Last year, more than 61 thousand new cases of tuberculosis were identified in Russia. How not to add to these statistics?
Despite the persistent downward trend in morbidity and mortality, Russia is still among the 30 countries with the highest prevalence of tuberculosis. The call of doctors to regularly undergo examinations for tuberculosis is more than justified, and here are 10 facts to confirm this.
Fact 1: standard of living is not that important
Tuberculosis has long been considered a disease of people with a low standard of living. This belief has given rise to the problem of stigma, which experts now call one of the main obstacles in the fight against tuberculosis: fear of publicity forces many to hide the diagnosis, even at the cost of refusing treatment. In reality, the standard of living no longer affects the risk of infection with Koch's bacillus, which causes tuberculosis. According to WHO, a quarter of the world's inhabitants are infected, and not all of them are below the poverty line or in prison. However, social status, according to experts, can affect the likelihood of developing tuberculosis and the effectiveness of treatment. The process can be triggered by poor nutrition, for example, or stress, from which, however, no one is immune. The problem of adherence to treatment is acute - patients with low social status are more likely to refuse treatment or interrupt it.
Fact 2: A few bacteria are all it takes
A modern person living in a city has many chances to become acquainted with the tuberculosis bacillus. The very fact of the meeting, however, does not mean that tuberculosis is inevitable: this may not happen, because the human immune system can suppress the infection.
The large percentage of the population infected with Mycobacterium tuberculosis is explained, among other things, by its resistance to external conditions. For example, they can live in street dust for up to 3 months, in indoor dust for up to a year, and in warmth, humidity and without sunlight for more than 5 years. The tuberculosis bacillus feels comfortable in water and on any surfaces, for example, in the house, if there is no general cleaning with chlorine-containing products. The patient releases mycobacteria into the environment in a completely normal way - with particles of sputum. It is not necessary to spit blood at your feet - this will happen every time you cough, sneeze, and even talk. In case of close contact in a home, office or closed institution, this is quite enough, and in a year the patient can infect an average of 10-15 people. To become infected, you only need to inhale a few mycobacteria.
Fact 3: Smoking and diabetes increase risk
According to statistics, only 10 percent of people infected with mycobacteria become ill during their lifetime. There are circumstances that increase the likelihood of developing tuberculosis. Here they are:
- HIV infection
- diabetes mellitus, peptic ulcer
- long-term use of certain drugs - glucocorticoids, cytostatics, immunosuppressants
- smoking
- active alcohol consumption
- childhood and adolescence
- difficult stressful working conditions, unemployment
Fact 4: Some won't get sick, but they are few.
There are people in the world with genetic resistance to mycobacteria - about 2 percent of them. In their case, the immune system reliably suppresses the growth of the tuberculosis bacillus. For such people, the risk of developing tuberculosis is zero. The absence of a scar after vaccination and revaccination with BCG and a consistently negative Mantoux test speak in favor of congenital resistance. Although in most cases the absence of a scar or reaction to the Mantoux test is still explained by the fact that there was no BCG, the vaccine was administered incorrectly, or its storage conditions were violated and it simply did not work. Also, the scar may be almost invisible after administration of BCG-M (a “gentle” immunization vaccine).
Fact 5: There may not be a cough
Symptoms that should alert you and become a reason for examination for tuberculosis are causeless weight loss, fever, night sweats, chronic cough not associated with ARVI. There is a strong opinion among people that cough is the main symptom. A neighbor is coughing - this is suspicious. A loved one began to cough - it’s time for fluorography. Nobody is coughing - everything is fine. In fact, tuberculosis, like many serious diseases, does not have any symptoms in the early stages, or the above may be present in a mild form that does not cause concern. Cough occurs when lung function is impaired. That is why screening for tuberculosis should be carried out regularly, and not on demand.
Fact 6: examination is not just one analysis
A diagnosis such as tuberculosis is not made either by the results of one test or analysis, or by the conclusion of one doctor. This is a multi-step process. Here, for example, is how everything happens in children.
