Problems in the functioning of the osteoarticular system, unfortunately, affect people of any age. A child’s body has its own peculiarities in the structure of bones, which is why the fetus may experience and develop pathologies of bones and joints while it is in the womb, as well as at the time of birth - they are called congenital. Such pathologies include hip dysplasia. Being detected in the early stages of life, this disorder of the structure of the articular apparatus can be easily corrected and does not entail any threat to health. However, if dysplasia is not detected in the first months of a child’s life and treated, in severe cases it can even lead to the child’s disability. One of the effective methods for diagnosing dysplasia is radiography of the hip joints in children.
X-ray of the hip joints: the essence of the method
Classic X-ray examination is based on the ability of specific R-rays to pass through solid objects of different densities with different intensities. Radiation of this type was discovered at the end of the 19th century, and after 15-20 years it began to be used in medical institutions for diagnostic purposes.
Content:
- X-ray of the hip joints: the essence of the method
- What is dysplasia and why diagnose its presence?
- Stages of joint dysplasia
- In what cases are children prescribed x-rays of joint joints?
- Risks and dangers of performing an X-ray of the hip joint in a child
- Preparing the child and technique of the procedure
- The process of deciphering survey results
- Additional and alternative methods for examining the condition of joints
The patient is examined using a special device. The patient is placed in the beam projection area, and the image is captured, as if photographing the patient. Instead of photographic film, X-ray film is used, treated with a chemical composition containing silver bromide; instead of a camera, a device with an X-ray tube producing R-rays is used.
The images obtained in this way are highly accurate and informative; bone formations and joints, in particular the hip, are especially well and clearly visible.
Contraindications
Despite the fact that the influence of dangerous rays on the human body during X-rays is minimal, the stress of the study can lead to genetic mutations of cells. This is in no way a reason to refuse this procedure. You just have to approach it carefully, following all the techniques and following the indications. There are practically no contraindications for radiography, which is performed to determine the diagnosis. You just need to remember that not everyone can do it.
Self-prescribing an x-ray procedure without consulting a doctor is prohibited. Interestingly, even pregnant women and young children undergo radiography in cases where other recognized methods do not help establish a diagnosis and determine the cause of the patient’s sting. It is advisable for breastfeeding mothers to express milk before the procedure.
What is dysplasia and why diagnose its presence?
Out of one hundred newborn children, three are born with dysplasia of the joint joints. A feature of the infant’s musculoskeletal system is the presence of more cartilage tissue than bone. The baby's bones do not yet contain a sufficient amount of calcium; they are more flexible than those of adults. Therefore, children’s fractures are not the most common phenomenon, while dislocations and subluxations are much more common among them.

Dysplasia is a congenital disorder of the anatomical structure and development of the hip joint. Pathology can cause impaired mobility and chronic hip dislocation. Doctors do not yet have accurate information about what exactly causes it to appear. It is believed that the disorder develops in the fetus at 2-3 months of pregnancy. This may be due to past infectious diseases, unfavorable environmental conditions, exposure to toxins and bad habits, such as drinking alcohol or smoking.
Another theory suggests that the formation of chronic subluxation of the hip joint is facilitated by excessive accumulation of oxytocin, a pregnancy hormone that triggers the onset of labor. It is produced in the body of the expectant mother by the third trimester of pregnancy, and causes an increase in muscle tone in the fetus, which is why dysplasia develops.
The appearance of such a diagnosis is especially facilitated by the presence of the fetus in the womb with its legs crossed.
The risk of developing pathology increases the incorrect position of the fetus in the womb, as well as the factor of hereditary predisposition.
In some children born with dysplasia of the TJ joint, its reduction occurs arbitrarily immediately after birth.
In essence, dysplasia is a discrepancy between the articular surfaces. If the child lies with his legs crossed, the acetabulum and the surface of the femoral head are not in direct contact during development. Even normally, the joints and bones of the fetus are not particularly stable - this is due to the need to facilitate its passage during childbirth. However, with dysplasia, the development of joint ossification points occurs late, and the ossification nuclei are smaller in size than normal. Their vertical-lateral displacement relative to the normal position is clearly visible visually. Dysplasia is also characterized by a slowdown in the ossification process.
