This study allows you to determine the condition of the testicles, epididymis, and spermatic cords. Using ultrasound of the scrotum, deviations in the tissue structure, inflammatory foci, hernias and neoplasms are detected.
PRIMARY CONSULTATION WITH A UROLOGIST—RUB 1,000. ACCEPTANCE BASED ON ANALYSIS RESULTS – 500 rubles. Ultrasound of the kidneys - 1000 rubles. CLICK TO BOOK AN ULTRASOUND, TEST OR DOCTOR CONSULTATION
Let's try to figure out what an ultrasound procedure for men is, in what cases it is worth resorting to this diagnostic method, and what are its advantages or disadvantages over other research methods. You will also learn how often you should resort to the procedure, whether it is worth preparing for it, and what diseases can be detected.
What is scrotal ultrasound and why is it prescribed?
Ultrasound examination is one of the methods for studying the structure of tissues of internal organs, which in a healthy and pathological state differently reflect the wave radiation directed at them and, accordingly, give a different picture that is displayed on the monitor of an ultrasound device.
Ultrasound has no contraindications. During the study, there is no radiation or mechanical impact on the organs. It can be carried out as many times as needed for high-quality diagnostics. Since ultrasound radiation does not harm health, ultrasound is performed not only on adult men, but also on children.
Ultrasound examination is prescribed in the following cases:
- undescended testicle;
- closed injuries;
- an increase in the volume of the scrotal organs;
- infertility of unknown origin;
- pain in the scrotum, including during sexual intercourse;
- change in the appearance of the scrotum;
- inguinal hernia.
Ultrasound of the prostate
As with the scrotum, an ultrasound examination of the prostate allows one to assess its condition, identify neoplasms, their size and nature.
Prostate ultrasound is required for all men over 40 years of age due to the high prevalence of prostate cancer.
For what symptoms and complaints does a urologist prescribe an ultrasound of the prostate gland?
- problems with urination (retention, pain, blood)
- lumps and nodules around the rectum
- low sperm count in spermogram results
- some abnormalities in blood and urine test results
Andrologist consultation
Menshchikov Konstantin Anatolyevich Andrologist, urologist Curator of the spermatology laboratory
Initial consultation
4000 rubles
Repeated consultation
2000 rubles
+7 495 199-7554
+ MAKE AN APPOINTMENT
How the research is carried out

During an ultrasound scan of the scrotum, the patient is placed on his back or side, with the penis pulled up and to the side to provide access to the scrotum. It is recommended to place a rolled towel or bolster underneath to provide access to different parts. The sensor is moved in a certain way to examine the condition of the tissues in the longitudinal, transverse and oblique directions. Usually, during an ultrasound of the testicles in men, the contours of the testicles and appendages are also observed. To assess blood flow and tissue condition, it is enough to examine a cross section of the testicle. In most cases, during an ultrasound of the scrotal organs, both testicles are examined in order to have a comparative picture before your eyes.
Preparation
Features of preparation for the procedure depend on the research method. Preparation for transabdominal ultrasound:
- 2-3 days before the test, exclude from the diet foods that cause flatulence (fresh vegetables and fruits, beans, carbonated drinks, grain bread, yeast products, dairy products, etc.);
- The last meal is 5-6 hours before the ultrasound;
- 2 hours before the procedure, drink 1.5 liters of still water, and then refrain from urinating. If you can't stand it anymore, you can urinate a little, but then drink an extra glass of water.
- It is also possible to fill the bladder through a catheter if a man cannot drink that amount of liquid on his own.
Preparation for transrectal ultrasound does not require tight filling of the bladder, but has an additional mandatory requirement - a free intestine. To do this, you can use a cleansing enema or laxatives purchased at the pharmacy. Don't buy pills with senna!
The procedure should be carried out 1 hour before the examination. If a biopsy material of the prostate gland is supposed to be taken, then the man must start taking antibiotics 1 day in advance (as prescribed by the doctor).
What is vascular ultrasound?
