General information
Detection of elevated levels of creatine phosphokinase (CPK) is an urgent clinical problem.
This deviation may be a reflection of many pathological processes, which are often based on the following diseases: acute myocardial infarction, acute stroke, dermatomyositis/polymyositis, hypothyroidism, paraneoplastic syndrome. At the same time, the listed conditions do not exhaust the entire list of causes, and this review of the literature will allow us to draw attention to the rarer ones. CPK catalyzes the reaction that provides energy for muscle contractions: creatine phosphate + adenosine diphosphate → creatine + adenosine triphosphate. In human tissues, CPK exists in the form of three different isoforms: MM, MV, BB. M is a subunit from the English muscle - “muscle”, B is a subunit from the English brain - “brain”. The MM isoform is found in skeletal muscles and myocardium, MV is found mainly in the myocardium, EV is found in brain tissue, and in small amounts in any cells of the body [1]. Normally, the content of CPK isoenzymes in blood serum is: CPK-MM - 94-96%, CPK-MB - 4-6%, CPK-BB is absent or found in trace amounts [2].
Due to the intensive growth and participation in this process of muscle and nervous tissues rich in CPK, its activity is higher in childhood than in adults. In women, CPK activity is slightly lower than in men [3], and in the early stages of pregnancy it decreases, and in the later stages it can sharply increase due to the CPK-MB isoenzyme [4]. There are also some racial and constitutional differences in plasma CPK concentrations. Thus, in men and women of the Negroid race, its levels are higher than in Caucasians [5], and in trained athletes, CPK activity is higher than in people not exposed to intense physical activity [4, 6]. The level of CPK and its isoforms can be affected by certain manipulations on the eve of the study: intense physical activity, surgical interventions, injuries, intramuscular injections [7, 8].
The main methods for laboratory determination of CPK isoforms include immunoinhibition, ion exchange chromatography and electrophoresis. Immunoinhibition is a method widely used in all diagnostic laboratories; in some cases it has errors in the form of overestimation of indicators, the reasons for which are systematized in Table 1 [2, 9, 10]. The use of more accurate techniques, such as electrophoresis, will help to avoid unreliable results.
The most common causes of increased CPK levels in plasma
The differential diagnosis of a doctor who has identified elevated CPK values using a reference method is primarily based on the following diseases and conditions: acute myocardial infarction, acute stroke, idiopathic inflammatory myopathies, hypothyroidism, variants of paraneoplastic syndrome [11].
According to the Fourth Universal Definition of Myocardial Infarction
cardiac troponins I and T are the main biomarkers used to detect myocardial damage.
Other biomarkers are less sensitive and specific; measurement of CK-MB is justified only if it is impossible to determine cardiac troponins. A CPK-MB level above the 99th percentile of the upper reference limit may indicate the presence of myocardial infarction [12]. Previously, the determination of CPK-MB was used to diagnose recurrent myocardial infarction, but the latest domestic and foreign recommendations only take into account an increase in the level of cardiac troponin by 20% or more from the initial level [13]. Another emergency condition accompanied by an increase in total CPK due to CPK-MB is acute stroke
[14].
Idiopathic inflammatory myopathies
are a group of rare autoimmune diseases characterized by inflammatory lesions of striated muscles with the development of progressive muscle weakness and including the following subtypes: polymyositis, dermatomyositis, autoimmune necrotizing myopathy and inclusion body myositis. An increase in the level of CPK-MB is included in the diagnostic criteria for these diseases [15].
Clinical symptoms of the most common subtypes of idiopathic inflammatory myopathies [15]:
polymyositis: symmetrical muscle weakness of the proximal limbs, neck, pharyngeal muscles, vocal cord muscles (dysphagia, dysphonia), usually subacute onset;
dermatomyositis: symmetrical muscle weakness of the proximal limbs, neck, pharyngeal muscles, vocal cord muscles in combination with skin changes: paraorbital heliotrope rash, Gottron's erythema / papules on the extensor surfaces of the limbs, less often - soft tissue calcification.
It is important to note that 7–20% of all cases of idiopathic inflammatory myopathies are myositis associated with malignant neoplasms, more often dermatomyositis (23.5%) than polymyositis (3.8%) [15]. There is evidence that statin therapy can serve as a trigger for metabolic myopathies [16].
