The more people who have recovered from coronavirus infection, the clearer it is that for many the disease does not go away without a trace. Even those who have had a mild infection may experience all sorts of unpleasant symptoms. The Ministry of Health is talking about the need for rehabilitation for such patients and is creating a special commission to study post-Covid syndrome. This condition often remains for a long time even in those who were seemingly mildly ill with COVID-19.
At first, doctors advise those who have been ill to return to normal life carefully, take care of themselves, do not overexert themselves, observe a sleep and rest schedule and eat right, and increase the load very gradually.
How to control the consequences of the disease? What tests should I take, what systems should I check? The medical director of the Helix Laboratory Service, Dmitry Denisov, answered these questions for RG - Week.
Indications for biochemical blood tests in children
- diagnosis of diseases of internal organs and systems;
- metabolic diseases;
- diseases of the liver, kidneys, spleen;
- diseases associated with hormonal imbalance;
- infectious diseases;
- acute surgical diseases;
- preparation for surgical operations and medical procedures;
- hereditary diseases and congenital abnormalities;
- preventive (screening) studies;
- monitoring the effectiveness of treatment.
Protein deficiency
Protein deficiency is a painful condition of the body associated with insufficient intake and absorption of protein or with its increased breakdown. A true deficiency in protein intake from food can develop in people who have been undernourished for a long time, adhering to so-called mono-diets, or in vegetarians. Secondary protein deficiency, associated with its increased breakdown, can accompany a number of diseases, for example, severe forms of infectious diseases, burns, kidney pathologies, and hereditary metabolic disorders. Proteins are the main building material of the body, so even mild forms of protein deficiency, which are outwardly asymptomatic, affect the ability to resist infection or the rate of wound healing, slow down the growth of nails and hair, and cause dry skin. Severe protein deficiency can disrupt the normal functioning of all organs and systems. Protein deficiency in childhood is especially dangerous, as it can affect the development of mental abilities, muscle formation, and slow down the child’s growth.
Timely detection of protein deficiency and establishment of its cause is extremely important, as it allows one to avoid life-threatening complications.
Synonyms Russian
Protein deficiency, protein dystrophy, protein-energy deficiency.
English synonyms
Protein Deficiency.
Symptoms
Mild forms of protein deficiency are most often asymptomatic. An exception may be hereditarily determined deficiencies of individual amino acids (structural components of the protein molecule), the characteristic signs of which are observed in early childhood.
External manifestations of protein deficiency:
- general weakness;
- progressive weight loss;
- fragility, dullness and hair loss;
- brittle nails;
- dryness and flaking of the skin;
- swelling.
Manifestations from the nervous system:
- lethargy and increased fatigue;
- headache;
- decreased mental activity;
- unstable mood;
- insomnia.
Manifestations from the musculoskeletal system:
- pain in muscles and less often in joints;
- slow growth (in children);
- reduction in muscle mass and apparent volume;
- muscle weakness.
From the digestive organs:
- increased craving for sweets;
- nausea;
- abdominal pain and bloating;
- stool disorders (constipation followed by diarrhea);
- liver enlargement.
Who is at risk?
- Population of countries with low living standards.
- Vegetarians.
- Persons following a mono-diet or fasting in order to lose weight.
- Patients with kidney diseases.
- Patients with diseases of the digestive system.
- Persons with a hereditary predisposition to protein metabolism disorders.
- Persons with professionally caused weight deficiency: ballerinas, models, gymnasts.
- Persons over 60 years of age.
General information about the disease
Proteins are among the essential nutrients that perform the following functions in the body.
- Construction - protein is part of all cells of the human body and, in fact, is the basis for the existence of life.
- Frame – proteins are involved in the formation of hair and nails, form the protective membrane of the eye, cartilage, tendons and ligaments. Even such a property as the smoothness of the skin directly depends on the protein it contains.
- Motor and contractile. Proteins are the main component of muscle tissue that ensures its functioning.
- Transport. Many proteins have the ability to bind to nutrients contained in the blood and transport them to organs and tissues. An example of a transport protein is hemoglobin, contained in red blood cells (erythrocytes) and transporting oxygen.
