Indications and contraindications for examination
To obtain high-quality information about the state of a person’s respiratory system, doctors often prescribe an x-ray of the lungs. Indications and symptoms for the use of this diagnosis are:
- suspected pneumonia;
- pleurisy;
- malignant tumors in the lungs;
- tuberculosis, bronchitis and other pulmonary abnormalities;
- prolonged cough;
- chest pain, shortness of breath;
- wheezing in the patient's audible lungs;
- monitoring the progress of therapy for diseases of the pulmonary parenchyma.
In many countries, lung examination is a mandatory preventive procedure at least once every 2 years, and for some categories of employees and citizens, annual examination is strictly mandatory.
Such groups include people working in maternity hospitals, military personnel, carriers of HIV infection, people who have had tuberculosis, as well as those who often come into contact with such patients.
It is also important to undergo an annual X-ray examination of the lungs for those who suffer from bronchial asthma, diabetes mellitus, stomach ulcers and other patients with severe chronic diseases.
Children need to undergo an X-ray examination without indications only from the age of 15; before this age, x-rays can be prescribed by doctors in extreme cases necessary to clarify the picture of the course of the disease. X-ray examination is not recommended for pregnant women.
X-ray and ultrasound syndromes in lung diseases.
Chapter 5. Radiology of the respiratory system.
X-ray syndromes in lung diseases.
The following syndromes are distinguished for lung diseases:
- a) total (subtotal) shading syndrome,
- b) limited shading syndrome,
- c) round shadow syndrome,
- d) cavity formation syndrome,
- e) dissemination syndrome,
- f) syndrome of extensive pathological clearing,
- g) altered root of the lung syndrome.
Syndrome of total (subtotal) shading. This syndrome means shading of the entire pulmonary field or at least two thirds of it. The most important diseases that give a picture of this syndrome: agenesis and aplasia of the lung, subtotal and total pneumonia (lobar, staphylococcal, caseous) pulmonary atelectasis (obstruction of the bronchus by a foreign body or tumor process), massive hydrothorax (effusion pleurisy, hemothorax), diffuse pneumosclerosis, massive pleural adhesions - fibrothorax, (condition after pulmonectomy, armored lung - mantle-like pleurofibrosis, both without and with calcification of the pleura, diaphragmatic hernia or congenital defects of the diaphragm with prolapse of the abdominal organs into the chest cavity.
Having described all the signs of a pathological shadow, it is necessary to highlight the decisive ones for differential diagnosis or diagnosis. These include:
- a) position of the mediastinal organs,
- b) shadow structure.
Processes leading to a decrease in the volume of one half of the chest (atelectasis, pneumosclerosis, pleural adhesions) cause a shift of the mediastinal organs towards shading. Massive accumulation of fluid in the pleural cavity, diaphragmatic hernias, on the contrary, lead to a shift of the mediastinum to the healthy side.
Homogeneous shadowing is characteristic of massive pneumonia (without disintegration), atelectasis, hydrothorax; structural shadowing is characteristic of destructive pneumonia, pneumosclerosis, diaphragmatic hernia, fibrothorax (not always).

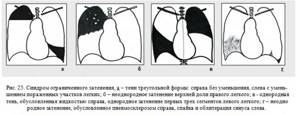
Restricted shading syndrome. This syndrome means shading of no more than two-thirds of the lung field of any shape other than round or oval. The main diseases that give a picture of this syndrome: aspiration of meconium in newborns, simple hypoplasia of a lobe or segment of the lung, pneumonia of various origins (lobar, segmental), primary tuberculosis complex in the phase of infiltration or resorption (bipolarity), infiltrative-pneumonic tuberculosis, limited pneumosclerosis ( OPS) and cirrhosis, segmental and lobar atelectasis, pulmonary tissue infarctions, hydrothorax of various origins, limited pleurofibrosis, diaphragmatic hernia with prolapse of the abdominal organs into the supradiaphragmatic space.
Crucial signs for diagnosis:
- a) correspondence of shading to the structural unit of the lung - lobe, segment (in this case the shadow has a more or less pronounced triangular shape),
- b) shadow structure,
- c) the nature of the shading contours,
- d) the state of the pulmonary pattern and root on the shading side.