According to the American Heart Association (2019) scientific statement on statin safety, if the cause of an increase in serum CPK levels is unclear, thyroid-stimulating hormone (TSH) levels should be determined, even if there are no clinical signs of hypothyroidism
[17]. Indeed, in terms of frequency of occurrence in the structure of endocrine pathology, hypothyroidism ranks second; its prevalence increases with age and reaches 12% [18]. Also, with age, the frequency of development of concomitant pathologies increases, especially from the cardiovascular system, which determines the need for statin therapy. In clinical practice, questions often arise about the prescription of statins for established hypothyroidism and the accompanying risk of rhabdomyolysis, depending on the degree of its compensation [19]. One of the common mechanisms for the development of muscle damage in patients with hypothyroidism and in patients taking statins is impaired mitochondrial function and damage to membrane ion channels [18].
In the instructions for original and generic statins, you can find information that rosuvastatin at a dose of 40 mg is contraindicated for use in the presence of hypothyroidism, and the use of atorvastatin and pitavastatin in this category of patients must be used with caution [20]. With hypothyroidism, the catabolism of statins slows down, which can lead to their accumulation and increased side effects. On the other hand, statins can reduce the conversion of thyroxine to triiodothyronine by impairing the synthesis of selenoproteins, exacerbating hypothyroidism regardless of the presence of replacement therapy [21].
It must be emphasized that in the relevant Russian and European recommendations on hypothyroidism [22], as well as on the diagnosis and correction of lipid metabolism disorders [23], hypothyroidism is discussed only from the perspective of the cause of secondary dyslipidemia, and there is no information regarding the management of patients with hypothyroidism taking statins presented. Accordingly, the management of a patient taking statins with hypothyroidism is no different from the management of patients without hypothyroidism. The consensus statement of the European Atherosclerosis Society (2015) on statin-associated muscle symptoms (SAMS) states that if an incidental increase in CPK is detected in the range of up to 4 upper limits of normal (ULN) in patients taking statins and without muscle symptoms, it is necessary to to clarify the function of the thyroid gland, and when CPK escalates in the same range, but with the presence of muscle symptoms, there is no such recommendation [24].
On the contrary, in the study by L.A. Lugovoi et al. (2017) showed that the prevalence of muscle symptoms in the group of patients with compensated hypothyroidism and statin therapy is 2–2.5 times higher than in patients without hypothyroidism taking statins, as well as in patients with thyroid insufficiency who achieved drug euthyroidism, but not taking statins. At the same time, the study authors revealed a significant relationship between muscle pain and the duration of statin use in patients with hypothyroidism on statin therapy. Based on the ROC analysis, patients with hypothyroidism taking statins were suggested to maintain TSH levels below 2.5 mU/L in order to reduce the risk of developing SAMS, which, of course, is not always feasible due to the high incidence of cardiovascular diseases [25 ]. Undoubtedly, this recommendation needs to be studied in randomized controlled trials (RCTs) to determine the effectiveness of preventing the development of SAMS in patients with hypothyroidism.
In clinical situations when the share of CPK-MB in the total concentration of CPK accounts for more than 25%, it is worth thinking about a malignant neoplasm
, since various tumors are capable of producing CPK-MB [26]. S.S. Chang et al. (2015) studied a sample of patients with a CK-MB/total CK ratio >1.0. Of the 846 subjects studied, 339 (40.1%) were diagnosed with malignant neoplasms. The most common were colorectal cancer (CK-MB / total CK - 1.42±0.28, 16.5%, n=56), lung cancer (1.38±0.24, 15.9%, n=54 ) and hepatocellular carcinoma (1.3±0.27, 14.5%, n=49). In addition, the CK-MB/total CK ratio was significantly higher in late-stage malignancies than in early-stage malignancies (1.37±0.26 vs. 1.29±0.31, p=0.014), and significantly higher with liver metastases than with metastases of other locations (1.48±0.30 versus 1.30±0.21, p<0.001) [27].