- Protective. The body produces specific proteins (antibodies) that provide protection against microorganisms and viruses.
- Enzymatic. Enzymes are proteins that are involved in all chemical processes occurring in the body (for example, in the digestion of food).
- Hormonal. Most of the hormones in the human body are proteins.
The implementation of these functions occurs due to protein metabolism - constantly occurring processes of protein formation (synthesis) and breakdown.
The main causes of protein deficiency:
- Severe and long-term illnesses require the body to use all its reserves. Proteins are spent to replenish energy costs and restore dead cells. In a number of diseases, significant protein loss occurs.
- Chronic kidney disease (glomerulonephritis, renal failure, nephrotic syndrome) can lead to the excretion of significant amounts of protein in the urine (proteinuria), causing a drop in protein levels and chronic protein deficiency.
- Liver cirrhosis and liver failure can cause protein deficiency, especially in the later stages of the disease, when edema develops - fluid containing large amounts of protein (ascites) can accumulate in the abdominal cavity. The liver synthesizes many proteins necessary for the body, and the digestive enzymes it produces are involved in their absorption. With cirrhosis, normal liver function is disrupted and protein deficiency may develop.
- Burns (burn disease). With thermal burns, blisters filled with protein-containing liquid may form on the skin. Protein losses when opening these bubbles can be quite significant.
- Diarrhea (diarrhea) is characterized by a significant loss of fluid and digestive juices containing proteins.
- Malignant neoplasms in late stages can lead to severe protein deficiency. The protein is spent on tumor growth, and is also lost during its decay and bleeding. Substances formed in tumor cells are foreign to the body. Once in the blood, they cause poisoning by decay products (cancer intoxication syndrome), one of the manifestations of which is a drop in protein levels.
- Diabetes mellitus can cause protein deficiency due to increased protein breakdown, as well as diabetic kidney damage and secondary proteinuria.
- Disorders of protein-amino acid metabolism. Proteins are complex substances that, like a chain, are made up of units called amino acids. The sequence of amino acids is individual for each organism, therefore the protein supplied with food during the digestion process is broken down to the level of individual links, from which its own sequence is then composed. At the same time, some amino acids can be formed in the human body, while others (they are also called essential) come only from food. The role of essential amino acids is so great that without them, protein formation becomes impossible. If any essential amino acids are missing from the diet or are not absorbed, the balance between protein breakdown and synthesis may shift toward breakdown and lead to protein malnutrition.
- Impaired digestibility of essential amino acids is a hereditary pathology. The following diseases are most significant in the development of chronic protein deficiency.
- Phenylketonuria is a metabolic disorder of the amino acid phenylanine. Phenylanine is involved in the formation of almost all proteins of the human body, primarily proteins of the nervous system. The disease is characterized by the absence or insufficient level in the liver of a special protein (enzyme) responsible for the absorption of this amino acid. As a result, its excessive accumulation in tissues occurs. Phenylketonuria is usually diagnosed in early childhood and is accompanied by various disorders of the nervous system, as well as retardation in physical development. Without treatment, it can lead to mental disability.
- Tyrosine metabolism. Tyrosine is an amino acid necessary for the formation of one of the main protein pigments of the human body - melanin, therefore one of the manifestations of impaired metabolism is albinism (pale skin, discoloration of hair and iris). Tyrosine is also required for the formation of thyroid hormones.
- Disturbances in protein synthesis can lead to insufficient protein formation or the appearance of so-called defective, or pathological, proteins that are unable to perform their functions. For example, with a hereditary disease such as sickle cell anemia, hemoglobin is detected in the blood, which is not able to carry the same amount of oxygen as normal. Acquired disorders of protein synthesis can be caused by malignant tumors or taking certain medications.
- Alimentary (digestive) protein deficiency is the most common form of protein deficiency. It can develop under the following circumstances:
- Insufficient protein intake from food. Some diets include limiting animal protein (meat), replacing it with vegetable protein, or completely eliminating proteins. Prolonged fasting can also lead to protein deficiency. In the latter case, irreversible protein breakdown may begin, which poses a threat to life.
