Arthroscopy is a minimally invasive technique that is an excellent replacement for traditional open shoulder surgery (OS). It allows you to simultaneously diagnose the disease and eliminate existing problems with minimal damage. The procedure does not require any incisions, just a few small punctures, which makes it possible to avoid damage to the connective tissue.
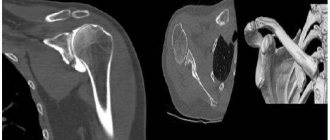
Usually two/three punctures are used. An arthroscope equipped with light sources and a microscopic video camera is inserted into one, which transmits the image to the monitor. This allows you to see all the structures in detail. One or two other punctures are used to introduce microsurgical instruments necessary for the operation.
Inside view of the joint.
This technique ensures high precision of surgery, minimal intervention, absence of postoperative complications and a quick recovery period. The procedure is especially relevant among athletes who need to quickly recover and continue training.
Features of the operation
The patient's journey before surgery begins with a consultation with an anesthesiologist who will offer possible anesthesia options. Most often, regional anesthesia is given to the arm or just the shoulder area. The substance (anesthesia) is injected into the base of the neck or along the sensory nerves related to the shoulder. In some cases, doctors use combined anesthesia with sedatives or mild general anesthetics, as the patient may experience discomfort during surgery. You will also need to undergo blood tests, ECG and fluorography.
It is important to tell your doctor about any medications and/or dietary supplements you are taking. You may need to stop taking some of them for a time before and after surgery.
The intervention is carried out in two positions: a reclining position and a position lying on one’s side. Each position allows for different operations, so the surgeon chooses the most appropriate approach for each patient.
During the surgical process, a fluid is first injected to increase the size of the joint. This allows you to get a higher quality and clearer image. Then punctures are made (from 1 to 3), into one of which an arthroscope is inserted. After the diagnosis is made, micro-instruments are introduced into other accesses to perform the operation. At the end of the operation, the surgeon applies sutures or adhesive strips to seamlessly close the edges of the wounds, securing them with a soft bandage.
The operation usually does not take more than an hour.
Diagnosis and preparation for surgery
To make an appointment for surgical treatment, you need to consult a doctor at our department (contact number 8 812 559 97 83).
You will be examined and examined, high-quality radiography, ECG registration, and blood tests. If you have ready-made examination results (X-ray, MRI, etc.), bring them with you to the consultation. After the examination, you will receive final answers to your questions about the surgical plan and postoperative treatment.
Indications for arthroscopy
Surgeons suggest using this intervention in the following situations:
- For initial diagnosis of pathology or clarification of the diagnosis;
- Severe pain in the shoulder area after surgery. In this case, arthroscopy is aimed at diagnosis and, if necessary, removal of trigger elements;
- Unstable condition shoulder joint (Bankart injury, shoulder dislocation, including primary).
A) In case of anterior dislocation of the joint, the intervention is aimed at restoring the articular labrum (Bankart operation). The method is aimed at restoring the integrity of the articular lip by fixing the torn part to the edge of the articular process of the scapula. B) In case of habitual posterior dislocation, the articular labrum is restored together with suturing of the joint capsule from behind. A study by GW Misamore et WA Facibene showed that after arthroscopy, 13 out of 14 athletes operated on with this method were able to achieve their previous physical condition and results. C) In the case of a combination of posterior Bankart injury, accompanied by a posterior rupture of the scapular glenoid ligament, arthroscopy allows fixing the torn articular labrum to the edge of the glenoid cavity of the scapula, the posterior part of the shoulder capsule to the posterior part of the humeral head. Bioabsorbable anchor fixatives are used as a fixative. - Epicondylitis. Used when conservative treatment is ineffective. The operation consists of separating the muscles from the area of attachment to the condyle of the humerus, then removing chronically inflamed and altered tissue. The muscles are then reattached to the bone.
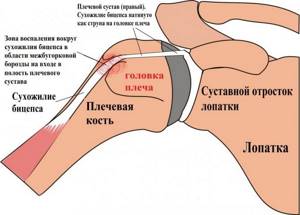
- SLAP syndrome (snapping shoulder syndrome). It is characterized by avulsion of the upper components of the articular labrum of the joint joint associated with the tendon of the long head of the biceps. In the initial stage, arthroscopic debridement of the affected area is recommended. This method makes it possible to remove from the intra-articular space pieces of destroyed cartilage tissue, overgrown fragments of the synovial membrane, and bone protrusions (osteophytes that interfere with the sliding of the articular head and cause additional mechanical damage to the cartilage).