The development of dislocations and subluxations of the articular joints is also possible during childbirth, since the joint in a newborn consists of cartilage tissue, and the degree of correspondence between the shape and size of the articular surfaces (joint congruence) is low. The size of the femoral head does not correspond to the size of the acetabulum, the ligaments are inelastic. All this contributes to the appearance of hip dysplasia in children.

If the pathology is not detected immediately after the birth of the child, it will be more difficult to work on correcting it in the future. When the child begins to walk, dysplasia manifests itself as lameness; There is also a noticeable difference in the length of the baby’s legs.
Once a child reaches three or four years of age, it becomes much more difficult to cure dysplasia. In adulthood, it is no longer possible to correct the pathology. Moreover, due to improper formation of the articular apparatus, a person may experience lameness, gait disturbances, and pain. Dysplasia increases the risk of hip fracture and contributes to faster wear and tear of the joint, which can lead to disability.
Indications
X-ray of tubular bones is one of the most effective methods to identify abnormal bone structure and violations of its integrity. He diagnoses various pathologies. This could be a fracture or more serious diseases: a tumor, an infection of bone tissue. This procedure also allows you to accurately determine the location that is affected, as well as the severity of the lesion.
Indications for X-rays of tubular bones are:
- swelling of the tissues on the bones after an injury;
- pain in the bone of unknown nature;
- vague results visible in the picture taken immediately after the operation;
- suspicions that malignant tumors have formed in the carpal tissue;
- doctor's appointment.
An X-ray is needed to determine what kind of injury the patient has: a dislocation, a crack or a fracture. It is also prescribed to detect diseases that affect joints and bone tissue, abnormalities in the structure of bones, and violations of their functionality. Using radiography, doctors monitor the development of the skeleton of children and monitor the aging process.
Stages of joint dysplasia
Depending on how susceptible the articular apparatus and its parts are to pathology, the following stages of dysplasia are distinguished:
- preluxation: the mildest degree, when the head of the femoral bone can move inside the acetabulum, and the joint itself is characterized by instability;
- subluxation: the stage when anatomical and morphological changes begin to form, the head of the femur moves away from the glenoid cavity, but remains within the limbus (a cartilaginous plate that prevents the head from moving upward);
- dislocation: in this case, the head of the femur completely comes out of the socket of the joint, while the limbus moves upward, and the ligaments of the joint are stretched.
When should the examination be carried out?
While the child is not walking, it is difficult to identify symptoms of dislocation or pre-dislocation. However, there is one external manifestation: free dislocation in the hip area and a click during reduction, which is also very easy. When a child begins to walk, asymmetrical skin folds and different leg lengths become noticeable. In sleep, when the muscles are relaxed, the leg takes a slightly outward position.
Important!
If a newborn baby's hips are spread apart, they should lie on the changing table. At a slightly older age, the deflection angle should be 60 degrees. If this figure is lower, this is a reason to consult a doctor.
In what cases are children prescribed x-rays of joint joints?
Responsibility for the health of the child from the first days, in addition to the parents, lies with the neonatologist and pediatrician. These doctors conduct the very first examination in the baby’s life. As for the orthopedist, parents and the child should see him no later than a month after his birth.
However, even before visiting an orthopedist, the parents or pediatrician themselves may suspect dysplasia during the initial examination. This is possible in severe forms of the pathology, if the head of the femur completely protrudes from the acetabulum. If dysplasia does not affect the articular apparatus so severely, only a specialist with appropriate qualifications can determine it.
Signs that should alert parents and pediatricians:
- impaired joint mobility, difficulty spreading the hips, to the point that the child cries when trying to move the leg to the side;
- asymmetry of the inguinal and gluteal folds: on the side where the joint is affected by dysplasia, they are more pronounced;
- shortening of the leg, if the pathology is developed in only one joint;
- clicking symptom: the head of the femur pops out of the socket of the joint with a characteristic sound when the child bends the legs at the knee and hip joints.