- Protein digestion disorders can develop in diseases of the gastrointestinal tract, accompanied by insufficient production of digestive juices, for example, in atrophic gastritis with reduced secretory function.
Depending on the severity, protein deficiency can lead to:
- retardation in mental and physical development;
- weakening of memory and intelligence;
- weakening of the body's defense system.
Diagnostics
Protein deficiency may be primarily suspected in patients with underweight, as well as in individuals with symptoms of diseases characterized by protein deficiency. To confirm the diagnosis, a complex of studies is carried out.
Laboratory research
- A general blood test is one of the basic tests.
- The level of red blood cells and hemoglobin may be reduced (anemia) in patients with severe forms of protein deficiency and general exhaustion. A normal content of red blood cells with a low level of hemoglobin can be observed when it is insufficiently formed or excessively destroyed. This condition is called hypochromic anemia.
- Leukocytes. An increase in the number of leukocytes with the appearance of young cells in the leukocyte formula may indicate an infectious-inflammatory process that is the cause of protein deficiency.
- Erythrocyte sedimentation rate (ESR) is also an indicator that indicates an inflammatory process as the cause of protein deficiency.
- A general urine test is essential in excluding or confirming a renal cause of protein deficiency. Includes studying the following parameters.
- Urine color. Normally it is assessed as straw yellow. Red or brown discoloration may occur when blood enters the urine (hematuria) and indicates serious kidney problems. Dark brown urine, especially in combination with jaundice, is characteristic of liver disease.
- Transparency. Normal urine is clear. In case of kidney diseases, it becomes cloudy due to a significant content of pus (pyuria) or salts.
- The specific gravity of urine is an indicator of the efficiency of the kidneys. With protein deficiency caused by kidney damage, it can decrease significantly.
- Protein is normally absent in a urine test. If the test is positive (proteinuria), a quantitative determination of protein in the urine is carried out and its composition is necessarily examined. Albumin is the most commonly detected type of protein, but other proteins may also be detected, such as immunoglobulins, hemoglobin, myoglobin, and others. The degree of proteinuria allows us to indirectly judge the level and severity of kidney damage.
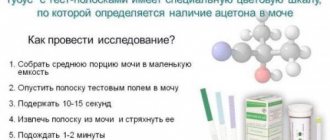
- Urine testing using special test strips is carried out to detect proteinuria - the release of protein in the urine. A positive result may be the first indication of a renal origin of protein deficiency. In this case, microscopy of the sediment is necessary. Urine sediment examination:
- Red blood cells - erythrocytes of protein deficiency caused by kidney pathology, can be present in the urine in large quantities. The presence of altered discolored red blood cells allows one to suspect glomerular damage (glomerulonephritis).
- Cylinders are formed in the renal tubules from protein, leukocytes, erythrocytes, and epithelium. Identification of casts, especially protein casts, may indicate a renal origin of protein deficiency.
- Protein in blood serum. The study is the “gold standard” for studying protein metabolism and confirming protein deficiency. Protein levels in blood plasma and tissues are in a state of equilibrium. With the loss of tissue protein, the level of plasma proteins also decreases, which determines the significance of this parameter.
- Protein fractions of blood serum. Determination of the quantitative composition and ratio of protein types in blood serum. Total serum protein is represented by albumins and globulins, which perform various functions. The main part is albumin, the main building protein of the body. Fluctuations in its level to the greatest extent reflect the state of protein metabolism. Globulins are more specific in their purpose. These are proteins of the defense system, markers of inflammatory reactions and special transport proteins. Under various pathological conditions, the ratio and amount of proteins of one type or another can change significantly, and in some cases additional (pathological) protein fractions appear. Based on the ratio of individual fractions of the protein composition of the blood, one can to some extent judge the cause of protein deficiency. For example, if the liver and kidneys are damaged, albumin levels may decrease. Globulins increase during inflammatory processes, reflecting the activity of inflammation or the immune (protective) system. A decrease in globulin levels may indicate diseases of the renal tubules, and can also be observed with impaired liver function and when the body’s immune system is suppressed (as in severe forms of sepsis).