In acute conditions, there is a need to study blood flow in the scrotal organs. For this purpose, ultrasound with Doppler ultrasound is used. A special sensor allows you to clearly see the direction of blood flow and its intensity. This study is most relevant for suspected obstruction of the vas deferens. A vascular pattern can be observed on the monitor screen. Identification of areas of increased blood supply to tissues or, conversely, areas that do not receive sufficient nutrition, helps to diagnose neoplasms and inflammatory processes even at an early stage.
Doppler ultrasound is a very effective diagnostic method for erectile dysfunction. The study allows us to exclude the vascular nature of the condition. To learn how to prepare for a scrotal Doppler ultrasound, consult your doctor.
Indications and contraindications
Doctors refer you for an ultrasound of the scrotum: a surgeon, urologist or andrologist. The reason for such a diagnosis may be:
Sonography should be used in the following cases:
- For preventive purposes, to clarify the diagnosis, after surgery for control;
- Pain or swelling in the scrotum and groin area;
- To scan the lymph nodes, which may indicate diseases of the reproductive system.
- In adolescence with early development or lagging behind;
- If you suspect dilated veins (varicocele), orchitis, orchiepididymitis, epididymitis;
- In case of infertility, unclear spermogram results;
- For various injuries, foreign objects, changes in the size of the scrotum, to study seals;
- When hematomas and inflammation of the scrotum appear, to search for neoplasms, to monitor tumors, cysts and other formations;
- In case of an inguinal hernia, in the absence of two or one testicle in the patient, to determine the reason for the failure of the testicles to descend;
- With partial or complete dysfunction of the reproductive system (impotence), pain during sexual intercourse;
- With poor functioning of the endocrine system.
There are no contraindications to ultrasound diagnostics of the scrotal organs; the examination can be carried out an unlimited number of times. Ultrasound is not an x-ray, so men’s fears for their “dignity” are groundless.
Preparation for the procedure
The study is carried out at any time of the day, regardless of food intake and bladder emptying. Simply wash the area with soap and warm (not hot) water. It is important to prepare yourself mentally—there is nothing scary, much less shameful, about this examination. When conducting research on children or adolescents, it is necessary to explain to them the essence and importance of the procedure.
Decoding the research results

A healthy testicle is characterized by a dense, homogeneous, fine-grained structure. On the outside there is a protein shell in the form of a thin white stripe. If a dark stripe is visible between the protein membranes, a hydrocele is diagnosed. When fluid spills into the inguinal canal, they speak of hydrocele of the testicles. Excess fluid may indicate a hematoma. Testicular cysts are observed as round black spots with clear contours. Epididymitis is indicated by an increased testicular size and a loose, heterogeneous structure. In acute orchitis, there is a cellular structure and an uneven outer contour of the testicle. Varicocele looks like a tense cord with a cellular heterogeneous structure.
The cause of pain may be calcifications, which are small dense areas that usually do not pose a danger, but if there are a large number of them, it is recommended to undergo regular examination. A malignant neoplasm is recognized as an irregularly shaped spot with a heterogeneous structure. With the help of Doppler ultrasound, increased blood flow can be detected in this place.
A transcript of the research results is issued in the form of a medical report.
Ultrasound diagnosis of diseases of the scrotum
The appearance in the clinic of new generation ultrasound devices equipped with high-frequency sensors, the development of new methodological techniques have made it possible to visualize the anatomical structures of the scrotum, which was considered unrealistic 15-20 years ago. However, today, practical doctors in ultrasound diagnostic departments (offices) are not sufficiently informed about the issues of ultrasound diagnostics and differential diagnosis of diseases of the scrotal organs, as evidenced, among other things, by the mail of our magazine. In this article we tried to fill this gap.
The scrotum is a skin-muscular formation (Fig. 1)*, divided into two halves, each of which contains a testicle, epididymis, and scrotal section of the spermatic cord. The wall of the scrotum consists of 7 layers, which are also called testicular membranes. This is skin; the fleshy membrane forming the median septum; external spermatic fascia; fascia of the levator testis muscle; muscle that lifts the testicle; internal spermatic fascia and tunica vaginalis of the testicle, consisting of parietal and visceral layers.