Diagnosis of pathology can occur directly in the maternity hospital, while the child is there with the mother after childbirth. Dysplasia can be identified by an orthopedist during the first appointment. In any case, if any of the doctors detects signs of dysplasia in a child, it becomes necessary to visually assess the degree of damage to the joint, its structure, the shape of its components and how they come into contact. For these purposes, the doctor sends the baby for diagnostic examinations.
X-rays of the hip joints in children are not performed in every case. Due to the fact that the procedure involves x-ray exposure of the patient, children under the age of three to four months are not recommended to undergo x-rays at all. An orthopedic surgeon may prescribe preventive measures without x-rays, for example:
- use of soft tires with spreading mechanisms;
- massage of the gluteal muscles;
- course of special therapeutic gymnastics.
In each specific case, the doctor decides whether to send the child for an ultrasound of the joint or for an x-ray. Some doctors are guided by the principle “any diagnosis is better than no examination and treatment.” X-rays are advisable if the benefit from the information received outweighs the likely threat to the baby’s health from radiation exposure. Otherwise, the doctor gives the little patient a referral for an ultrasound of the joint.
Preparation for radiography of long bones
Mostly, x-rays of tubular bones do not require any special preparatory procedures. During the examination, you need to completely expose the part of the body that will be irradiated. A special shirt must be put on first and given to each patient in the office. It is also necessary to remove jewelry, dentures, and metal items. They negatively affect the image quality of the photo.
A woman must provide the radiologist with information about a possible pregnancy. This is necessary in order to take all measures to protect the fetus.
Risks and dangers of performing an X-ray of the hip joint in a child
Before the onset of puberty, it is believed that radiography is indicated for the patient only in exceptional cases. In addition, an interval of at least 6 months must be observed between procedures. Prescribing hip x-rays in children more than twice a year is not recommended.
Contraindications for radiography for a baby are:
- immunodeficiency and other disorders of the immune system;
- predisposition to cancer;
- metabolic disorders;
- obvious atrophy of organs or muscles;
- diagnosed pathologies of the bone apparatus.

This diagnostic method may negatively affect:
- germ cells;
- bone marrow cells;
- eye lenses;
- epithelial cells that form the mucous membranes of organs and skin;
- organs of the endocrine system.
Despite this, the method of x-ray examination of joints in children is still used by doctors if necessary, as it is the most effective and objective of the existing ones. It is this that allows you to determine the presence of dislocation or dysplasia with an accuracy of up to 75%.
When should an x-ray be taken?
For children, this study is most often performed in cases of trauma, including birth trauma. Often this is the only method that helps identify life-threatening pathologies. The following doctors can refer you for this procedure: oncologist, neurologist, traumatologist, surgeon, ophthalmologist, endocrinologist. Symptoms and indications for examination are:
- headache;
- tremor (shaking) of hands;
- nosebleeds;
- darkening of the eyes;
- dizziness;
- decreased vision or hearing;
- fainting;
- facial asymmetry;
- suspicion of a malignant tumor;
- recent injury;
- some endocrine diseases;
- congenital pathologies.
Pictures are also taken during treatment to monitor the effectiveness of the therapy.
Preparing the child and technique of the procedure
There is no need to carry out any specific preparatory measures before taking x-rays of the hip joints. For very young patients, you need to follow a normal sleep and feeding schedule. For children older than a year or a year and a half, you can clearly and generally explain what will happen during an x-ray, tell them that the upcoming procedure is painless and there is no need to be afraid of it.
The child lies on his back during the x-ray. In this case, the patient’s legs should be straight and straight and should not be bent. In newborn babies, the legs move closer to the body and move slightly inward.
If the child’s pelvis is tightly pressed by the cassette to the plane of the couch or table, his movements will not interfere with the recording of the image. The genitals are covered with a protective lead apron to prevent exposure to X-ray radiation.
If there are no contraindications to the use of anesthesia, the procedure can be performed with the young patient under general anesthesia to ensure the accuracy and quality of the images.
