Today in Russia, tuberculoma is not a rare diagnosis. Let's try to figure out what it is and what you need to do if you have been diagnosed with tuberculoma.
Tuberculoma got its name because it looks like a tumor (most tumors have the suffix “-oma”) and is a round formation in the lung ranging in size from several millimeters to several centimeters. In terms of its structure, teburculoma is an area of necrotic (dead) lung tissue surrounded by a dense capsule. Tuberculoma forms at the site of active tuberculosis inflammation - tuberculosis infiltrate. The transformation of the infiltrate into tuberculoma in the lung indicates that active tuberculosis inflammation has subsided, that is, the body has overcome the infection (at least temporarily) and localized it in the lung, surrounded by a protective fibrous membrane.
Often tuberculoma does not cause any symptoms, and therefore is discovered by chance during fluorography or chest X-ray. In such cases, the presence of tuberculoma indicates that you once had a latent form of tuberculosis.
Is a patient with tuberculoma contagious? As a rule, no. However, the final answer to this question will be given by a TB doctor.
What happens when the TB pathogen (bacterium) enters the lungs?
There are 2 options:
- If your immune system functions well, the tuberculosis pathogen will be destroyed and the disease will not occur;
- Your immune system can control the infection, but it cannot kill the bacteria that causes TB. The body isolates the infection in the lungs and there will be no clinical manifestations. This condition is called infection. In Russia, about 70% of people over 30 years of age are infected. At any time, bacteria can begin to multiply (for example, when the immune system is weakened).
When the bacteria that causes tuberculosis begin to actively multiply in the lungs and destroy them, they speak of active tuberculosis.
Treatment
In countries with an increased number of cases of infection and spread of the disease, treatment is provided free of charge. This reduces the risk of infection, mortality and the likelihood of spreading infection during migration.
The main condition for treatment is complete cessation of smoking and drinking alcohol. Both the first and second greatly reduce the body’s immunity, making it unable to fight the disease. It is important to carefully follow all the necessary rules of personal hygiene, including for healthy people, to prevent the risk of disease.
Mycobacterium tuberculosis is able to quickly adapt and develop resistance to various drugs. Therefore, selecting a treatment regimen is a very long process.
Medicines are divided into several types:
Drugs that directly affect the causative agent of the disease and affect the resistance of the bacilli. They have bactericidal and bacteriostatic mechanisms of action.
- Isoniazid is the most effective drug, suppressing 90% of active and growing bacilli in a few days.
- Rifampicin is the best sterilizing agent.
- Pyrazinamide kills bacteria in the acidic environment of cells.
- "Ethambutol" is a chemotherapy drug that affects typical and atypical cells.
- The drug Streptomycin, which has an antimicrobial effect, is administered intravenously.
The second line of drugs to combat the disease includes tablets:
- "Protionamide" is a drug active in an acidic environment.
- "Cycloserine" is a bacteriostatic and bactericidal drug.
- “Ethionomide”, which has an effect on bacilli located outside and inside cells.
Intravenous drugs:
- Amikacin is a broad-spectrum antibiotic. Prescribed when bacilli are resistant to other drugs.
- "Kanamycin", active against acid-fast bacteria.
The dose of all medications must be calculated strictly by the attending physician, since it directly depends on the weight and age of the patient, as well as on the nature and stage of the disease.
Who is at risk for developing active tuberculosis?
The following groups of people are most susceptible to the disease:
- persons without a fixed place of residence;
- released from prison;
- living in shelters, boarding schools for the elderly;
- refugees, migrants;
- patients of drug treatment and psychiatric institutions.
There is a high probability of developing tuberculosis in people with chronic diseases of the respiratory system and cardiovascular system; receiving treatment with drugs that weaken the immune system; patients with diabetes mellitus, alcoholism, drug addiction; infected with HIV and patients with AIDS.
Hospital treatment

Usually treatment occurs at home, but sometimes the complex course of the disease requires observation in a hospital. Once the diagnosis is confirmed, treatment in hospital may take approximately 3-4 months. During this period, to monitor the success of treatment, sputum is collected for analysis. If bacteria are not detected three times, the person is discharged and his condition is then monitored on an outpatient basis.