The above results correlate with the data of the domestic study by T.A. Ruzhentsova et al. (2018), which studied the significance of an increase in CPK-MB and the ratio of CPK-MB / total CPK in various extracardiac pathologies. Thus, among the 47 adult patients studied, 36 (76.6%) were diagnosed with cancer, among them colorectal cancer - in 12 patients (33.3%, CPK-MB - 520±183 U/l, CPK-MB ratio / total CPK - 1.41±0.12), stomach cancer - in 8 (22.2%, 429±199 U/l, 1.0±0.1, p<0.05), breast cancer - in 4 (11.1%, 353±198 U/L, 0.77±0.11, p<0.05). Metastatic lesions were observed in 33 (91.7%) patients, most often - metastases to the liver - in 25 (69.4%), to the lungs - in 9 (25%), to the bones - in 5 (13.9%) [2].
The importance of oncological alertness if the CPK-MB exceeds the total CPK indicator was demonstrated by A. Eidizadeh et al. (2019) using a clinical case as an example. A 75-year-old man with a total CPK activity of 387 U/l (reference interval - 30–200 U/l) and a CPK-MB activity of 669 U/l (≤25 U/l) was diagnosed with metastatic prostate cancer, and isolated from blood serum macrocomplexes type 2 (forms of mitochondrial CPK-MB), explaining the discrepancy between CPK isoforms [28].
Correction
Drug therapy
If the cause of hyperfibrinogenemia was the use of oral contraceptives, in order to avoid the development of thrombosis, it may be necessary to discontinue these drugs if the patient has risk factors (excess weight, smoking, hereditary thrombophilia). In all other cases, with the exception of pregnancy, treatment of the underlying disease is necessary to correct hyperfibrinogenemia. The following types of treatment are used:
- Elimination of infectious pathogen.
For bacterial infections, antibacterial agents are used. In the case of sepsis, 2 broad-spectrum antibiotics are used - penicillins, cephalosporins, fluoroquinolones. For influenza, neuraminidase inhibitors are effective drugs. - Therapy for myocardial infarction.
To relieve a painful attack, the patient is administered narcotic analgesics; to prevent recurrent thrombosis and increase the area of damage to the heart muscle, antiplatelet agents and anticoagulants are prescribed. - Chemotherapy.
To transfer a patient with a malignant oncological disease into remission, he is given courses of chemotherapy with a combination of various cytostatic drugs - alkylating agents, nucleoside analogues, antimetabolites. - Hormonal therapy.
To correct hypothyroidism, synthetic drugs containing thyroid hormones are prescribed. The dose is selected individually, taking into account the patient’s age and the presence of concomitant chronic diseases, especially heart disease. The effectiveness of treatment is monitored by determining the TSH level.
Surgery
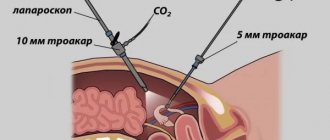
Patients with MI undergo revascularization surgery, i.e. restoration of blood flow in the coronary arteries - percutaneous transluminal balloon angioplasty followed by stenting. A catheter is inserted through the femoral or radial artery and placed into the affected coronary artery. At the site of stenosis, high pressure destroys the atherosclerotic plaque, then a stent is placed in this place, expanding the lumen of the vessel.
For patients with multiple lesions of the coronary arteries in several areas, stenting will be ineffective, so they undergo open surgery - coronary artery bypass grafting. Patients with amyloidosis often require a kidney transplant.
More rare clinical situations accompanied by increased CPK levels
Table 2 lists the main groups of drugs that can cause hypercreatine phosphokinasemia (hyperCPKemia) [20].
![Table 2. Main groups of drugs and their representatives that cause an increase in CPK levels in blood serum [20]](https://ddpskov.ru/wp-content/uploads/tablica-2-osnovnye-gruppy-lekarstvennyh-preparatov-i-ih-predstaviteli-vyzyvayushchie.png)
Let us dwell in more detail on the use of statins, since out of all the variety of lipid-lowering drugs, they are the ones most often prescribed by clinicians for a long period of time. Myalgia and myopathy are the most common side effects of statin therapy, while meta-analyses of RCTs indicate no increase in muscle symptoms among patients on statin therapy, although data from observational studies demonstrate the incidence of SAMS
ranging from 10 to 15% [23]. This discrepancy can be explained by the fact that when conducting clinical trials, there are strict exclusion criteria, thereby patients with multiple risk factors for CAMS are not included in the studies, on the other hand, there is insufficient detection of adverse drug reactions, and they are reported selectively [31].
