obstruction (patency of deep veins), occlusion plethysmography was used. During this study, venous outflow was studied in 3 s (in %), which was also recorded by the sensor and reflected in another curve (Fig. 2). Thus, we obtained digital data characterizing total venous reflux and the degree of venous obstruction.
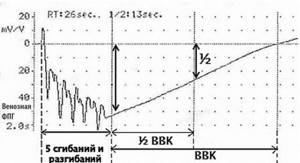
Rice. 1. Venous photoplethysmography curve. Study of the consistency of the valve apparatus of the veins of the lower extremities (reflux). The ordinate axis shows the parameters of the device when studying reflected light; the abscissa axis shows the time of venous filling. The patient's position is sitting with legs lowered without support. The infrared sensor is fixed to the skin in the projection of the posterior tibial neurovascular bundle. The patient performs 5 flexions and extensions of the foot. PPG - photoplethysmography.
Rice. 2. Curve obtained from venous occlusion pneumoplethysmography. Study of the patency of the deep veins of the lower extremities (obstruction). The ordinate is the pressure in the diagnostic cuff (in mmHg); The x-axis is the time © of pressure in the blocking cuff. The patient is positioned supine. A wide locking cuff is placed at the mid-thigh (60 mmHg). Measuring cuff - in the middle of the shin (15 mm Hg). After 90 s, the air from the blocking cuff is quickly removed. VE - venous capacity, 90 s, MVO - maximum venous outflow in 3 s, % venous emptying in 3 s = MVO/VE ×100%. PPG - venous pneumoplethysmography.
Statistical analysis of variables not normally distributed was performed using Kruskal–Wallis ANOVA, U
- Mann-Whitney test.
The correlation between parameters was assessed by Spearman's rank test. Data are presented as medians ( Me
) with interquartile range (
Q
1 -
Q
3), where
Q
1 is the first quartile, corresponding to the 25% percentile, and
Q
3 is the third quartile, corresponding to the 75% percentile.
The indicators of IVC and ½ IVC were 15 (12-18) and 6 (4-7) s in group 1, respectively, in group 2 - 13 (10-16) and 5 (4-6) s, and in group 3- y group - 14 (10-18) and 5 (5-6) s. No statistical significance was found in the pairwise study for VVC and ½VVC between groups ( p
>0.05). In all groups, a decrease in the values of VVC and ½VVC was noted (Fig. 3).
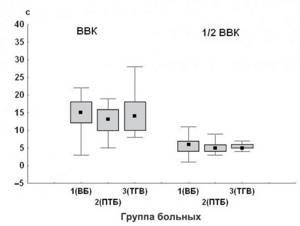
3. Indicators of venous reflux in patients of various groups. Here and in Fig. 4: VV - varicose veins; DVT - deep vein thrombosis; PTB is a post-thrombotic disease. With occlusion plethysmography in patients of group 1, the rate of venous outflow was 100% (100-100), which was significantly higher compared to patients of group 2 - 93% (83-98), p
<0.0001 and group 3 - 90% (82-95),
p
<0.0001. There were no statistically significant differences between groups 2 and 3 (Fig. 4). This fact is explainable, since primary venous disease is not accompanied by a violation of venous patency, and with a secondary disease, venous obstruction is always present to one degree or another.