If the bacterium is particularly resistant to drugs, making their selection incredibly difficult, the patient may remain in the hospital for one to one and a half years.
The main indications for hospitalization are:
- non-pulmonary form. Treatment is done through chemotherapy;
- pulmonary form, not amenable to outpatient treatment due to the resistance of the bacterium;
- treatment of acute forms of infection;
- the need for surgical intervention.
Diagnosis of pulmonary tuberculosis.
Signs of pulmonary tuberculosis are nonspecific, that is, they can also appear in other diseases.
If you suspect tuberculosis, your doctor will prescribe the following tests:
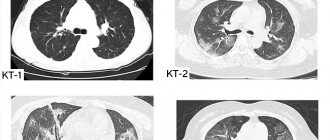
- X-ray of the chest organs (if necessary, computed tomography of the lungs);
- Examination of sputum to determine the presence of the tuberculosis pathogen in it. If the cough is dry, then you have to use various methods of obtaining sputum for research (inhalation with substances that dilute sputum, etc.). The study must be carried out at least three times on different days;
- Tuberculin skin test (Mantoux test). The nurse will inject you subcutaneously into the forearm area with a special drug containing antigens (parts of protein molecules) of the tuberculosis pathogen. This test DOES NOT cause illness. After 72 hours, the doctor will determine the size of the papule (a red round lump slightly raised above the skin) on the forearm, which will help make a more accurate diagnosis.
Based on the results of the studies, a conclusion will be drawn about the presence or absence of the disease.
Historical information
There is plenty of evidence that tuberculosis was familiar in ancient times. Direct evidence is the modified bones of the mummies of Egyptian pharaohs.
In the chronicle of the history of Ancient Greece, there are materials from Hippocrates, who identified the main symptoms of the acute form of the disease: sputum, weakness in the body, weight loss, cough and pain in the chest. The infected were evicted from cities to isolated areas. But both Hippocrates and the scientist Avicenna knew tuberculosis as a disease transmitted only by airborne droplets.
Throughout human history, the name of tuberculosis has varied. It was defined as the “white plague” and “flying death” because it affected a huge number of people. In 1200 BC, the Hindus called it consumption. Marriages with sick women were strictly prohibited. In 1819, the French doctors Laennec and Bailey called the disease “tubercle” (tuberculum). For a long time it was believed that tuberculosis was a non-infectious disease characteristic exclusively of the lower social strata of the population.
On March 24, 1882, the German scientist Robert Koch identified the causative agent of the disease - a bacterium named Koch's bacillus in honor of the researcher. He discovered it while studying the sputum of one of his patients. Robert then experimentally caused this disease in animals, which confirmed the correctness of his discovery. It was Koch who proved that tuberculosis is equally dangerous for representatives of both the upper and lower classes of the population. March 24 has officially received the status of World Tuberculosis Day.
Celebrities who suffered from the terrible disease were actress Vivien Leigh, sister writers (Charlotte, Emily and Anne) Bronte, playwright Anton Pavlovich Chekhov, seventh US President Andrew Jackson, writer George Orwell.
What to do if you have been diagnosed with pulmonary tuberculosis?
- DO NOT PANIC! In most cases, the disease can be cured with the help of modern highly effective drugs;
- Treatment of pulmonary tuberculosis with folk remedies without the use of special anti-tuberculosis drugs is UNACCEPTABLE! None of the folk remedies can cure tuberculosis; for this purpose, special highly effective anti-tuberculosis drugs (antibiotics and antimicrobial drugs) have been developed. Treatment of pulmonary tuberculosis only with folk remedies can lead to death. A clear, but at the same time sad example is famous people of the 19th and 20th centuries. (Chekhov, Perov, Belinsky, Kustodiev, Kafka, Napoleon II Bonaparte, Vivien Leigh, etc.), who died from this disease due to the lack of highly effective anti-tuberculosis drugs at that time;
- Strictly follow all treatment recommendations of a phthisiatrician (a doctor who treats tuberculosis).