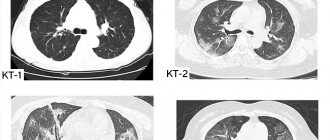
- Up to 7 years of age, a Mantoux test is done.
There are no general standard criteria for assessing the size of a papule; it is always carried out taking into account previous indicators. If the result changes from negative to positive, the sample is said to have swung. This does not mean that the child may have tuberculosis. After 8 years, Diaskintest is performed. According to the Order of the Ministry of Health of the Russian Federation No. 124n dated March 21, 2021 “On approval of the procedure and timing of preventive medical examinations of citizens in order to detect tuberculosis” and the Federal clinical recommendations (Moscow, 2016; 2018), currently used in children and adolescents for the purpose of screening for LTBI immunological tests based on the specific interaction of antigens and antibodies. For children under 7 years of age (inclusive) - this is a Mantoux test with two tuberculin units (2TU), for children over 8 years of age - a test with a recombinant tuberculosis allergen (test with ATP) - the drug Diaskintest. - If the Mantoux test is outside the normal range, Diaskintest or laboratory tests are prescribed. If the result is negative, the examination is stopped. If positive, the child is required to be examined by a TB specialist and undergo further examination - blood, urine, and, if possible, sputum tests, as well as computed tomography. The goal is to rule out or confirm an active process.
- If CT results are normal, latent tuberculosis therapy is carried out - in the hospital or at home. If an active tuberculosis process is confirmed, the case is examined by a special medical commission, which sends the child for treatment to a hospital.
Fact 7: there is a pre-disease that needs to be treated
Latent tuberculosis is a kind of pre-disease: the Koch bacillus is already multiplying, but the person has not yet released it into the external environment. In this case, X-rays and CT scans do not show tuberculosis lesions in the lungs, but a blood test or intradermal test will be positive. The problem is that an adult is usually limited to fluorography and, in the absence of other symptoms, is no longer examined. However, with latent tuberculosis, despite the patient’s normal state of health, doctors prescribe preventive chemotherapy to prevent the disease from developing.
Fact 8: Tuberculosis is curable
Tuberculosis is treated and cured. The course of treatment lasts on average six months, a combination of several antibiotics is used, 3 weeks after the start of therapy the patient stops releasing mycobacteria into the external environment. A certain lifestyle is important - scrupulously following the doctor’s instructions, a protein-rich diet, a daily routine, and normal rest. Therefore, even in those countries where long-term hospital stays are not practiced, the treatment process is controlled by a medical worker or volunteer.
Fact 9: People still die from it
Despite advances in the treatment of tuberculosis, it is still one of the 10 leading causes of death on the planet - along with stroke, COPD, diabetes, lung cancer and road accidents. The main reasons are late detected disease (two thirds of patients die without treatment), incorrect prescription of drugs or their poor quality, low adherence to treatment in certain categories of patients, as well as drug-resistant forms (MDR-TB). According to WHO statistics, in the EU countries, where the situation with such tuberculosis is better than in the region as a whole, the success rate of MDR-TB treatment does not exceed 45 percent.
Fact 10: You can't stop
The number of patients who stopped therapy at their own request in some regions of the Russian Federation reaches 53 percent. This is one of the causes of drug-resistant tuberculosis. Almost half of such cases in the world occur in three countries - India, China and Russia.
The two most effective first-line drugs for treating tuberculosis infection are rifampicin and isoniazid. Drug-resistant tuberculosis is said to occur when mycobacteria no longer respond to one or both of them. MDR-TB can develop not only against the background of improper therapy, but you can become infected with resistant tubercle bacilli. Treatment regimens for such tuberculosis exist, but they are incomparably more expensive, more complex and longer, and the prognosis is worse. In addition, the resistance of Koch's bacillus can be broad, that is, it can extend to a larger number of antibiotics. According to WHO, such tuberculosis is officially registered in 117 countries around the world. Often there is nothing to treat a patient with extensive drug resistance. That is why it is extremely important not only to diagnose tuberculosis in time, but also to treat it correctly.