The psychology of choice or about our fears and insecurities
Today there are many methods for studying internal organs: from the familiar ultrasound and x-rays to the most modern computed tomography or magnetic resonance imaging. Many mothers try by all means to avoid any, absolutely any research based on methods originally from physics. It is not difficult to imagine what this can lead to: if diagnosis is delayed, any disease is more difficult to cure, and the outcome is unpredictable. Diagnosis in a newborn is especially difficult: after all, the baby cannot say what is bothering him.

Here are simple arguments that will help you make the right decision. They are based simply on common sense, nothing more.
- We live in a world where dangers await us at every step and this must be recognized as a given. The source of danger for mother and newborn can be low-quality products, stuffed with chemicals, toys made of harmful plastic, unregulated pedestrian crossings, terrible drafts, inadequate grandparents, nosocomial infections, polluted air in the city and the invasion of aliens, in the end. Advice one: stop being afraid of everything.
- Tip two: choose a doctor, not a diagnostic or treatment method. You need a doctor whom you completely trust and only he can choose the most appropriate examination method for the child, based on his knowledge and experience. If the pediatrician insists that a newborn needs an x-ray, then so be it. Trust does not prevent you from asking 100,500 clarifying questions, but all responsibility for the decision lies with the doctor. Where can I find a smart doctor? Well, you’ll have to look if you value the health of your newborn and your own.
The son was treated to an apple. He silently takes it and looks at me. - What do you need to tell your aunt? -Did you wash it?
- If you have been sent for an x-ray, it is not a sin to ask how modern the equipment in your clinic or hospital is. If there is no particular urgency in the examination, it is worth looking for an X-ray room with the most modern equipment and an intelligent radiologist to boot (to avoid a repeat visit).
- Of all the possible “evils”, choose the lesser and act energetically! If your baby is sick, you need to get an X-ray as quickly as possible, and not be overwhelmed by the opinions of strange characters you read on social networks and forums, who are simply nobody to you.
This video shows a detailed discussion about x-rays:
Sometimes a trip to the bakery is fraught with many more dangers than a visit to the x-ray room. This is the last thing you need to know about x-rays.
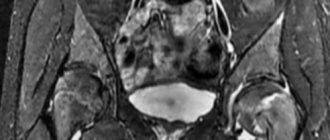
The process of deciphering survey results
After the radiologist receives the X-ray images, he needs to interpret them and draw up a conclusion.

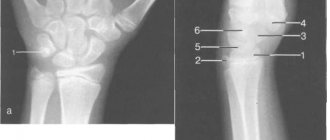
To decipher the results, there is a special technique called the Hilgenreiner scheme. It contains the following categories:
- acetabular angle;
- Hilgenreiner line;
- the distance between the metaphyseal plates and the Hilgenreiner line, denoted by the letter h;
- the distance from h to the lower contours of the vestibular plate, denoted as d.
The acetabular angle is defined as the area between two planes - the line of epsilon-shaped cartilages and the tangent running along the edge of the glenoid sockets.
Hilgenreiner's line is drawn horizontally through the Y-shaped cartilages along the lower points of the ilium.
Distance h is measured from the Hilgenreiner line to the middle of the metaphyseal plate of the proximal femur. It can be used to track how much the head of the femur is displaced in relation to the socket of the joint.
The d gap shows the lateral displacement of the head compared to the acetabulum.
The diagram makes it possible to represent the joint in a three-dimensional projection. Even at the earliest stages, it makes it possible to detect most pathologies and disorders of joint development.
For greater reliability, the scheme provides for additional indicators - the Calvet and Shenton lines. The first of them connects the upper edge of the femoral neck with the outer edge of the ilium, and normally it should be continuous. If the line is interrupted, this may indicate a lack of integrity of the articular apparatus.
Shenton's line is a continuation of the circumference of the acetabulum, in the form of a projection onto the medial surface of the femoral neck. Its rupture means lateral-proximal displacement of the femur.
There are also auxiliary schemes for deciphering radiographs of the joint in children - the Reinberg scheme and the Ombredan scheme.
How is an X-ray of a child’s hip joint interpreted using the Reinberg scheme?