Symptoms

Tuberculosis can damage both the respiratory system and other organs of the human body. The lungs are affected in 85% of cases. The symptoms are very similar to any other diseases of the respiratory system, so you need to be extremely attentive to the body to diagnose the disease at an early stage.
Clinical symptoms of pulmonary tuberculosis:
- A dry cough, which, as the disease develops and progresses, becomes wet with the presence of blood in the sputum. Often prolonged coughing attacks occur at night. - The cough lasts for at least 3 weeks.
- Coughing up blood. The bacillus attacks the small arteries that supply the lungs with blood, which is why the blood is released with a cough.
- Sharp chest pain when coughing. It occurs due to irritation of the nerve endings of the pleura, which covers the lungs. In a healthy person, the pleural layers slide relative to each other, due to which inhalation and exhalation occur. The infected leaves are affected by Koch's bacillus, which leads to disruption of the functioning of the respiratory system.
- Increased shortness of breath with any physical activity. The fact is that the bacterium affects the lungs, which means they cannot supply the human body with the necessary amount of oxygen. Shortness of breath occurs as a result of a person’s attempts to inhale as much air as possible, of which he feels lacking.
- Fever (increased body temperature from 37.1 - 38 °C). But most cases are characterized by exceeding the norm by 1-2 degrees in the evening.
- Weakness and malaise as a result of increased temperature.
- Increased sweating at night.
- Weight loss.
A noticeable deterioration in the condition in most cases is observed in the evening and at night.
In children, tuberculosis is accompanied by additional symptoms:
- Enlarged lymph nodes and pain when touching them. This occurs because this is where a large number of bacteria are concentrated.
- Pale skin due to decreased blood supply.
- Sleep disturbances, problems concentrating, increased irritability and mood swings.
The non-pulmonary form of tuberculosis is much more difficult to diagnose:
- The only symptom is a slight but constant increase in body temperature, as a consequence of the body’s fight against the disease.
- Damage to the genitourinary system is characterized by the presence of blood in the urine and acute pain in the lumbar region. The consequence of the disease is infertility in women.
- The presence of blood in feces is also observed when the digestive tract is damaged. This also includes bloating, intestinal obstruction, and pain similar to those observed with pancreatitis or gastritis.
- If the infection affects the nervous system, symptoms similar to meningitis occur. Inflammation of the meninges occurs. The patient feels severe pain when turning and tilting the head, especially strong tension in the occipital muscles.
- If the disease affects the joints and bones, then the person becomes prone to frequent fractures, pathologies appear in the vertebral curves and postural disorders. Movements become constrained. Acute pain occurs in the back and joints.
Forms of pulmonary tuberculosis.
In Russia, a clinical classification is widespread, which includes a large number of forms. We will look very briefly at the following:
- focal tuberculosis (single lesions up to 1 cm in size, usually in the upper lobes of the lungs);
- disseminated tuberculosis (extensive bilateral lung damage);
- infiltrative tuberculosis (localized damage to the lung tissue, reminiscent of pneumonia within several segments, lobes of the lung);
- fibrous-cavernous tuberculosis (severe damage to the lungs with destruction, compaction (fibrosis) and the formation of cavities (cavities) in the lung tissue and disruption of lung function);
- cirrhotic tuberculosis (the outcome of fibrous-cavernous tuberculosis with gross compaction of the lungs (fibrosis), the formation of non-collapsing cavities (cavities) in the lung tissue and severe impairment of all lung functions).
The most unfavorable in terms of prognosis are fibrous-cavernous and cirrhotic pulmonary tuberculosis. One of the reasons is the development of severe respiratory failure due to fibrosis (hardening) of the lungs. Less commonly, massive fibrosis occurs after infiltrative or disseminated pulmonary tuberculosis. Dyspnea in all these cases, as a rule, progresses, which requires long-term oxygen therapy. In case of hypoxemia (decreased oxygen concentration in the blood), which arose due to impaired pulmonary function, the only effective method of improving the prognosis is long-term oxygen therapy using oxygen concentrators. This treatment allows you to maintain the oxygen concentration in the blood at an acceptable level, which helps reduce shortness of breath, increase physical activity and sleep, and improves the prognosis. Unfortunately, lung transplantation for tuberculosis is contraindicated, which further increases the relevance of long-term oxygen therapy.