There is no unified SAMS terminology. Experts from the American College of Cardiology, the American Heart Association, the US National Heart Lung Blood Institute, the US National Lipid Association, and the US Food and Drug Administration give different definitions of myopathy, myalgia, myositis and rhabdomyolysis. We share the point of view of A.I. Dyadyka et al. (2019), who believe that the most acceptable classification is the European Society of Atherosclerosis, which presents muscle symptoms in combination with CPK levels (Table 3) [24, 31].
![Table 3. Definition of statin-associated muscle symptoms [24, 31]](https://ddpskov.ru/wp-content/uploads/tablica-3-opredelenie-statin-associirovannyh-myshechnyh-simptomov-24-31.png)
Some patients with thoracic or lumbar radiculopathy, arthritis, and tendinitis report increased pain when taking statins, possibly because muscle weakness worsens the arthropathy or tendinopathy [32]. Estimating the incidence of statin-associated rhabdomyolysis in the Russian Federation is difficult, which is due to insufficient reporting of these cases; there are only separately presented clinical observations. Among the causes of death in rhabdomyolysis, in 10% of cases, the development of arrhythmias occurs against the background of hyperkalemia or disseminated intravascular coagulation [24]. A rare, but severe and prognostically unfavorable variant of SAMS is statin-associated autoimmune myopathy, which most often develops several months and even years after the start of statin therapy. The appearance of muscle symptoms is associated with the formation of autoantibodies to HMG-CoA reductase, which is confirmed by the detected correlations between the level of autoantibodies, CPK and the severity of muscle symptoms [32].
The Russian recommendations “Diagnostics and correction of lipid metabolism disorders for the purpose of prevention and treatment of atherosclerosis” dated 2020 and the corresponding recommendations of the European Society of Cardiology dated 2021 highlight a group at risk of developing myopathy and elevated levels of CPK while taking statins: elderly patients, patients those receiving concomitant therapy, a large number of drugs, having liver or kidney diseases, athletes [23, 33]. The American Heart Association in 2021 expanded the list of risk factors for hypothyroidism, a history of muscle disease, indicating the influence of factors such as female gender, diabetes mellitus, and Chinese ancestry [17].
Drugs metabolized by cytochrome P450 3A4, which when interacting with statins can lead to myopathy and rhabdomyolysis [33]:
anti-infective drugs: intraconazole, ketoconazole, posaconazole, erythromycin, clarithromycin, HIV protease inhibitors;
calcium antagonists: verapamil, diltiazem, amlodipine;
others: cyclosporine, danazol, amiodarone, ranolazine, fenofibrate; grapefruit, cranberry and pomegranate juice (more than 1 liter per day).
If the initial CPK level is >4 ULN, initiation of statin therapy is not recommended; it is necessary to repeat the study and find out the possible reasons for the increase in CPK [23]. The 2021 recommendations of the European Society of Cardiology developed an algorithm for the management of patients with muscle symptoms during statin therapy, the tactics of which generally correspond to the domestic recommendations of 2020 [33]. These approaches are structured in Figure 1.
![Rice. 1. Algorithm for the management of patients with SAMS during statin therapy [33]](https://ddpskov.ru/wp-content/uploads/ris-1-algoritm-vedeniya-pacientov-so-sams-na-fone-terapii.png)
After statin-associated rhabdomyolysis, non-statin lipid-lowering agents or plasmapheresis can be used to achieve target low-density lipoprotein levels [24].
A possible cause of hyperCPKemia is myocarditis
. There are no necrosis markers specific to it. According to the current Russian recommendations of 2021, determining the content of troponin T and I in the blood serum in cases of suspected acute myocarditis is more appropriate than determining the dynamics of the level of CPK-MB, since cardiac troponins are more sensitive to damage to cardiomyocytes [34].