The triangular shape of shading with the apex directed towards the root is characteristic of segmental and lobar lesions: segmental and lobar pneumonia, atelectasis, pulmonary infarction, and in this case the diagnostic task is simplified. However, during these processes the shadow can have any other shape. A triangular shadow with an apex directed away from the root is characteristic of effusion, pleural adhesions and moorings (but in this case this sign is not absolute).
The structure of the shadow has the same significance as in total shading syndrome.
Contours are assessed by the nature of their direction (convex, concave) and clarity. Concave contours are observed when the affected area of the lung decreases (atelectasis, infarction, acute renal failure), with small effusions, pleural adhesions. Convex contours are characteristic of inflammatory processes - lobar pneumonia, accumulation of effusion in the pleural cavity. Blurred contours are usually a sign of an active inflammatory process, however, if the inflammation is limited by the pleura, then the contour will be clear. Clarity of contours is also characteristic of atelectasis, infarctions, adhesions, and the organization of effusion.
In inflammatory processes that give rise to limited shading syndrome, an increase in the pulmonary pattern is always observed on the affected side, and the image must be carefully analyzed in search of this symptom. In children, inflammation in one lung very often leads to an increase in the pattern in the other lung. The same applies to the root of the lung. In pneumonia, primary tuberculosis complex, tuberculous infiltrates, exudative pleurisy, the root on the affected side is always expanded (inflammatory hyperemia and inflammatory lymphadenopathy).
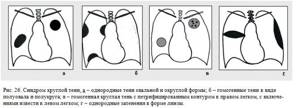
Round shadow syndrome. This syndrome refers to a shadow (shadows) of a round or oval shape, or shaped parts of a circle or parts of an oval, measuring 1.5 cm or more. The most important diseases that give a picture of this syndrome: arteriovenous aneurysms (shunts) - AVA, pulmonary sequestration, bronchogenic cysts, tuberculous infiltrate, tuberculoma, globular and eosinophilic pneumonia, lung abscess in the maturation phase, benign lung tumors, peripheral lung cancer, filled cysts fluid (echinococcal, bronchogenic), metastases, encysted and interlobar pleurisy, pleural tumors, tumors and cysts of the mediastinum protruding into the pulmonary field, rachitic rosary of the ribs.
Crucial signs for diagnosis:
- a) shape (round, oval, part of a circle, part of an oval),
- b) the nature of the contours,
- c) the structure of the shadow in terms of the presence of denser inclusions,
- d) the state of the surrounding lung tissue (additional shadow formations, limited dissemination, track symptom),
- e) the state of the pulmonary pattern and the root of the lung.
The round shape of the shadow is characteristic of formations located in the thickness of the lung parenchyma - a benign tumor, peripheral cancer, inflammatory infiltrates, cysts with liquid contents.. Cysts containing liquid are often oval in shape. Shadows in the form of part of a circle or part of an oval are characteristic of paracostal and paramediastinal encysted pleurisy, for mediastinal neoplasms protruding into the pulmonary field (thymomas, goiter, teratodermoids, lymphomas, neuromas, aortic aneurysms). Interlobar pleurisy usually have the shape of a biconvex or biconcave lens.
The nature of the contours is very important for this syndrome. Smooth and clear contours are characteristic of benign tumors and cysts, large metastatic foci, and encysted pleurisy. A clear but uneven contour is characteristic of peripheral cancer. In inflammatory processes, a fuzzy contour is often observed, which can be even. and uneven character.
The homogeneity of the shadow in this syndrome is characteristic of benign tumors and cysts, metastases, maturing abscesses, and encysted pleurisy. Heterogeneity of the shadow (multi-nodularity) is characteristic of peripheral cancer, and the presence of lime inclusions is characteristic of tuberculomas and teratodermoids.