COMPARATIVE TABLE OF SCREENING METHODS FOR TUBERCULOSIS DIAGNOSIS
| Mantoux test | Diaskin test | Quantiferon test | T-SPOT.TB | |
| Research method | Skin test | Skin test | Blood test from a vein | Blood test from a vein |
| Adverse reactions | Possible | Possible | No | No |
| Contraindications | Eat | Eat | No | No |
| Result evaluation | Subjective | Subjective | Objective | objective |
| False positive result after BCG | Often | Absent | Absent | Absent |
| Detects the stage of tuberculosis | Active | Active | Latent and active | Latent and active |
| Use during pregnancy | Forbidden | Forbidden | Allowed | Allowed |
T-SPOT.TB
T-SPOT.TB is a modern method of immunological diagnosis of latent tuberculosis infection using a blood test.
T-SPOT TEST FOR TUBERCULOSIS METHOD IS RECOMMENDED:
- If the patient refuses to undergo skin tests and fluorography;
- If extrapulmonary forms of TV are suspected;
- If the patient is found to have an allergy to tuberculin (according to the medical history), allergic diseases, skin diseases, epilepsy, acute and exacerbation of chronic diseases;
- Patients for whom subcutaneous tests are contraindicated or difficult due to exacerbation of the underlying disease.
- When a false positive Mantoux reaction is detected in children vaccinated with the BCG vaccine.
- In people who have visited countries with high incidence of tuberculosis (Africa, Asia)
- In pregnant women in case of contact with a patient with tuberculosis or presence of symptoms;
- Patients with HIV infection, especially those with a reduced level of CD4 protein cells;
- For tumor diseases, if a person is undergoing radiation or chemotherapy treatment
- For autoimmune and other pathologies leading to immune suppression;
First signs
The very first signs of pulmonary tuberculosis vary depending on the form, stage and localization of the process. In 88% of cases, the infection takes a pulmonary form.
Symptoms of pulmonary tuberculosis in the initial stage of its development:
- sudden weight loss;
- presence of blood in sputum;
- cough with phlegm for 2–3 weeks;
- periodically elevated temperature up to 37.3 °C;
- night sweats;
- general weakness and loss of strength;
- chest pain.
The initial manifestations of tuberculosis infection can be mistaken for any other disease. If the patient does not consult a doctor in a timely manner, the tuberculosis infection will progress and spread in the body. That is why it is so important to undergo periodic fluorography, which will promptly identify the source of the disease.
T-SPOT.TB: who needs it and when
All existing tests can be divided into two groups – screening and confirmatory. The main advantage of the former is their low cost; screening examinations should cover as many people as possible. In adults, screening for tuberculosis is fluorography. However, it can only detect lesions in the lungs, but not carriage of infection or latent tuberculosis. For children for whom x-rays are not indicated, skin tests are performed. The problem is that they often give false positive results. And in order to subsequently save parents and the child from visiting doctors and the need in some cases to still do an X-ray examination, you can perform a blood test - for example, T-SPOT.TB.
Such an analysis can be recommended not only if the skin test result is positive. The second case is when, in principle, it is impossible to make a Mantoux test. It's not just a matter of parents' refusal; there are medical contraindications. The third situation when a blood test is indicated is an examination of people at risk: first of all, medical personnel, people with immunodeficiency conditions (HIV, systemic diseases requiring the use of immunosuppressants, cancer, etc.), those who have been in contact with a patient with tuberculosis . In principle, if a person who does not fall into any of the categories has had, for example, fluorography, but for some reason he is not satisfied with the negative result (let’s say he has warning symptoms), he can also clarify the situation with the help of such a test.
Primary and secondary form
Depending on whether a person fell ill with tuberculosis for the first time or not, primary and secondary tuberculosis are distinguished.