Another reason for the development of myopathy and increased CPK levels may be hypoparathyroidism with long-term uncompensated severe hypocalcemia. To establish a diagnosis of hypoparathyroidism, it is necessary to register a reduced level of parathyroid hormone and albumin-corrected or ionized blood calcium [35].
In a study by S. Lentini et al. (2006) in a third of the subjects (67 patients) with obstructive sleep apnea syndrome
(OSA), an increase in CPK levels was observed. The mean baseline CK level was significantly higher in patients with severe OSA (191.4 ± 12.9 U/L, n = 89) than in patients with mild to moderate OSA (134.3 ± 7.5 U/L , n=93) and control group (107.1±7.9 U/l, n=19, p<0.01). The use of continuous positive pressure ventilation in patients with OSA led to a significant decrease in CPK levels. The authors suggest that OSA may be the cause of a significant number of cases of unexplained increases in CPK levels, which requires further research in this direction [36]. In a study by A. Sakellaropoulou et al. (2017) established a connection between increased CPK concentrations and chronic intermittent nocturnal hypoxemia in children [37].
Amyotrophic lateral sclerosis
- a steadily progressive neurodegenerative disease of unknown etiology, which is associated with damage to motor neurons of the cerebral cortex, trunk and anterior horns of the spinal cord and is accompanied by the development of paralysis and death due to impairment of respiratory and bulbar functions within 2–5 years after the onset of symptoms [3] . Patients with amyotrophic lateral sclerosis have elevated levels of CPK [3, 38]. N.P. Voloshina et al. (2014) consider the level of CPK activity in the blood serum and cerebrospinal fluid of patients with this pathology as one of the prognostic factors for survival [3].
Progressive muscular dystrophies
are a large group of hereditary neuromuscular diseases. The diseases are characterized by muscle weakness and atrophy, disorders of static and locomotor functions [39]. It is worth noting that clinical cases of a masked course of hereditary myopathies while taking statins have been described, when the diagnosis of SAMS complicates the path to a true diagnosis [40]. Table 4 presents the main muscular dystrophies, accompanied by an increase in CPK levels, that an internist may encounter [41].
![Table 4. Major muscular dystrophies accompanied by increased CPK levels [41]](https://ddpskov.ru/wp-content/uploads/tablica-4-osnovnye-myshechnye-distrofii-soprovozhdayushchiesya-povysheniem-urovnya-kfk-41.png)
Increased CPK levels have high specificity and moderate sensitivity after tonic-clonic seizures
. Post-ictal CK determination can serve as an additional test for differentiating between psychogenic and epileptic generalized tonic-clonic seizures [42].
The list of causes of hyperCKemia continues with acute alcoholic myopathy
. There are three main forms of muscle tissue damage due to ethanol intoxication: acute (1–5% of patients), chronic alcoholic myopathy (60–84%) and alcoholic cardiomyopathy (15–35%) [43]. Acute alcoholic myopathy is characterized by weakness, pain, and swelling of the affected muscles associated with recent alcohol consumption. This form is characterized by an increase in CPK activity [43]. Chronic alcoholic myopathy is characterized by progressive weakness and wasting of the proximal muscle groups of the limbs, difficulty walking, and painful cramps of the leg muscles. This diagnosis is confirmed only by a biopsy of the deltoid or quadriceps femoris muscle, since no increase in CPK levels or changes are observed during electroneuromyography [43].
Positional ischemia syndrome
, often combined with alcohol intoxication, is a type of prolonged compression syndrome, in which the muscles are compressed by the weight of one’s own body. In this case, compression of soft tissues leads to the development of ischemic necrosis, and the entry of myolysis products into the systemic circulation is accompanied by an increase in the level of CPK-MB [44].
Neuroacanthocytosis
- a rare autosomal dominant nosology with a prevalence of 1 to 5 people per 1 million population. The clinical picture of neuroacanthocytosis is characterized by choreiform hyperkinesis, mental and cognitive disorders, polyneuropathy, cardiomyopathy, and the basis of the disease is the presence of altered erythrocytes (acanthocytes) in the peripheral blood. Laboratory diagnosis of neuroacanthocytosis is based on the identification of acanthocytes in a fresh blood smear and the detection of increased CPK activity [45].