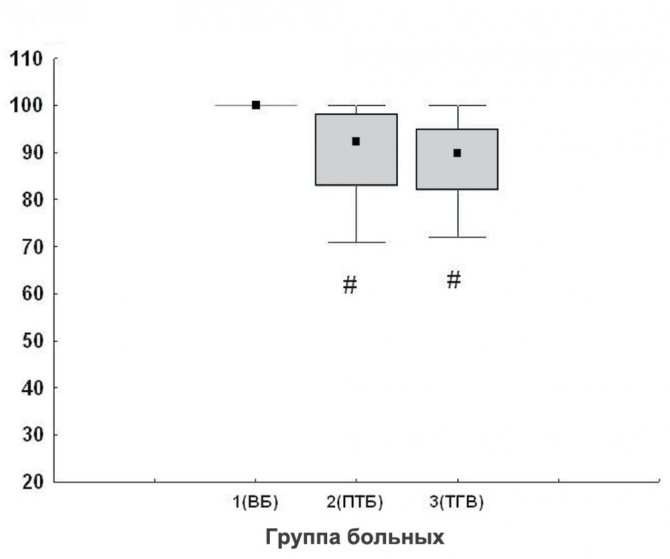
4. Indicators of venous obstruction (in%) in patients of various groups. A strong correlation was found between VVC, as well as a moderate correlation between ½VVC and the clinical class of the disease in group 1. In patients of group 2, the connection was of medium strength. In patients of group 3, a moderate correlation was revealed between ½VVC and indicators of impaired venous outflow (Table 2).
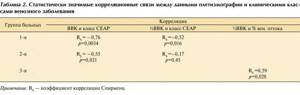
Table 2. Statistically significant correlations between plethysmography data and clinical classes of venous disease Note. RS—Spearman correlation coefficient.
A relationship was found between the magnitude of total venous reflux and the clinical class of the disease in patients of group 1: with class C1, the VVC was 28 (22-33) s, with class C2 - 20 (19-31) s, with class C3 - 15 (13- 18) s, for class C4 - 14 (10-16) s and for classes C5-C6 - 8 (7-10) s. Significant differences were observed between all subgroups, except class C1 and class C2, as well as class C4 and class C5. The ½VVK indicator for class C1 was 10 (8-12) s, for class C2 - 6 (6-12) s, for class C3 - 5 (5-7) s, for class C4 - 5 (4-6) s, for grades C5-C6 - 4 (4–4) pp. At the same time, there were no differences between classes C3 and C4 and C3 and C5–C6 (Fig. 5). The median IVC in patients with classes C1 and C2 was 28 and 20 s, respectively, and in patients with CVI (classes C3-C6) it was less than 20 s. Especially low rates of VVC (8 s) and ½VVC (4 s) were characteristic of patients with healed or open trophic ulcers.
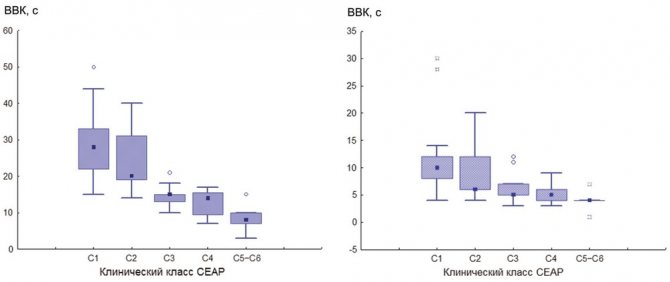
Rice. 5. Changes in venous reflux indicators in patients with different classes of primary venous disease.
The main pathophysiological mechanisms in the development of CVD are reflux, obstruction, or a combination of both [1]. Diagnosis of these conditions is based on the use of DS, which allows quantitative assessment of blood flow in certain anatomical areas, but cannot assess the total reflux in the superficial, deep and perforating veins [14]. The study of limb volume fluctuations (plethysmography) seems more justified to monitor the effectiveness of drug treatment [15], physical influences [16], sclerotherapy [17] or surgery [18]. In all these works, the effectiveness of treatment was determined based on quantitative characteristics, primarily on VVC, which correlates well with the severity of CVD. Based on this, we attempted to search for a connection between quantitative parameters reflecting the degree of impairment of venous outflow and the severity of clinical symptoms of the disease.
Determination of the degree of reflux in groups of patients with various types of pathology did not reveal significant differences. The median IVC in patients of these groups was within 13-15 s. In the 1st and 2nd groups of patients, the number of patients with clinical class C1 was 7 (7.8%) and 2 (9.1%), respectively.