- Primary tuberculosis is an acute form of the disease, which begins to manifest itself after the pathogen enters the blood. Primary tuberculosis is often observed in children under 5 years of age. This happens because children have not yet fully developed immune systems that are unable to cope with mycobacteria. Despite the fact that the disease is severe during this period, it is not dangerous to others. At the beginning of primary tuberculosis, a small granuloma forms in the lungs. This is the primary focus of lung damage, which, if the outcome is favorable, can heal on its own. Thus, the patient may not even suspect that he actually had tuberculosis, attributing his health to a cold. However, after the next X-ray, it turns out that he has a healed granuloma in his lungs. The development of a bad scenario involves the enlargement of the granuloma with the formation of a cavity in which tuberculosis bacilli accumulate. Mycobacteria enter the bloodstream, where they spread throughout the body.
- Secondary tuberculosis. This form of the disease occurs when a person has already had tuberculosis once, but he became infected with another type of mycobacteria. Or secondary tuberculosis can occur in the form of an exacerbation of remission of the disease. Secondary tuberculosis is much more severe than primary tuberculosis. New lesions form in the lungs. In some cases, they are located very close to each other, which merge to form large cavities. Approximately 30% of patients with secondary tuberculosis die within 2-3 months after the onset of the disease.
There are also pulmonary and non-pulmonary forms of tuberculosis. Phases of the tuberculosis process: infiltration, decay, contamination; resorption, compaction, scarring, calcification. More than 90% of cases occur in the pulmonary form of tuberculosis. Damage to the genitourinary organs, brain, bones, intestines and other organs is also possible.
How to treat tuberculosis?
In adults, treatment of tuberculosis is complex and lengthy; depending on the type and severity of the disease, it lasts up to two years and includes the following measures:
- Chemotherapy;
- Maintenance drug therapy;
- Surgical interventions (if necessary);
- Rehabilitation in sanatorium-resort institutions.
In modern phthisiatric practice, anti-tuberculosis therapy is used with the participation of several types of antibiotics.
There are currently three treatment regimens available:
- Three-component;
- Quadruple;
- Five-component.
Treatment of tuberculosis consists of two main phases:
- Intense;
- Prolonged.
The goal of the first, intensive phase is to stop the inflammatory process, prevent further tissue destruction, resorption of infiltrate and exudate, and stop the removal of tuberculous mycobacteria from the body into the environment. That is, doctors are trying to make a person stop being contagious. This takes, on average, two to six months.
Prolonged treatment of tuberculosis is aimed at complete healing of foci of inflammation, scarring of damaged tissue and restoration of strong immunity in the patient. Depending on the nature and severity of the disease, therapy can last up to two years, and in the case of multidrug-resistant tuberculosis - up to three to four years, until X-ray examination proves complete attenuation of the disease.
Additional therapy for tuberculosis includes:
- B vitamins, glutamic acid and ATP are needed to prevent peripheral neuropathy and other undesirable effects from the central nervous system;
- Immunostimulants (galavit, xymedon, glutoxim) help the body fight mycobacterium tuberculosis;
- Methyluracil, aloe vera, glunate, FiBS are prescribed during the treatment of tuberculosis to accelerate the processes of cellular regeneration;
- Sorbents (acetylcysteine and rheosorbilact) are prescribed during chemotherapy withdrawal in case of extremely severe side effects. After a short period of rest, treatment still has to be resumed;
- Hepatoprotectors are necessary to protect the liver from the destructive effects of antibiotics; they are prescribed with constant monitoring of the level of bilirubin in the blood;
- Glucocorticoids are a last resort because they have a strong immunosuppressive effect. But sometimes they are still prescribed for a short period of time in order to suppress the too violent manifestations of the inflammatory process in extensive and severe tuberculosis.
In advanced cases, surgical treatment of tuberculosis may be required.
Symptoms of tuberculosis
In adults, pulmonary tuberculosis can be asymptomatic for a long time or with a small number of symptoms and discovered by chance during fluorography or on a chest x-ray. The fact of contamination of the body with tuberculous mycobacteria and the formation of specific immunological hyperreactivity can also be detected by performing tuberculin tests.