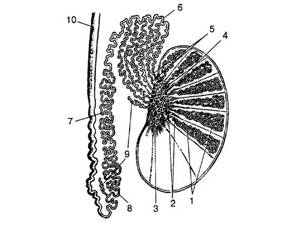
Rice. 1.
Schematic representation of the normal anatomy of the scrotal organs. 1 - convoluted tubules; 2 - straight tubules; 3 — galley net; 4 - maxillary body; 5 - efferent tubules; 6 - head of the appendage; 7 - body of the appendage; 8 - tail appendage; 9 — deviating grooves; 10 - vas deferens.
The testicle is a paired glandular organ of an ellipsoidal shape, somewhat flattened laterally. Its length on average is 4.2-5 cm, width - 3-3.5 cm, thickness - 2-2.5 cm. In the testicle, there are lateral and medial surfaces, posterior and anterior edges, upper and lower poles. The testicle is suspended on the spermatic cord (the left one is lower than the right one) in such a way that its upper end is inclined forward, and its lateral surface is slightly posterior. The spermatic cord is attached posteriorly and superiorly. In the projection of the posteroinferior edge there is a scrotal ligament, which fixes the testicle along with the tail of the appendage to the scrotum. The testicle is covered with a fibrous tunica albuginea, forming a wedge-shaped thickening along the posterior surface - the mediastinum of the testicle. From the latter, fibrous septa fan out, connecting to the inner surface of the tunica albuginea and dividing the parenchyma into lobules. Each lobule contains 2-3 seminiferous tubules. The seminiferous tubules contain the seminiferous elements from which sperm develop. The epididymis is located vertically along the posterolateral portion of the testicle. There are an upper thickened part (head), a middle part (body) and a lower, somewhat expanded part (tail). The epididymis serves as a reservoir for the accumulation of sperm. In the area of the upper pole of the testicle, head and tail of the epididymis, various rudimentary formations are found: testicular appendage, epididymal appendage, deviating ducts.
The organs of the scrotum are supplied with blood by the following paired vessels: the testicular artery, the artery of the vas deferens, the cremasteric artery, the anterior and posterior scrotal arteries, and the perineal artery. The testicular artery is a branch of the abdominal aorta, and the right one may be a branch of the right renal artery. Other arteries are branches of the internal and external iliac arteries. The listed vessels widely anastomose with each other, providing good blood supply to the scrotum. Venous outflow is carried out by veins of two types: veins extending from deep-lying areas of the testicle, and veins draining the superficial zones of the organ. Both types of veins, merging, form a pampiniform plexus outside the testicle, forming the testicular vein, which flows into the inferior vena cava on the right and into the left renal vein on the left. The vein of the vas deferens and the vein of the levator testis muscle originate from the venous plexuses of the same name. All three plexuses are united by communicating veins.
Ultrasound examination uses high-frequency (7.5 MHz or more) convex and linear sensors. During echography, the patient lies on his back and fixes the penis to the anterior wall of the abdomen with his hand. The transducer is installed perpendicular to the area under study, and tomograms are sequentially obtained in the transverse, longitudinal and oblique planes of the right and left halves of the scrotum.