Another indicator, the percentage of venous emptying, allows one to determine the presence of obstruction with a high degree of accuracy. In the group of patients with primary venous disease, emptying was complete (100%), while in patients with damage to the deep veins of different periods of time, it was 93 and 90%, respectively. Therefore, the air plethysmography method is important in identifying venous obstruction.
The most significant result was obtained when studying the relationship between reflux indicators and the clinical class of primary venous disease. The work of R. Bays [19] did not reveal a strong connection between VVC and the severity of venous disease. Relatively recent studies have demonstrated similar data [20, 21]. However, we found a strong connection between VVC and the clinical class of venous disease, which allowed us to draw clinical and instrumental parallels in patients with varicose veins. In these patients, a significant relationship was identified between the quantitative indicator reflecting the degree of reflux and the clinical class of the disease, and IVC values were established for individual classes. For C1 (no signs of CVI), the median IVC was 28 s, which corresponded to normal (more than 20 s) values for this indicator [5]. The appearance of signs of CVI (classes C3-C6) was accompanied by a decrease in IVC of less than 15 s in class C3 and up to 8 s in classes C5-C6. In patients with clinical class C2, the decrease in IVC was insignificant - 20 s.
Thus, in patients with primary and secondary venous diseases, a relationship was found between the clinical class and the indicators of total venous reflux. Using photoplethysmography, it is possible to accurately determine what clinical class of disease a patient has.
Conflict of interest: The authors report no conflict of interest.
Author contributions:
Study concept and design - N.H., D.V.
Collection and processing of material - N.Kh., D.V., V.K.
Statistical processing - D.V., V.K.
Text writing - N.Kh., V.K.
Editing - N.Kh., Ya.Sh.
What is the plethysmography procedure?
During plethysmography, you will be asked to sit in a small, sealed room that looks a bit like a telephone booth.
If you normally use oxygen, you will not need to receive oxygen during the test. Your technician will apply clamps to your nose and give you a mouthpiece to breathe in. Some people feel claustrophobic when the procedure begins, but you can open the door or remove the mouthpiece at any time if you need to (though this may lengthen the procedure.) The technician will then guide you through different breathing patterns, where you'll be breathing normally, then panting heavily. , then take a deep breath and exhale.
Most people tolerate the procedure very well, although some people may feel claustrophobic or light-headed during the procedure. Overall, the active portion of this test takes about 15 minutes.

What are the basic elements of a plethysmogram?
The structure of a plethysmogram consists of three basic types of oscillations that are reflected on it. These include:
- Waves that are of the first order and imply a volumetric impulse (a reflection occurs of how much the vessels are filled with blood during one run of blood through the arteries and veins).
- Waves that are of the second order are called respiratory (this indicator is recorded extremely unevenly and inconsistently and, as a rule, it is higher than the previous one).
- Waves that are of the third order mainly capture and record those vibrations that arise in the human body in addition to the above.
What does a plethysmography test measure?
Plethysmography gives your doctor measurements that can help her understand how well your lungs are functioning. Most pulmonary function tests do not measure residual volume, or the amount of air left in the lungs after you exhale as much air as possible. By determining this measurement, plethysmography helps your doctor calculate other numbers. Measurements that can be made using this test include:
- Functional Residual Volume - Functional residual volume is the amount of air remaining in your lungs after you exhale as much air as possible.
- Functional Residual Capacity (FRC) - Functional residual capacity (FRC) is a measure of how much air is left in your lungs after you exhale as much as possible (expiratory reserve volume). plus the amount of air remaining in the lungs after normal exhalation (residual volume).
- Total lung capacity (TLC) is a measure of the total amount of air in your chest after you've taken the deepest breath possible.
Preparatory stage
The preparatory stage is simple and does not require special conditions. It can be divided into several stages.
- The essence of the upcoming study is explained to the patient, explaining that plethysmography is a completely safe method of objective examination.