- Glucose (blood sugar). Determination of glucose levels may be prescribed if protein deficiency due to diabetes is suspected. Kidney damage in diabetes mellitus (diabetic nephropathy), as well as increased protein breakdown, can cause protein deficiency.
- Urea and creatinine in blood serum. These are substances formed during the breakdown of proteins. With intensive protein destruction, their level in the blood may increase. The indicator should be assessed together with the level of urea in daily urine.
- Urea in daily urine reflects the efficiency of the kidneys. With intensive protein breakdown, it can increase significantly. A low level of urea in the urine with an increase in it in the blood is more typical of renal failure.
- Creatinine in daily urine is an indicator of impaired excretory capacity of the kidneys, which is indicated by a decrease in its level. For a more accurate assessment, creatinine clearance is calculated, which is the ratio of its levels in daily urine and blood. In renal forms of protein deficiency, this indicator can decrease significantly.
- Coprogram is a stool examination that allows you to identify possible violations of the main stages of digestion. The chemical composition of feces, their color, smell, consistency are assessed, and certain types of microorganisms (dysbacteriosis) are identified. The analysis allows you to evaluate the activity of the main enzymes of the liver, gastric and intestinal juice, and pancreas. With protein deficiency caused by impaired protein absorption, undigested muscle fibers may be found in the stool.
Additional (instrumental) research methods
The scope of diagnostic tests depends on the suspected cause of protein deficiency and should be determined by the attending physician. The main diagnostic methods include:
- Ultrasound examination of the abdominal organs. A doctor may prescribe it to rule out diseases of the liver and pancreas, as well as kidneys. it combines high information content and safety for the patient. Ultrasound passes through soft tissue to the organ being examined and, after being reflected, returns back. The resulting image is transmitted to the monitor. The study allows you to assess the size of internal organs, the structure of their tissues, identify a tumor lesion or cyst, and exclude the presence of fluid in the abdominal cavity. If necessary, the study can be supplemented with an ultrasound-guided biopsy.
- Esophagogastroduodenoscopy. It is a direct examination of the esophagus, stomach and duodenum. The patency of the upper digestive tract, the condition of the mucous membrane, the degree of its inflammation or atrophy are assessed. During the examination, a piece of tissue may be taken for analysis (biopsy). Along with ultrasound, gastroscopy is mandatory if a nutritional protein deficiency is suspected.
- Daily pH measurements. This is the study of daily fluctuations in the acidity of gastric juice. A probe with a sensor at its end is placed in the stomach, and the information coming from it is recorded by a portable device attached to the patient's belt. The main part of the protein supplied with food is digested in the stomach under the influence of hydrochloric acid and pepsin, an enzyme that breaks down protein. If the acidity of gastric juice is reduced, protein digestion may be impaired.
- Enteroscopy (intestinoscopy). Examination of the small intestine. The study is similar in its capabilities to gastroscopy, but is technically more complex, since it involves examining the entire small intestine. Allows you to assess the condition of the mucous membrane, exclude erosive lesions and take the contents for analysis to exclude an infectious process.
- Colonoscopy is an examination of the large intestine. For protein deficiency, it can be prescribed to patients with suspected intestinal tumors or ulcerative colitis, in which significant protein loss is likely.
Treatment
Treatment of protein deficiency is aimed at replenishing protein volume and normalizing protein metabolism. At the same time, the underlying disease is treated.
It may include the following items.
- Recommendations for a balanced or protein-enriched diet (with sufficient animal protein). Including meat, eggs, fish, caviar in the diet. For patients with protein deficiency caused by kidney disease, liver disease, or diabetes mellitus, the diet should be selected by the attending physician, taking into account the characteristics of the course of the underlying disease. Such a correction of the diet may be the only necessary measure in case of a mild form of protein deficiency.