The presence around or near a single round shadow of smaller shadows (1-10 mm, they are called focal shadows) is characteristic of tuberculoma, and the track symptom (local enhancement of the pulmonary pattern between the round shadow and the root of the lung) is usually observed with tuberculous infiltrates, tuberculoma, peripheral cancer
A general strengthening of the pulmonary pattern with expansion of the root on the side of the round shadow is observed, as with the above-mentioned syndromes, during inflammatory processes. However, the root can also be expanded in case of peripheral cancer and tuberculoma due to regional lymphadenopathy (metastases to bronchopulmonary lymph nodes, caseation of lymph nodes). But if the enlargement of the root during inflammation occurs while maintaining its shape, the enlargement of the root during lymphadenopathy leads to its deformation - it acquires polycyclic, convex contours.
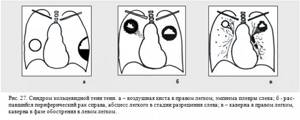
Cavity syndrome (ring-shaped shadow). This syndrome includes shadow formations that look like a round or oval ring. The most common diseases that give a picture of this syndrome: cystic hypoplasia of the lung, congenital diaphragmatic hernia, infiltrative tuberculosis with disintegration, destructive pneumonia (staphylo- and streptococcal, Friedlander's pneumonia), fibrous-cavernous tuberculosis, lung abscess in the resolution phase, disintegrating peripheral cancer, air lung cyst (pneumocele), aspergilloma, bullous emphysema, pleural empyema, encysted pneumothorax, diaphragmatic hernia with prolapse of hollow abdominal organs.
Crucial signs for diagnosis:
- a) thickness of the cavity walls,
- b) the nature of the external and internal contours,
- c) the presence and nature of the content,
- d) the state of the surrounding lung tissue (additional shadow formations, track symptoms),
- e) the nature of the pulmonary pattern and the root of the lung.
Based on the wall thickness, thin-walled cavities are distinguished - 1-2 mm and thick-walled cavities > 2 mm. The first are characteristic of air cysts, stamped and sanitized cavities, bullous emphysema, emptied parasitic cysts, and prolapse of hollow abdominal organs.
Thick-walled cavities are observed with disintegrated peripheral cancer, with an abscess, with tuberculous cavities. Smooth and clear internal and external contours are characteristic of air cysts and bullous emphysema. Uneven and unclear external contours indicate either perifocal inflammation (abscess, cavity, festering cyst), or fibrous changes in the adjacent lung tissue (fibrous-cavernous tuberculosis). Uneven internal contours indicate the disintegration of the pathological process (tumor, parasitic cyst, aspergilloma, sometimes a cavity), smooth and clear internal contours are typical for an abscess, cavity, bronchiectasis.
When talking about the nature of the contents, one must keep in mind the fact that the cavity formation, by its pathoanatomical essence, already contains air, and we are talking about other contents located in the cavity. So, liquid contents - in this case its horizontal level is clearly visible, is characteristic of abscesses in the resolution phase, staphylococcal and streptococcal pneumonia, pleural empyema, diaphragmatic hernias with prolapse of the stomach or intestinal loops. Dense tissue inclusions (sequestra) are characteristic of disintegrating cancer, in some cases of the tuberculosis process, and of fungal infections (aspergillosis).
The condition of the surrounding tissue is usually changed in cavities of tuberculous origin - focal shadows of varying density, a fibrous path to the root; with staphylo- and streptococcal pneumonia - focal shadows of low or medium intensity of different sizes; peripheral cancer - a vascular path to the root of the lung and to the pleura, caused by cancer lymphangitis.
Assessment of the pulmonary pattern and the root of the lung follows the same principle as for round shadow syndrome.
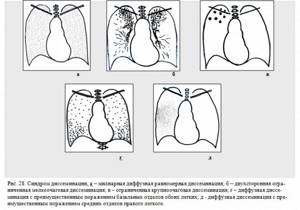
Dissemination syndrome. Dissemination syndrome is the presence of many focal shadows of various shapes, no more than 1.5 cm in size. Based on the affected area, dissemination is classified into unilateral and bilateral, limited (occupying an area of no more than two intercostal spaces) and widespread. Based on the size of the foci, miliary (0 – 2 mm), small focal (3 – 5 mm), medium focal (5 – 8 mm) and large focal (8 – 15 mm) dissemination are distinguished. The most important diseases that give a picture of this syndrome: acute focal pneumonia of various etiologies (pneumococcal, staphylococcal, streptococcal, influenza, measles), miliary tuberculosis, chronic hematogenously disseminated tuberculosis, pneumoconiosis (silicosis, anthracosis, etc.), pulmonary sarcoidosis II- Stage III, metastases of malignant tumors, alveolitis of various origins, fungal infections of the lungs, venous congestion in the lungs, pulmonary hypostasis (accumulation of fluid in the interstitium and alveoli of the basal parts of the lungs), post-tuberculosis focal calcification of the pleura, congenital and acquired hemosiderosis of the lungs.