Call us right now and get quality advice regarding the choice of equipment!
Contraindications for MRI
The main contraindications to the MRI procedure are related to the peculiarities of its implementation. Magnetic resonance imaging is not performed in the following cases:
- the patient suffers from claustrophobia or other problems associated with emotional and mental disorders that will not allow him to lie motionless in a closed cell for a long time. The solution to this problem can be the use of anesthesia, if MRI cannot be avoided. General anesthesia can also be used for diagnostic MRI examinations of young children;
- the patient’s body contains metal implants, pins, plates, a pacemaker and other metal-containing objects;
- pregnancy in the first trimester is also a contraindication, since during this period exposure to a magnetic field can negatively affect the development of the fetus;
- if an MRI with contrast is planned, it is necessary to find out whether the patient is allergic to iodine.
Nutrition rules

The ratio of carbohydrates, proteins and fats in the diet of patients with tuberculosis changes in order to strengthen the immune system.
Preference should be given to slow carbohydrates (cereals, vegetables, fruits). Fast carbohydrates (confectionery) do not have to be excluded, but it is advisable to reduce them to a minimum (no more than 80 g per day).
Proteins are especially important during illness because they are responsible for the production of antibodies. It is recommended to eat lean fish and poultry meat, seafood, dairy products, cattle and fish liver. Proteins should be at least 120-150 grams per day.
Fats take part in the processes of restoration of cell membranes after damage by the bacillus and should be included in the diet in the amount of 50-80 grams per day. Preference should be given to vegetable fats (oil), lard and fish oil. Animal fats are allowed to be consumed, but in small quantities.
Mineral salts (found in tomatoes, figs, herbs, cheeses, cottage cheese and cauliflower) help increase immunity, improve the functioning of the endocrine system and normalize metabolic processes.
It is important to remember: the ratio of proteins, fats, carbohydrates and mineral salts, as well as their required amount, directly depends on the individual proportions and characteristics of each person (body weight, height, age, and so on). Only a doctor can correctly calculate the formula. The information above is general information and may vary from person to person.
Hygiene rules

Since tuberculosis in most cases affects the respiratory system, any contact with an infected person can lead to transmission of the disease. Therefore, those infected with tuberculosis must take care to prevent the risk of infecting others. To do this, be sure to cover your mouth with a handkerchief when coughing and turn away to the side. In public places it is only permissible to wear a surgical mask, changing it as often as possible (mandatorily every 4-6 hours).
If one of your family members is infected, it is important to clean and disinfect living areas daily. Do not come into contact with the patient’s personal belongings. It is necessary to allocate him a separate room, where healthy family members will enter as rarely as possible. Movement of the infected person around the apartment/house is only possible with a gauze bandage on the face. It is important to remove upholstered furniture, toys, carpets and curtains from the patient’s room or use special covers for them. Be sure to boil them periodically.
Preventive measures
The child is vaccinated 3-5 days after birth. It includes about 500 thousand bovine-type bacilli, whose properties, however, are reduced compared to real pathogens. The vaccine is given into the upper left shoulder. A scar measuring up to 8 mm usually forms at this site. Repeated vaccination is carried out at the age of seven years.
The vaccine is not given in the following cases:
- injuries received after childbirth;
- skin damage;
- allergies (there is a danger of respiratory tract spasm);
- elevated body temperature as a result of other diseases.
Tuberculosis is one of the most dangerous diseases of the human body, second only to HIV. Inattention and indifference to one's health can lead not only to death, but also to infection of family and friends. Therefore, only timely initiation of treatment by a specialist, and not attempts to make a diagnosis on your own, will be able to provide timely assistance to the body in the fight against the disease.