Asymptomatic hyperCPKemia
is considered to be established when there is a persistent increase in CPK levels by more than 1.5 times relative to ULN, not accompanied by clinical, neurophysiological manifestations, specific changes in muscle biopsy, and refers to accidentally detected and difficult to diagnose conditions. Often asymptomatic hyperCPKemia is an early manifestation of neuromuscular disease [6, 46]. The only diagnostic guidelines for persistently elevated CPK levels are those of the European Federation of Neurological Societies, published in 2010 and based on level C evidence. Figure 2 shows the diagnostic approach to the presence of persistently elevated CPK levels based on these guidelines [47].
![Rice. 2. Diagnostic tactics in the presence of a persistent increase in CPK levels [47]](https://ddpskov.ru/wp-content/uploads/ris-2-diagnosticheskaya-taktika-pri-nalichii-stojkogo-povysheniya-urovnya-kfk.png)
It should be remembered that the sensitivity of the genetic method of multiplex amplification of ligated probes for suspected Becker muscular dystrophy is 50–99%; therefore, if the result is negative, a muscle biopsy or gene sequencing is recommended [47, 48]. The likelihood of identifying the etiology of asymptomatic hyperCKemia is very low if the following factors are present: elevated CPK levels <3 ULN, an unremarkable family history, an unremarkable neuromuscular examination, and normal electroneuromyography [48]. Recently published results of a 2-year cohort study by A. Rubegni et al. (2019), dedicated to the use of next-generation sequencing in patients with asymptomatic hyperCKemia without an established diagnosis, show the possibility of diagnosing rare genetic defects using this modern technique [49].
Coagulogram. What is this?
You can take a coagulogram test on any day (except Saturday and Sunday) in the laboratory of the National Health Institution “Nodal Hospital at the station. Vyborg. The result is issued on the same day. (office no. 4)

Coagulogram (syn.: hemostasiogram) is a set of blood indicators that characterize its ability to clot. Blood clotting is one of many protective functions that maintain the normal functioning of the body by preventing excessive blood loss.
The coagulogram can be basic or extended. Typically, a baseline study is ordered first. It helps to understand where in the system the deviation from the norm occurred. And if a pathology is detected, a detailed study is carried out, as a result of which not only qualitative changes are determined, but also quantitative ones.
Material for taking a coagulogram: Venous blood Indications for a coagulogram:
- monitoring the state of the hemostasis system;
- routine examination before surgery;
- pregnancy;
- gestosis (complication of a normal pregnancy);
- monitoring of anticoagulation therapy; (for example, taking heparin)
- monitoring of antiplatelet therapy;
- hematological diseases;
- varicose veins Moscow
- atrial fibrillation;
- Coronary heart disease (CHD);
- stroke;
- Pulmonary embolism (PE);
- DIC syndrome; (impaired blood clotting due to massive release of thromboplastic substances from tissues)
- taking medications (oral contraceptives, glucocorticosteroids, anabolic steroids);
- cirrhosis of the liver.
Basic coagulogram parameters:
- Fibrinogen . The most important test of the state of the coagulation system.
- Prothrombin index (PTI), INR (international normalized ratio), PTT (prothrombin time) . Usually one of these tests is performed, based on the equipment available in the laboratory. The most universal test is INR. All of these studies show an extrinsic clotting pathway.
- Activated partial thromboplastin time . In the test you can find the abbreviation APTT.
- Thrombin time.
Additional coagulogram parameters:
- Protein C. An insufficient amount of this parameter leads to thrombosis.
- Antithrombin . Like protein C, it is a factor in the anticoagulation system.
- D-dimer . Formed as a result of the destruction of a blood clot.
- Lupus anticoagulant.
- Plasma tolerance to heparin.
- AVR (Activated Recalcification Time).
- RFMC (soluble fibrin-monomer complexes).
- Plasma recalcification time.