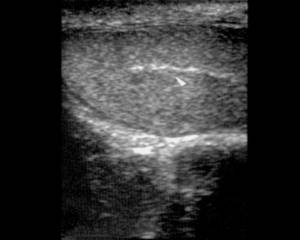
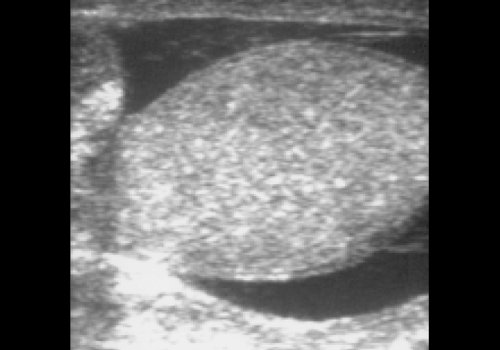
The sizes of both testicles (they may vary slightly), as well as the detected pathological formations, are measured in three mutually perpendicular planes. The unchanged testicle (Fig. 2) has an oval shape, a clear, even contour, the parenchyma is homogeneous, of medium echogenicity. The tunica albuginea and visceral drainage of the tunica vaginalis are visualized as a thin continuous strip of high echogenicity located along the edge of the testicle. The mediastinum (Fig. 3) has the appearance of a hyperechoic thin strip or wedge in the upper parts of the organ. The testicular appendage can be visualized as a protrusion or tubercle with a diameter of 2-3 mm at the upper pole of the testicle. The testicle is surrounded by a small amount of serous fluid, defined as a thin hypoechoic zone 1-3 mm wide. The epididymis (Fig. 4) is located at the upper pole along the posterior surface of the testicle. Its structure is homogeneous and echogenicity is similar to the testicular parenchyma. In the absence of pathological changes in the appendage, only its head is determined, the size of which is 10-15 mm.
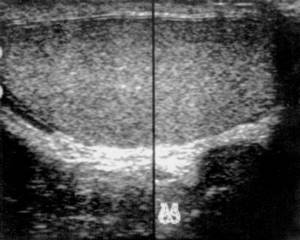
Rice. 2.
Normal testicle.
Rice. 3.
Mediastinum of the testicle.

Rice. 4.
Head of the epididymis.
The spermatic cord and pampiniform venous plexus are located in the form of a cord of cellular structure with many hypoechoic areas with a diameter of 1-2 mm, located above the testicle or along its posterior edge.
Anomalies of testicular development.
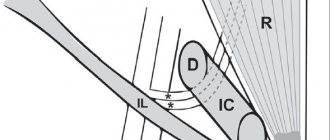
One of the areas of application of echography is to clarify the location of an undescended testicle. An anomaly of location, in which the testicle is located along the normal path of its descent, but does not enter the scrotum, is called cryptorchidism. Most often, the testicle with cryptorchidism is retained in the inguinal canal. With ectopia (extremely rare), the testicle descends normally through the external inguinal ring, but then its reverse movement begins, as a result of which it is located ectopically. Ultrasound examination, as a rule, is effective only for inguinal retention of the testicle.
If one or both testicles are absent in the scrotal cavity, it is necessary to conduct a study in the projection of the inguinal canals. To do this, the transducer is moved from the area of the external inguinal ring along the inguinal fold, capturing the suprapubic region and the region of the femoral triangle. An undescended testicle is often reduced in volume, has an unclear contour and a heterogeneous structure. As a rule, with cryptorchidism the epididymis is not differentiated.
Varicose veins of the spermatic cord (varicocele)
. The importance of timely diagnosis of varicocele is explained not only by the prevalence of the disease (from 8 to 20%), but also by the unfavorable effect on spermatogenesis. The etiological factors of suffering include: congenital absence or insufficiency of the testicular vein valves, weakness of the venous walls of the pampiniform plexus, the confluence of the left testicular vein into the left renal vein at a right angle and some other pathological conditions.
Varicose veins have characteristic ultrasound signs: in the projection of the scrotal part of the spermatic cord, the superolateral and posteroinferior parts of the testicle, multiple dilated tubular anechoic structures of a convoluted or nodular shape are determined. The diameter of the veins exceeds 3 mm.
There are three stages of the disease: in the first, varicose veins are detected only when the patient strains or when examining him in a standing position; in the second (Fig. 5a), the varicocele remains in the supine position, and dilated vessels are identified at the level of the upper pole of the testicle and slightly lower. In the third stage (Fig. 5b), varicose veins are visualized below the lower pole of the testicle, and a decrease in its size up to atrophy is noted.
Rice. 5.
Varicocele.
A)
Stage 2 of the disease.

b)
Stage 3 of the disease.