Crucial signs for diagnosis:
- a) preferential localization,
- b) number of lesions,
- c) intensity and structure,
- d) the nature of the contours,
- e) the condition of the surrounding structures of the lung (roots, pleura, mediastinum).
The localization of lesions may be different for different diseases, but there is still a certain tendency. Unilateral dissemination is more often observed in acute bronchopneumonia and tuberculosis in the phase of lymphogenous and bronchogenic dissemination. Bilateral dissemination is characteristic of acute hematogenously disseminated tuberculosis, staphylo- and streptococcal pneumonia, hemosiderosis, collagenosis, sarcoidosis, pneumoconiosis, and carcinomatosis. The upper parts of the lungs are most often affected by tuberculosis, the upper and middle parts by sarcoidosis, pneumoconiosis, the middle and lower parts by staphylo- and streptococcal pneumonia, the lower parts by metastatic lesions, acute pneumonia, and cardiogenic edema.
A large number of lesions are usually observed in acute miliary tuberculosis, sarcoidosis, pneumoconiosis, and carcinomatosis. Acute pneumonia, fungal infections, and collagen diseases often produce a relatively small number of lesions.
Speaking about the shape of the lesions, it should be noted that most often they have a round shape, while the sizes have little differential significance, but it should be noted that miliary lesions are still characteristic of tuberculosis and venous stagnation with hypostasis.
It is difficult to determine the intensity of foci in dissemination syndrome, since foci with the same density can have different densities, which is explained by their different distances to the film (laws of skialogy). But sometimes there are pockets of lime in the lesions, and this already has great diagnostic significance, since lime is characteristic primarily of tuberculous and post-tuberculous processes, hemosiderosis and some forms of pneumoconiosis.
The nature of the contours can also be distorted by skialological phenomena, but the erasure of the foci is usually characteristic of acute inflammatory processes and disorders of blood and lymph circulation; in other processes, the foci have clearer contours. If the lesions are located against the background of a reticular pattern, they also have unclear contours, and this is already characteristic of alveolitis, lymphogenous metastasis, pneumoconiosis at an early stage of development, interstitial pulmonary edema.
When assessing the condition of surrounding structures, attention is first paid to the roots of the lungs. Enlargement of the roots is characteristic of acute inflammatory processes and stagnation in the pulmonary circulation. Enlargement and deformation are characteristic of chronic forms of tuberculosis, pneumoconiosis, sarcoidosis, malignant lesions of the lymph nodes (metastases, lymphocytic leukemia, etc.). Assessing the condition of the pleura, the presence of effusion is determined (staphylo-streptococcal pneumonia, acute forms of tuberculosis, cardiogenic edema). The presence of adhesions and moorings is typical for pneumoconiosis, post-tuberculosis conditions, collagenosis, and fungal infections. In children, spontaneous pneumothorax, including encysted pneumothorax, is possible in acute interstitial pneumonia, staphylococcal and measles pneumonia.
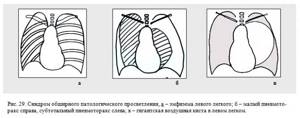
Extensive pathological clearing syndrome. This syndrome means the presence of increased transparency of the pulmonary field from one lobe or more. There are one- and two-sided extensive clearing.
Unilateral clearing is observed in congenital lobar emphysema, giant air cyst, hypoplasia of the pulmonary artery, valve blockage of the bronchus (obstructive emphysema, aberrant pulmonary artery), pneumothorax, and compensatory hyperpneumatosis. Bilateral – for interstitial emphysema of newborns, bronchiolitis, chronic bronchitis, pulmonary emphysema, bronchial asthma.