In cases where tuberculosis manifests itself clinically, usually the very first signs are nonspecific manifestations of intoxication: weakness, pallor, increased fatigue, lethargy, apathy, low-grade fever (about 37 ° C, rarely above 38 °), sweating, especially disturbing the patient at night, weight loss Often generalized or limited to any group of lymph nodes, lymphadenopathy is detected - an increase in the size of the lymph nodes. Sometimes it is possible to identify a specific lesion of the lymph nodes - “cold” inflammation.
Further, as the disease develops, more or less obvious symptoms from the affected organ appear. With pulmonary tuberculosis, this is a cough, sputum discharge, wheezing in the lungs, runny nose, sometimes difficulty breathing or chest pain (usually indicating the addition of tuberculous pleurisy), hemoptysis. With intestinal tuberculosis - certain intestinal dysfunctions, constipation, diarrhea, blood in the stool, etc. As a rule (but not always), damage to the lungs is primary, and other organs are affected secondarily through hematogenous seeding.
However, there are cases of development of tuberculosis of internal organs or tuberculous meningitis without any current clinical or radiological signs of lung damage and without a history of such damage.
Tuberculosis: diagnosis, prevention, treatment
Tuberculosis: diagnosis, prevention, treatment

Content
Tuberculosis is an infectious disease of bacterial etiology. The disease has not only a medical, but also a social aspect: the most sensitive to the causative agent of tuberculosis are people with a low level of immunity, an unbalanced diet, living in conditions of non-compliance with sanitary and hygienic standards, and poor social and living conditions. The development of the disease is influenced by the level of a person’s quality of life. However, the risk group for tuberculosis consists of all segments of the population, regardless of age and gender. The high frequency of deaths (up to 3 million people per year) and the prevalence of the disease are due not only to social reasons, but also to the long period of latent course of the disease, when symptoms of tuberculosis do not appear. This time is the most favorable for therapy, and to determine the likelihood of infection, an assessment of the body’s reaction to the Mantoux test is used.
Causes of the disease and routes of infection
The disease develops after infection of the human body with the tuberculosis bacterium Mycobacterium or Koch's bacillus. This microorganism is resistant to environmental influences, high temperatures, and remains viable for a long time at low temperatures.
Koch's bacillus is not considered a highly contagious infectious agent, although a carrier of infection with an open form of the disease spreads bacteria into the environment, the likelihood of getting sick after contact with the pathogen and its penetration into the body in a healthy person is extremely low. A tuberculosis patient (tuberculosis patient) in most cases does not require hospital treatment in an inactive form of the disease and is not limited in movement or social activity. With constant household contact, in families where there is a person with tuberculosis, it is recommended to pay attention not only to his health, but also to maintaining hygiene, measures to strengthen the immunity of other family members and regular checks of the body’s reaction to the Mantoux test to identify possible infection at the earliest stages .
The main route of infection is the entry of Koch's bacillus into the respiratory system by airborne droplets. Household (contact) and transplacental methods of transmission of infection are less frequently recorded. The bacterium enters the body through the respiratory tract, then migrates to the mucous membrane of the bronchi and alveoli and spreads throughout the body through the bloodstream. For the human body, Koch's bacillus is a foreign microorganism. Normally, when it appears and multiplies in the body, immune cells attack the causative agent of the disease, preventing the stage of active reproduction. The development of the disease is likely in two cases: if the immune system is suppressed, there are disturbances in the production of antibodies, conditions of immunodeficiency, the body’s defenses are weakened by other diseases, or are not sufficiently formed due to age or social conditions; or if contact with the pathogen is long-term, constant, the bacilli carrier is at the stage of an open form of the disease and does not receive the necessary treatment (in case of undiagnosed tuberculosis in a family member, when kept in closed institutions, etc.).
Among the factors that reduce specific immunity and contribute to the development of the disease upon contact with an infectious agent are the following:
- smoking as a factor in the development of diseases of the bronchopulmonary system, weakening local immunity;
- excessive intake of alcoholic beverages;
- all types of drug addictions;
- predisposition to diseases of the respiratory system due to the presence of structural abnormalities, a history of frequent diseases, the presence of chronic inflammatory processes in the respiratory organs;
- chronic diseases and foci of inflammation in other organs and tissues;
- diabetes mellitus, endocrine diseases;
- unbalanced diet, lack of vitamins and nutrients;
- neurotic disorders, depressive states, low stress tolerance;
- pregnancy period;
- unfavorable social and living conditions.