- Recommendations are given on the need to adhere to a daily routine; a healthy diet is desirable, excluding fatty, spicy and excessively carbohydrate foods. It is advisable to get a good night's sleep the night before the examination.
- The fact of avoiding stress on the eve and day of the study is reported. If this cannot be avoided, it is advisable to postpone the examination to the next day - excessive anxiety can distort the results.
- Within a few days, alcohol should be completely eliminated, it is advisable to limit smoking, and the doctor prescribing the study must be informed about the need to take any vasoactive drugs.

Impedance plethysmography
Some types of plethysmography, for example, impedance, do not require preparation at all. But it would be a good idea to follow the general recommendations and refrain from consuming certain foods.
Understanding Plethysmography Test Results
Depending on whether your results are elevated, whether your functional residual capacity is increased, normal, or less than expected, your doctor can better assess the lung condition you may be suffering from.
Increased functional residual capacity
Obstructive pulmonary diseases often cause an increase in FRC.
To put this into perspective, you can imagine how in conditions such as emphysema, the full volume is not exhaled after each inhalation. The elastic recoil is damaged, leaving excess air. The excess remaining air that cannot be exhaled is added to the normal volume remaining after exhalation. Conditions that may cause FRC to increase include:
- Emphysema;
- Cystic fibrosis;
Decrease in functional residual capacity
Reduced functional residual capacity means that there is a reduced amount of air space in the lungs.
This, in turn, may have several reasons. The lungs may be "less elastic" either externally or internally, for example due to weakness of the chest muscles associated with a stroke, or due to decreased elasticity of the lungs themselves (reduced elasticity) due to a chronic lung condition. You should also make sure that you have part of your lung removed for lung cancer. Diseases that can lead to decreased functional residual capacity include:
- Idiopathic pulmonary fibrosis;
- Other types of pulmonary fibrosis;
- Sarcoidosis;
- Removal of a lung or part of a lung;
- Obesity;
- Scoliosis;
These numbers may be abnormal if your airways are narrowed or blocked in some way, if there is too much air left in your lungs after you exhale (as with emphysema), or if your lungs are unable to expand fully.
Examples: Doctors usually recommend having a procedure called plethysmography before surgery for lung cancer.
Main types of plethysmographs

Plethysmograph for studying the function of external respiration
Each device consists of several parts:
- a receiving part equipped with a special calibrator;
- transmission system;
- recording device;
- tape drive with the necessary marks.
The very first device of this type was a mechanical apparatus designed to directly record changes in volume in the part of the body being studied. It has not found widespread use in clinical practice due to obvious difficulties in research. Later, electric and photovoltaic devices appeared. Electrical devices, in turn, are divided into dielectric and impedance. They are designed to assess the blood supply to the vessels of the whole body or brain. Photoelectric models are ideal for working with flat but large areas of skin.
Clinical designation
Along with the diagnostic method, a clinical one is also used. As a rule, it is used only when it is necessary to obtain the most complete information about a person’s condition. In this case, it is important to understand how impaired the patient’s blood circulation is and how weak the tone of the veins is. If the division into functional diseases is used, then subsequent results will also be required in order to carefully monitor the physical and mental state of the person, since these components play an equally significant role.
If one part of the body has been damaged, then there is a significant outflow of blood from that limb or area of the body. Then plethysmography will show low fluctuations and a very low frequency of waves.
In order to understand what nature a particular deviation has, it is worth conducting several additional tests. The reason can be both organic and functional. That is, certain tissues are damaged, but the body will function in the same rhythm, or damage can disrupt the normal functioning of some parts of the body or even organs.

The amplitude of vibrations varies in different parts of the body. For example:
- in the finger of the hand they (oscillations) reach 0.015 cm3;
- if it concerns the lower leg, then the amplitude reaches 0.15 cm3;
- if this is the eyeball, the orbit of the eye, then the indicator is slightly higher than in the finger - 0.016 cm3;
- if this is the area of the temples, then the amplitude of vibrations here is average and amounts to 0.01 cm3.