Hydrocele of testicular membranes
. Hydrocele of the testicular membranes (hydrocele) is characterized by the accumulation of serous fluid between the visceral and parietal layers of the testicular tunica vaginalis (Fig. 6). Hydrocele can be either congenital or acquired. The causes of the latter are most often inflammatory diseases of the epididymis and its trauma, congenital - non-closure of the vaginal process of the peritoneum after the descent of the testicle into the scrotum.
Rice. 6.
Hydrocele.
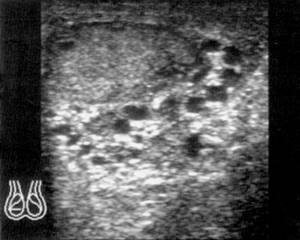
Ultrasound diagnosis of hydrocele is not difficult: a large anechoic zone surrounding the testicle and epididymis is usually visualized. Sometimes the fluid penetrates the inguinal canal, forming an hourglass-shaped hydrocele or multilocular hydrocele (Fig. 7).
Rice. 7.
Multilocular dropsy.
Cysts of the testicle and epididymis (seminal cysts, spermatocele)
. Seminal cysts can develop from embryonic remains, and can also be acquired. Seminal cysts from embryonic remains are usually small in size (rarely more than 2 cm) and contain clear fluid (Fig. 8). Acquired - occur as a result of an inflammatory process or injury, causing obliteration of the duct and the formation of a retention cyst.

Rice. 8.
Epididymal head cyst (size 13.8 x 9.6 mm).
On ultrasound tomograms, seminal cysts are located in the form of round or oval anechoic formations with a smooth, thin, clear contour.
Inflammatory diseases of the epididymis and testicles
. Epididymitis (inflammation of the epididymis) is most often accompanied by orchitis (inflammation of the testicle itself), which is explained by the close anatomical and functional connection of the organs, a well-developed collateral network between their circulatory and lymphatic drainage systems. In most cases, epididymitis and orchitis are infectious in nature.
Echographically, with epididymitis, there is a uniform increase in the appendage, a decrease in its echogenicity, the structure often becomes fine-mesh and heterogeneous (Fig. 9). Often the testicular membranes are involved in the inflammatory process, which is manifested by the presence of free fluid in their cavity. In chronic epididymitis, the appendage is enlarged in volume and has a heterogeneous structure (Fig. 10); cysts may form.

Rice. 9.
Acute epididymitis. CDC.

Rice. 10.
Chronic epididymitis.
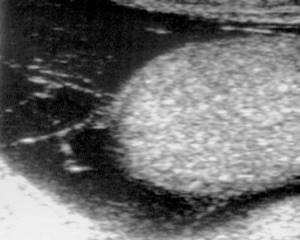
In acute orchitis, the testicle is increased in volume and its echogenicity is reduced. In most cases, the disease is accompanied by effusion into the testicular membranes. The greatest difficulty for differential diagnosis is chronic orchitis. During ultrasound scanning in such a case, the testicle is often enlarged in size (although it may be normal or reduced), has an uneven contour, and the internal structure is heterogeneous (Fig. 11). Frequent development of vascular thrombosis during orchitis leads to the formation of focal changes that must be differentiated from the tumor process.

Rice. eleven.
Chronic orchitis.
Testicular tumors
. Neoplastic testicular lesions are relatively rare (2-3% of all malignant neoplasms in men). More than 90% of cancer cases are germ cell tumors that develop from the seminiferous epithelium. Tumors appear in both homogeneous and mixed forms, somewhat more often on the right; bilateral lesions are observed in 1-2% of patients.
On ultrasound tomograms, the tumor often has an irregular shape, sometimes consists of several merging nodes, and its structure is heterogeneous. The affected testicle is usually enlarged in size, and a reactive effusion is visualized in its membranes. In a patient with a suspected testicular tumor, the retroperitoneal space and regional lymph drainage zones must be examined. The peculiarity of lymphatic drainage is due to the predominant damage to the paracaval lymph nodes in cancer of the right testicle and para-aortic lymph nodes in the left; the lymph nodes located at the level of the renal hilum are initially affected. Metastases in the inguinal lymph nodes appear in advanced cases with significant local spread of the tumor process.