- Medications:
- solutions containing a complex of amino acids or protein components of blood intended for intravenous administration; treatment with these drugs is carried out under the strict supervision of a doctor in a hospital setting;
- special nutritional mixtures can be prescribed to patients with severe forms of protein deficiency due to diseases of the gastrointestinal tract or in the postoperative period; these are special protein cocktails that are introduced into the stomach or duodenum through a tube when normal nutrition is impossible;
- Digestive enzymes are used for replacement purposes by patients who do not produce enough of them.
Prevention
- A balanced diet with sufficient amounts of plant and animal proteins.
- Mandatory medical supervision during a diet that strictly limits the diet, or during courses of therapeutic fasting.
- Timely detection and treatment of diseases that increase the risk of developing white deficiency.
Recommended tests
- General blood analysis
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- General urine analysis with microscopy
- Rehberg test (endogenous creatinine clearance)
- Urea in daily urine
- Creatinine in daily urine
- Total protein in urine
- Total protein in whey
- Protein fractions in whey
- Serum creatinine
- Urea in serum
- Plasma glucose
- Coprogram
Features of biochemical blood tests in children
Standard biochemical parameters in a child change throughout life. Therefore, in laboratory diagnostics of biological fluids, I usually distinguish four main age periods:
- newborn - first four weeks of life;
- infant - from four weeks to two years;
- child – from two years to puberty;
- adolescence – from the age of puberty to entry into adulthood.
For example, in the neonatal period, the standard values for glucose, calcium and magnesium are lower, while the levels of urea and bilirubin are higher than in other age groups. Newborns and babies born prematurely may have significantly different hormone levels.
The low weight of a newborn or infant, the small size of his body and some other features impose special requirements on the highly qualified medical personnel who collect samples of material for biochemical research. For example, special skill is required for collecting capillary blood from newborns and infants: excessive compression of the capillaries when squeezing out drops of blood can lead to the destruction of its cells, which in turn distorts the picture of the content of potassium, magnesium, phosphates and some enzymes in the blood.
Hemolytic disease (HDN) - symptoms and treatment
The development of hemolytic disease is possible only through contact between the blood of the mother and the fetus. During pregnancy, thanks to the placenta, fetal red blood cells enter the mother's body in small quantities, insufficient for the production of antibodies. At the time of delivery, due to abortion, miscarriage or complicated pregnancies, red blood cells enter the mother's bloodstream in large quantities, which causes the production of class M antibodies (IgM). These antibodies are formed almost immediately after contact with Rh-positive fetal blood. They provide temporary immunity from any foreign substances, but IgM are not able to penetrate the placenta to the baby.
Antibodies of class M are then transformed into antibodies of class G (IgG). They are produced 3 months after contact with Rh-positive red blood cells, provide long-term immunity for several years and are able to pass through the placenta into the fetal blood. This explains the fact that during the first pregnancy, these immune particles are not dangerous for the fetus, because during a normal pregnancy, the child’s blood mixes with the mother’s blood only in the last months of pregnancy or after childbirth, when IgG has not yet been developed.
During the first pregnancy, only recognition of the fetal red blood cells occurs, i.e., a primary immune response, which is also called “irritation” of the mother’s immune system. The term “sensitization” is also used for this process, and when applied to Rh conflict - “Rh sensitization”. The primary immune response is not dangerous to the fetus.
As a rule, a conflict regarding the Rh factor develops during a second pregnancy. This is due to the fact that by the time of the next conception, class G antibodies are already present in the mother’s body, so they begin to attack the red blood cells of the fetus already in the early stages. In this regard, the likelihood of developing this disease, as well as its severity, increases with each subsequent pregnancy. The disease occurs in 63% of children from women with sensitization.
It is important to understand that in the case of an abortion during the first pregnancy, regardless of the method used, the likelihood of sensitization (antibody production) in women with a negative Rh factor increases significantly. At the same time, the risk of infertility increases.
Maternal antibodies destroy fetal red blood cells in the liver and spleen, which disrupts the functioning of these organs. With a large amount of antibodies, damage to red blood cells occurs inside the vessels. In response to the death of red blood cells, the liver, spleen and bone marrow begin to produce reticulocytes (red blood cell precursor cells), which leads to their increase. This explains the development of symptoms of anemia and hepatosplenomegaly (enlarged liver and spleen) [7].