Coagulogram norms (Table):
| Clotting time | ||
|
| |
| Bleeding time | ||
|
| |
| Analysis indicator | Designation | Norm |
| Prothrombin time according to Quick | PV | 11-15 sec |
| INR (International Normalized Ratio) | INR | 0,82-1,18 |
| Activated Partial Thromboplastin Time | APTT | 22.5-35.5 sec |
| Activated Recalcification Time | AVR | 81-127 sec |
| Prothrombin index | PTI | 73-122% |
| Thrombin time | TV | 14-21 sec |
| Soluble fibrin-monomer complexes | RFMK | 0.355-0.479 units |
| Antithrombin III | AT III | 75,8-125,6% |
| D-dimer | 250.10-500.55 ng/ml | |
| Fibrinogen | 2.7-4.013 g | |

Preparing for a coagulogram:
- This analysis is carried out in vitro (in vitro - outside the body). Blood is taken from a vein.
- Blood is donated on an empty stomach. The last meal should be no later than 8-12 hours before the test.
- You cannot drink any drinks (coffee, tea, and especially alcohol). Only clean water is allowed.
- When taking a coagulogram, it is necessary to indicate the medications you are taking - especially those that affect the blood clotting process Moscow
- The emotional state of the patient is very important. You need to try not to be nervous, to be calm and balanced. Muscle overstrain also negatively affects the results of the study.
- It is useful to drink an additional glass of cold water right before taking the test.
- Interpretation of the results is carried out only (!) by a specialist.
Coagulogram during menstruation:
A coagulogram during menstruation is not able to give clear results. The fact is that during this period the blood is diluted and it is not possible to test its clotting abilities. Therefore, to carry out the procedure, it is advisable to wait until the end of the critical days, but not to take the test immediately.
During this period, the body, on the contrary, is interested in removing excess blood from the uterus, so coagulation is somehow impaired. After the critical days, everything returns to full normality, and the woman can easily get tested. Again, it is also not worth carrying out the procedure just before your period; the body is preparing for the withdrawal process and the blood gradually thins out. In this case, the coagulogram will be unreliable and will have to be taken again
Factors influencing the result of a coagulogram?
Factors distorting the result of the analysis:
- violation of the technique of taking and storing material;
- blood sample hemolysis;
- the presence of fat drops in the material;
- ingress of tissue thromboplastin from the patient’s capillary blood;
- the presence of a lupus anticoagulant in the patient’s blood (directly inhibits coagulation factors);
- sharply increased or decreased hematocrit;
- anticoagulants entering the blood sample;
- transfusion of donor blood components in the last month (distorts the fibrinogen indicator, APTT).
Factors that increase INR and PT and reduce PI:
- drinking alcohol, fatty foods;
- medications: antibiotics, anabolic steroids, aspirin (in large doses), acetaminophen, allopurinol, warfarin, vitamin A, heparin, glucagon, diuretics, MAO inhibitors, indomethacin, kanamycin, clofibrate, corticotropin, levothyroxine, mercaptopurine, methyldopa, mefenamic acid, mithramycin, nalidixic acid, neomycin, nortriptyline, propylthiouracil, reserpine, streptomycin, sulfonamides, tamoxifen, tetracyclines, tolbutamide, phenylbutazone, phenytoin, quinidine, quinine, chloral hydrate, chloramphenicol, cholestyramine, cimetidine, ethanol.
Factors that reduce INR and PT and increase PI:
- excess intake of vitamin K from food (found in beef or pork liver, green tea, broccoli, chickpeas, cabbage, turnips, soy, green leafy vegetables);
- diarrhea and vomiting (due to dehydration and increased blood viscosity);
- medications: vikasol (vitamin K analogue), antacids, antihistamines, ascorbic acid, barbiturates, griseofulvin, digitalis, diuretics, colchicine, corticosteroids, caffeine, xanthines, meprobamate, oral contraceptives, rifampicin, theophylline, phenobarbital, chloral hydrate.
Factors that increase APTT:
- antibiotics, asparaginase, aspirin, warfarin, heparin, thrombolytic drugs (streptokinase, urokinase), quinine, cholestyramine, cyclophosphamide, enoxaparin.
Factors that increase fibrinogen content:
- estrogens, oral contraceptives.
Drugs that reduce fibrinogen levels:
- atenolol, valproic acid, lipid-lowering drugs, corticosteroids, progesterone, thrombolytic drugs (streptokinase, urokinase), fluorouracil, estrogens, fibrin degradation products, nicotine.