Based on the results of the ultrasound examination, the conclusion should reflect: the size of both testicles (normal, enlarged, reduced); sizes of appendages (their heads); the nature of the contour (smooth, uneven, clear, fuzzy); characteristics of the echogenicity of the parenchyma of the testicles and appendages (normal, decreased, increased); the presence of free liquid in the intershell space. In addition, you should indicate the size and characteristics of pathological formations, if any, and also note the symmetry or asymmetry of the vascular pattern.
* Sirotkin A.K. Topographic anatomy of the genital organs, urethra and perineum / In the book: Operative urology. — M.-L.: State. Publishing house of biological and medical literature, 1934.
Literature
- Demidov V.N., Pytel Yu.A., Amosov A.V. Ultrasound diagnostics in uronephrology. M.: Medicine, 1989. - 112 p.
- Zubarev A.V. Diagnostic ultrasound. M.: Realnoe Vremya, 1999. - pp. 94-103.
- Zubarev A.R., Mitkova M.D., Koryakin M.V., Mitkov V.V. Ultrasound diagnostics of the external genitalia in men. M.: Vidar, 1999. - P. 53-81.
- Lopatkin N. A. Urology. M.: Medicine, 1992. - P.267, P.468-488.
- Mitkov V.V. Clinical guidelines for ultrasound diagnostics. M.: Vidar, 1996. - P.311-321.
- Sinelnikov R.D. Atlas of Human Anatomy, vol.2. M.: Medicine, 1973. - P. 183-186.
- Fenish Hantz. Pocket atlas of human anatomy. 2nd ed. Minsk: Higher School, 1998. - pp. 158-162.

Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
Advantages and disadvantages of scrotal ultrasound
The main advantages of ultrasound diagnostics are:
- absolute painlessness and comfort for the patient;
- high information content of the resulting picture;
- no harm to health;
- There is no need for complex preparation for an ultrasound test of the testicles in men.
The only disadvantage of ultrasound is the inability to distinguish benign from malignant lesions. To exclude the possibility of developing an oncological process, a biopsy of the suspicious area is additionally prescribed.
What pathologies does ultrasound detect in men?
There are a large number of pathologies of the genitourinary system in men. Ultrasound scanning allows us to identify the following abnormalities at an early stage of development:
- infectious and inflammatory pathologies (cystitis, prostatitis, vesiculitis);
- benign and malignant neoplasms (tumors, polyps, cysts, etc.);
- urolithiasis (sand, bladder stones);
- prostate adenoma;
- factors causing male infertility;
- vascular pathologies of the pelvic organs;
- congenital structural anomalies;
- circulatory disorders.
What diseases can be detected during examination?
An ultrasound examination, performed using highly sensitive equipment, will help diagnose minimal changes in the organs being examined. Using this type of diagnosis, the doctor will be able to identify almost any genitourinary disease:
- cystitis;
- vesiculitis;
- urolithiasis;
- adenoma, prostatitis;
- congenital developmental anomalies;
- problems with blood supply to organs;
- benign neoplasms: cysts, polyps;
- pathological processes in the testicles: cysts, epididymitis, hydrocele, varicocele, torsion, abscesses;
- malignant tumors.
Pathological indicators detected on pelvic ultrasound in men
| Pathology | Signs |
| Acute cystitis | loss of small hyperechoic sediment (salt); the wall of the bladder is not changed. |
| Chronic cystitis | the sediment is represented by larger hyperechoic formations (flakes); thickened, uneven bladder wall. |
| Urolithiasis disease | large sharply hyperechoic foci; impaired bladder emptying and an increase in its residual volume. |
| Polyps (tumors) | local formations on the wall of the bladder, protruding into the lumen of the organ. The question of the nature of the formation will be finally resolved by histology. |
| BPH | deformation of the prostate gland; change in its value; focal growth. |
| Acute prostatitis | swelling of the prostate gland; low echogenicity. |
| Prostate abscess | cavity of very low echogenicity. |
| Chronic prostatitis | prostate hardening; foci of high echogenicity in the form of cords; gland deformation; with prolonged inflammation and stagnation of secretions, foci of high density appear. |
| Prostate cancer | deformation of the prostate gland (in the form of a node or diffuse); echogenicity may vary. |
What is included in the examination?