Crucial signs for diagnosis:
- a) one- or two-sided enlightenment,
- b) the state of the pulmonary pattern,
- c) the state of the diaphragm.
The pulmonary pattern in the zone of pathological clearing is depleted in pulmonary emfzema and in hypoplasia of the pulmonary artery, in ventral bronchoconstriction. Strengthening the pattern in combination with increased transparency is characteristic of compensatory hyperpneumatosis. In chronic bronchitis, the pattern is deformed, and in pneumothorax and a giant air cyst it is absent.
An upward displacement of the diaphragm on the clearing side is characteristic of hypoplasia of the pulmonary artery and its branches; a downward displacement of the diaphragm is characteristic of compensatory hyperpneumatosis and pulmonary emphysema.
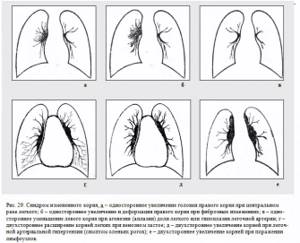
Altered root syndrome. This syndrome refers to unilateral or bilateral changes in the x-ray anatomical characteristics of the root (position, size, shape, structure, intensity, contours). The most important diseases that give a picture of this syndrome: lobar aplasia and agenesis, tuberculous bronchoadenitis, chronic forms of pulmonary tuberculosis, central lung cancer (with peribronchial and exophytic growth patterns), pneumoconiosis, pulmonary sarcoidosis, lymphogranulomatosis, lymphosarcoma, metastatic lesions of bronchopulmonary lymph nodes, venous congestion in lungs, pulmonary arterial hypertension, pulmonary edema.
Crucial signs for diagnosis:
- a) one- or two-sided lesion,
- b) preservation of the anatomical shape of the root,
- c) the nature of the external contour of the root.
- d) the state of the pulmonary pattern on the side of the modified root.
Unilateral damage with a decrease in the root is typical for aplasia and agenesis of individual lobes, with an increase - for central lung cancer, tuberculous bronchoadenitis (although with this pathology there may be bilateral damage), lymosarcoma. Bilateral damage is typical for all the other diseases listed above.
5. Ultrasound syndromes in lung disease.
Syndrome of the presence of free fluid in the pleural cavity. In the pleural cavity, almost anechoic fluid is visualized, in most cases with floating lung tissue. Due to the high sound conductivity of the fluid, from almost any intercostal space corresponding to the level of the fluid or located closer to the costophrenic sinuses, it is possible to visualize the mediastinum and domes of the diaphragm.
When intrapleural adhesions form and fibrin falls out, they are located in the form of thin linear hyperecho structures extending from the contour of the parietal pleura to the contour of the lung.
The minimum volume of fluid detected in the costophrenic sinus is 50 ml, therefore ultrasound examination is especially valuable in identifying local limited fluid accumulations, which is manifested by the symptom of thin anechoic lenses.
Lung tissue hepatization syndrome. In this case, lung tissue is detected that is similar in structure and echogenicity to liver tissue, but with individual point accumulations of gas. Typical for pneumonia and other inflammatory processes, for sclerotic and cirrhotic processes, for diffusely growing tumors that occur with symptoms of depnematization of the lung tissue.
Pulmonary mass syndrome . Visualization of a space-occupying lung formation is possible in the case of decreased pneumatization of the lung tissue along the periphery of the formation (atelectasis, pneumonia, etc.). Against the background of depneumatized lung tissue, a space-occupying formation (solid or liquid) is clearly visualized, similar to those formations detected in any parenchymal organ. In most cases, it is possible to visualize lung abscesses in the form of clearly defined heterogeneous hypoechoic formations with a layer of gas and a pronounced capsule.
As a rule, a nodular tumor focus in the lung cannot be visualized, because the tumor does not lead to a sufficient reduction in pneumatization of the lung tissue for adequate sound transmission.
Mediastinal mass syndrome . When scanning using the jugular or supraclavicular approach, in some cases it is possible to visualize a space-occupying lesion of the upper mediastinum (goiter, thymoma, lymphoma, aortic arch aneurysm). The interpretation of the data obtained does not differ from that when identifying any space-occupying formation.