This image interpretation technique uses the midsacral line, a horizontal line through the apices of the Y-shaped cartilages and the centers of the ossification nuclei in the femoral heads (line A), and a vertical line through the superolateral prominence of the acetabulum (line B) . In addition, determining the normal condition of the joint is associated with the location of the lower edge of the femoral neck - with normal development of the joint, it crosses the lower contour of the groin bone.

An auxiliary line B1 is drawn between line B and the median sacral line, the length of which helps to assess the condition of the joint.
Dysplasia is determined if the proximal end of the femur is above line A and as if outside of plane B.
What is the Ombredan scheme?
In the process of examining the results of radiography, the doctor draws a horizontal line along the synostoses in the image, connecting the pubic and ilium bones. A vertically lowered perpendicular is drawn to the outer edge of the acetabulum of the joint. This perpendicular divides the articular cavity into equal segments, in relation to which the compliance of the anatomy of the joint with normal indicators is assessed.
Normal and deviations in the image of the hip joints
The resulting image of the joint, if it is in a normal state, visualizes the head of the femur located in the glenoid cavity, which has the appearance of a notch. In the center, the head is attached to the surface of the cavity by the round ligament and joint capsule. From above, the head is held in its normal position by the limbus, a cartilaginous plate. The entire articular apparatus is supported externally by the muscular corset of the thigh.
Dysplasia in the image is characterized by a delay in the development of ossification. Ossification nuclei are small in size compared to normal. Dislocation or subluxation can be detected by the lateral and vertical displacement of these nuclei, thanks to the use of Ombredan, Reinberg, and Hilgenreiner schemes.
Research methodology
The radiologist or nurse places the patient on the table. Sandbags or pillows are used to keep the patient's body in the correct position. The pelvis and mammary glands are covered with a lead apron.
The patient is instructed to remain motionless and not even to breathe during the second of the image. After the photo is taken, the patient is asked to change position to take a photo of the bone in a different projection.
Sometimes a picture of a healthy, similar bone is also taken so that the results can be compared. The whole procedure takes no more than 10 minutes.
What pathologies can this examination reveal?
- Inflammatory processes in the lungs of various origins.
- Tuberculosis, which in children most often looks like multiple small (2–3 mm) lesions in the thickness of the tissue.
- Cysts in the lungs caused by malformations or parasites.
- Lung abscesses and enlargement of surrounding lymph nodes.
- Impaired lung expansion in newborns.
- Congenital defects in the structure of the respiratory system.
- Air or liquid between the layers of the pulmonary membrane, trapped there as a result of injury.
- Bronchiectasis.
- Signs of bronchial asthma.
- Tumor lesions of the chest organs.
- Injuries to the ribs, collarbones or vertebral bones.
- Some heart pathologies.
Advantages of children's x-rays in Ryazan at the SM-Clinic branch
- We use modern digital X-ray machines that take high-resolution images that increase the diagnostic value of the examination.
- Our equipment, while maintaining the quality of the results, provides 10 times less radiation exposure to the child’s body than film devices.
- Our clinic employs the best radiology specialists in the city.
- By coming to us for a paid examination, you will save yourself and your children from wasting time in queues.
- With us you can do a chest x-ray even for an infant.
- You will receive the diagnostic result on the same day.
If you are looking for where to get a paid x-ray of a child’s lungs in Ryazan or your child needs to undergo fluorography, then contacting SM-Clinic will be the best solution. To sign up for an examination, call tel.
| Name of service | Price, rub.) |
| X-ray of the chest organs in lateral projection | 500 |
| X-ray of the chest organs (survey) | 700 |
| X-ray of the chest organs in 2 projections | 900 |
How is an X-ray performed?

The tactics of the procedure depend on the area being examined and the examination method. Most often, the small patient takes a horizontal position on his back or side. In some cases, the child needs to take an upright position.
X-rays are taken for children in a matter of seconds, but it is important for parents to know at what age their child is able to remain still for short periods of time. In some cases, young patients need to be calmed or even “lulled to sleep.”