Development of tuberculosis: signs and symptoms of various stages of the disease

As a rule, the increase in manifestations of tuberculosis occurs gradually. For a fairly long period, the pathogen does not manifest itself in the body, spreading and multiplying mostly in the tissues of the lungs. At the onset of tuberculosis there are no symptoms. There is a primary stage, at which pathogenic organisms predominantly multiply and are not accompanied by clinical manifestations. After the primary stage, the latent or hidden stage of the disease occurs, at which the following symptoms may be observed:
- general deterioration of health;
- fatigue, loss of strength, irritability;
- unmotivated weight loss;
- excessive sweating at night.
Cough and elevated body temperature are not typical for the first stages of the disease; these symptoms are noted at the stage of extensive damage to the lung tissue. If the picture of the first stages of the development of the disease is blurred, diagnosis is only possible using tuberculin tests (Diaskin test, reaction to the Mantoux test, etc.) or using a blood test for PCR. The next stage is characterized by a latent stage, a “closed” form of tuberculosis, in which the pathogen is not released into the environment and, with its moderate reproduction and resistance of the body, no significant harm to health is observed. The latent form is dangerous due to the possibility of transition to the stage of an active disease, which is not only dangerous for others, but also has an extremely negative effect on the body. The active stage passes into the secondary stage, the pathogenic microorganism reaches the stage of mass reproduction and spreads to other organs of the body. Severe lesions and diseases occur, leading to death.

Active stage of tuberculosis: symptoms and manifestations
Symptoms of tuberculosis in the acute period of the disease:
- prolonged (more than three weeks) wet cough with sputum production;
- presence of blood inclusions in sputum;
- hyperthermia in the low-grade range;
- unmotivated weight loss;
- increased fatigue, general deterioration in health, weakness, irritability, decreased appetite, deterioration in performance and other signs of intoxication of the body.
The cough is wet, pronounced, attacks are frequent, with a characteristic increase in the morning. Often at this stage of the disease, smokers mistake this symptom for manifestations of “smoker’s cough,” a sign of chronic bronchitis in nicotine-dependent patients. With more aggressive rates of disease development, the clinical picture may be supplemented by the following symptoms:
- hyperthermia in the febrile range (body temperature 38-39°C);
- pain in the shoulders, sternum;
- pain when coughing;
- dry cough, hard breathing.
The symptoms of the tuberculosis inflammatory process are similar to the clinical pictures of other respiratory diseases of viral and bacterial etiology. Differentiation of diagnoses is carried out only by a specialist.

Symptoms of extrapulmonary forms of the disease
Koch's bacillus can affect not only lung tissue, but also multiply and cause inflammatory processes in other organs. With such localization they speak of an extrapulmonary type of disease. A nonspecific type of tuberculosis damage to internal organs and systems is diagnosed, as a rule, by excluding other diseases and pathologies. The clinical picture depends on the severity of the process and the location of the organ or tissue affected by the bacterium.
- When the inflammatory process is localized in the brain, the disease manifests itself in an increase in body temperature, disturbances in the functioning of the nervous system, sleep patterns, increased irritability, neurotic reactions, and enlargement of the neck and neck muscles. Characterized by pain in the back when straightening the legs, tilting the head towards the chest. The disease progresses slowly, and those at risk include preschool children, patients with diabetes, and HIV-infected people.
- Tuberculous damage to the organs of the digestive system is expressed in periodic defecation disorders, a feeling of bloating, pain in the intestinal area, signs of hemorrhagic bleeding (blood in the stool), and an increase in body temperature up to 40°C.
- Tuberculosis damage to bone and joint tissue is manifested by pain in the affected areas and limited joint mobility. Due to the similarity of symptoms with other diseases of the musculoskeletal system, it is difficult to diagnose.