The breakdown product of red blood cells is indirect bilirubin, a bile pigment. Bilirubin is a toxic enzyme that damages the tissues of the brain, liver, lungs, kidneys, etc. A critical increase in the level of indirect bilirubin leads to irreversible damage to brain structures - bilirubin encephalopathy (kernicterus).
Factors in the development of kernicterus are prematurity, infections, hypoxia (lack of oxygen in the fetus), metabolic disorders (low or increased blood glucose levels), hemorrhages, taking certain medications (sulfonamides, salicylates, furosemide, diazepam, etc.) and alcohol consumption [2].

What to do so that your child is not afraid of taking blood from a vein or finger:
Blood tests can cause some fears in children (children may be afraid of pain or the sight of blood), so try to tell your child in advance that no harm will come to him.
The medical staff of our center is excellent at working with small children, you don’t have to worry, the blood will be drawn quickly and professionally, our nurses try to take blood from both a vein and a finger so that the kids are not afraid and do not cry.
For mothers: if you are worried that your baby will not react well to taking blood from a vein or from a finger, you can first play “tests” with your child at home on a soft toy, showing how the procedure for taking blood from a vein goes. Repeating the game procedure with your child several times will significantly reduce the level of fear from the unknown of the upcoming procedure.
While collecting material for research from a child, stay close to him, diverting his attention by verbally counting or repeating the alphabet.
What symptoms should parents be wary of?
If in children under the age of one year a temperature of 37.2°C is considered normal, then as the child grows older, such indicators cease to be considered normal. As a rule, in addition to an increase in body temperature to subfebrile levels, the child may be bothered by:
- lethargy and apathy, the baby is not as active as usual;
- poor appetite, refusal of food and water;
- restless sleep, nervousness and moody behavior before bedtime;
- increased sweating, clothes become wet after sleep;
- confusion and rapid breathing.
We draw the attention of parents to the fact that the temperature does not indicate the severity of the disease. The symptoms listed above speak about this best.
How is blood taken for biochemical studies?
Blood is collected from newborns from the heel by puncturing the skin with a thin children's scarifier. In infants older than one month, blood is taken from the cubital vein.
In all cases, the nurse treats the surface of the skin with an antiseptic spray or solution. To increase the amount of blood in the vein before the study, it is briefly clamped with a tourniquet (soft tourniquet). Then a thin needle is inserted into the vein, through which the blood flows into a test tube or syringe. After blood collection, the injection site is treated with an antiseptic, and a bandage or plaster is applied to it.
Decoding and interpretation of the results of biochemical blood tests
The printout of the results of the study of biochemical parameters provided by the laboratory will indicate the levels of the test substances in the blood plasma and the normative indicators for the child’s age.
The results obtained should be assessed by the pediatrician or medical specialist who ordered the study. Based on the biochemical tests obtained, the doctor will prescribe treatment or suggest additional studies to clarify the diagnosis.
Biochemical studies are an informative, fast and safe method of studying the state of the child’s body and the functioning of individual internal organs and systems, which allows you to accurately establish a diagnosis and carry out the required treatment with maximum efficiency, or get rid of worries and doubts about the state of your baby’s health.
You can get additional information about biochemical studies and sign up for tests at the medical office by calling.
Is it necessary to lower the temperature to 37.5 °C?
It's no secret that an increase in temperature is the body's immune response to infectious aggression that has entered the body. At elevated temperatures, pathogenic viruses and microbes die, so it is not recommended to bring it down to 38°C.
These thermometer readings are not a reason to take antipyretics; it is better to give the body the opportunity to use its own defense mechanisms as efficiently as possible.
It is possible to bring down a low-grade fever only if it is poorly tolerated by the child, there are signs of severe intoxication, or there is a high risk of developing cardiac complications. In such cases, it is necessary to consult a doctor as soon as possible.
However, at a temperature above 38.5°C, it is already worth taking measures to reduce it, as the situation may become more complicated.