What is included in an ultrasound examination of the pelvic organs in men:
- Prostate. A male endocrine gland that produces specific hormones and secretions that support reproductive health and protects the bladder from pathogenic infections. Problems with the prostate can occur at any age, but most men experience the disease after 40 years of age, when the organ undergoes changes as a result of age-related physiological processes.
- Seminal vesicles. These are specific glands in which seminal fluid is formed.
- Bladder. A hollow organ of the urinary system that is responsible for storing and excreting urine.
- Adjacent tissues, lymph nodes.
To assess the condition of the seminal vesicles and ducts, a transabdominal or transrectal examination is prescribed. These methods will help identify uncharacteristic changes in the organ, pathological neoplasms and compactions.
When examining the bladder, a transabdominal method is used, with which it will be possible to identify structural changes, neoplasms and other pathologies.
When examining the prostate, transrectal ultrasound is used, with which you can assess the volume, size, structure of the gland, as well as timely diagnose any pathological changes.
Contraindications to pelvic ultrasound in men
There are no contraindications for transabdominal ultrasound, except for severe damage to the skin at the examination site (open wound, burn, infection).
Transrectal ultrasound is prohibited if the patient has:
- anal fissures;
- hemorrhoids;
- a tumor in the rectum that narrows the lumen.
Also, the procedure cannot be performed immediately after the x-ray. The patient should notify the doctor if, 2 days before the ultrasound, he underwent an X-ray examination during which a contrast agent was used. This is of great importance, since residues of the substance will be present in the intestines and distort the results of the ultrasound.
Normal indicators
The pelvic ultrasound should be interpreted by a clinician according to the parameters being studied:
- localization of each organ;
- size and shape;
- structure and contours;
- nature of echogenicity.
Normally, the organs being examined should have the correct shape and size, and there should be no formations.

Normal bladder examination results in men are as follows:
| Wall | homogeneous |
| Circuit | round in cross section and oval in sagittal view |
| Wall thickness | 3 – 5 mm |
| Residual cavity volume | 50 ml |
Normally, after urination, a complete absence of urine in the bladder should be recorded, as well as its normal flow from the ureters to the bladder.
Normal prostate parameters
| Form | Oval or close to triangular |
| Upper anterior prostate size | 24 – 41 mm |
| Anteroposterior size of the prostate | 16 – 23 mm |
| Transverse size of the prostate | 27 – 43 mm |
| Prostate volume | 24 – 30 cm3 |
The diameter of the seminal vesicles should be 8-10 mm.
The cause of distorted results may be fecal residues, accumulated gases in the intestines, fat, incorrect position during the examination, or damage to the skin of the abdomen.
Any deviations will indicate the development of a pathological change in the man’s body.
Benefits of the procedure
Among the main advantages of ultrasound diagnostics are the following:
- Non-invasive. The procedure does not require injections, incisions or other tissue damage.
- Painless. During the ultrasound, the patient does not experience any discomfort.
- No ionizing radiation. This allows you to prescribe ultrasound for adults, children, and the elderly.
- Good visualization. Highly sensitive sensors allow you to visualize on the screen the slightest changes in the organ that are not visible during x-ray examination.
- Ability to conduct research in emergency situations. In the event of the development of an acute pathology, the doctor will be able to identify in real time the cause of the disorder and the extent of damage to the diseased organ.
- The results are immediately displayed on the monitor, which allows you to make a preliminary diagnosis at the research stage.
- The procedure does not take much time. An ultrasound of the pelvic organs lasts on average 15 – 30 minutes. If the diagnosis is carried out for the purpose of prevention, then it will take no more than 10 minutes.