- Damage to the genitourinary system by tuberculosis bacteria is usually detected in the kidneys and/or pelvic organs. The clinical picture consists of painful attacks in the lower back, body hyperthermia, frequent, painful, unproductive urge to urinate, and the inclusion of blood in the urine.
- Tuberculous lesions of the skin are expressed in the form of rashes widespread throughout the skin, merging and forming nodular formations that are dense to the touch.
Other symptoms are possible when various organs are affected. A pathogenic organism, penetrating the bloodstream, can spread throughout the body and target almost any organ, tissue or system. In this case, clinical signs of the disease are difficult to differentiate from similar inflammatory processes of a different etiology. The prognosis for treatment of extrapulmonary forms depends on the time of diagnosis, the localization of the pathological process, its stage, the degree of organ damage, and the general health of the patient.
Diagnostic techniques

The diagnosis is established on the basis of tests to determine the presence of the pathogen in the body. Diagnostic measures begin with collecting anamnesis and analyzing the patient’s complaints, studying the medical history. To confirm or refute the diagnosis, a number of examinations are carried out:
- analysis for the Mantoux reaction or Pirquet test, the most common test to determine the presence of infection in the body. Intradermal or cutaneous application of tuberculin and assessment of the level of tension of the body's specific immunity. The tuberculin test allows you to assess probable contact with Koch's bacillus, but does not mean confirmation of the disease. This diagnostic method, however, has been criticized by phthisiatricians and other specialists, as it may indicate contact with other types of microbacteria. Also, tuberculin diagnostics using the test method can lead to incorrect results after BCG vaccination. The Mantoux test is also used before primary vaccination to predict possible allergic reactions to the main component of the vaccine;
- The Diaskin test also refers to skin tests, complementing tuberculin diagnostics using the Mantoux reaction method. Being a more specific test, it detects a reaction only to mycobacterium tuberculosis;
- Quantiferon test or ELISA is an enzyme-linked immunosorbent diagnostic test recommended for patients with an allergy to tuberculin, as well as when it is necessary to differentiate a false-positive reaction of the body to the Mantoux test and the Diaskin test after BCG vaccination. The study is carried out on biological material (blood), has no contraindications and is considered the most reliable test (less than 2% of erroneous results, compared to 30% with Mantoux tests). Recommended for identifying latent and extrapulmonary forms of the disease;
- Smear microscopy is carried out as a search for a pathogenic organism in sputum secreted during coughing. If tuberculous mycobacteria are detected in a smear, the method is supplemented by bacteriological inoculation of the sample in a nutrient medium;
- PCR, the polymerase chain reaction method, is the most accurate research method existing today, allowing you to determine the presence of mycobacterial DNA in various biological fluids;
- histological analysis of tissues removed by biopsy is prescribed in situations where it is impossible to confirm the diagnosis by analysis of biological fluids, in particular, in cases of indolent tuberculous lesions of bone tissue.
Using radiography and fluorography, the presence of foci of inflammation in the lung tissues is detected.
Treatment of the disease

The prognosis for recovery for this disease is made based on the stage of the disease, the affected area, and the general health of the patient. Diagnosis in the early stages allows you to prescribe an effective course of therapy that promotes complete healing of the patient. Treatment is long-term, complex, based on the use of antibacterial drugs, anti-tuberculosis drugs, immunomodulators, immunostimulants, probiotics and vitamin therapy. A mandatory part of the course of treatment is dietary nutrition and physical therapy. Treatment of a patient in the active stage is carried out in a tuberculosis clinic to reduce the likelihood of infection of others. The length of stay depends on the type and stage of development of the process and can range from several months to a year or more. Self-cessation of treatment most often leads to relapse or progression of the disease, the development of severe complications, and death.
Preventive measures

The development of the disease depends on the level of immunity, so the main prevention is maintaining a healthy lifestyle. Vaccination
children, regular samples and tests that allow detection of the disease in the early stages, when the prognosis for treatment is most favorable, also play a significant role in the prevention of the disease.