- Capsulitis (“pseudo-frozen shoulder”). The operation is performed only if all conservative methods are ineffective and is aimed at removing the inflamed areas of the joint capsule.
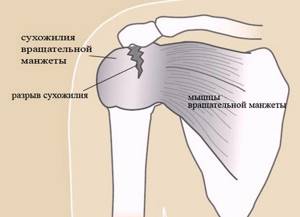
- Rotator cuff injury. During the operation, the torn part of the tendon is stretched to the place of its attachment and then sutured. For this purpose, special materials are used - “anchor clamps”. All necrotic, DDI tissues of the rotator cuff are subject to mandatory removal. Afterwards, the damaged area where damaged cuffs were diagnosed is removed from residual tissue fragments (including soft ones) so that the tendon can be firmly fixed with the help of scar tissue.
- chondromatous bodies in the synovial fluid .
- Overgrowth of bone tissue;
- Osteosynthesis of fractures of the processes of the scapula.
- Bursitis , including removal of the joint capsule of the shoulder joint. In this operation, the surgeon completely removes the inflamed joint capsule.
How to make an appointment for surgery for patients from abroad?
If you would like to undergo shoulder treatment in Germany, you will need to provide us with current MRI images as well as X-ray results. Thus, orthopedic doctors at the Gelenk Clinic will be able to assess the condition of the bones and joints of the shoulder. You can send these documents through our website. After this, within 1-2 business days you will be sent all the necessary information, a preliminary treatment plan, as well as a final cost estimate.
Foreign patients can make an appointment in a short time frame that suits their personal time. We will be happy to assist you with obtaining a visa after the amount of this service indicated in the cost estimate has been credited to our account. If for any reason your visa is denied, this amount will be refunded in full.
For patients from abroad, we try to reduce the time between the preliminary examination and the operation itself. This way you will not need to come to the clinic several times. During both inpatient and outpatient shoulder treatment, you will be able to benefit from the services of the patient management department, whose staff speaks several foreign languages (eg English, Russian, Spanish, Portuguese). We also provide assistance in finding a translator (for example, into Arabic), which is paid for by the patient separately. We will be happy to help you organize a transfer, find a hotel and tell you how to spend your free time in Germany interestingly for you and your family members.
Send request
When surgery won't help
Any procedure has its own situations when it is powerless. It is not recommended to resort to this method of treatment and diagnosis if:
- fibrous or bone ankylosis;
- presence of an infected wound;
- purulent-inflammatory processes in the periarticular tissues;
- liver, kidney, cardiovascular failure;
- deforming osteoarthritis stage III-IV.
In some cases, at the discretion of the specialist, the operation can be performed:
- extensive damage (torn ligaments and joint capsules, loss of joint tightness);
- profuse hemorrhage into the joint cavity.
In cases of ankylosis and arthrosis of the shoulder joint, it is recommended to perform endoprosthetics (replacement of the affected articular surfaces with a prosthesis).
Possible complications
If the operation was performed by an experienced doctor, and the patient followed all his instructions, then the risk of complications is reduced to zero. However, a tiny percentage still exists. What can happen:
- inflammatory processes may begin in the joint capsule;
- damage to nerves and blood vessels;
- damage to bone tissue;
- hematomas and swelling may form and last longer than expected.
If you feel an increase in body temperature or the operated area, you have lost sensitivity in your hand, or if you experience severe pain during exercise therapy or at rest, you should immediately consult a doctor.
What kind of anesthesia
There are several types and tactics of anesthesia based on the characteristics of the injury to the shoulder joint.
- Conduction anesthesia using interscalene blockade. The injected anesthetic reaches the caudal portion of the cervical plexus (C3, C4), the upper and middle sections of the brachial plexus (C5, C6, C7); the drug reaches the lower trunk later and in much lower concentrations, so blockade of the median and ulnar nerves most often does not occur. This type of anesthesia is used for osteosynthesis of the clavicle, elimination of habitual shoulder dislocation (RHD), reduction of shoulder dislocation, and during operations on the upper third of the shoulder.
- Conduction anesthesia through supraclavicular access. The local anesthetic interacts well with all trunks of the brachial plexus, but in 80% of cases it does not reach the ulnar nerve. This anesthesia is indicated for operations on the upper limb and elbow joint. Used for osteosynthesis of the humerus.
- Endotracheal (inhalation) anesthesia. Such anesthesia immerses the patient in a state of deep medicated sleep, close to physiological.
- Combined anesthesia. The most common choice of surgeons. Endotracheal anesthesia is used together with conduction anesthesia. This allows you to potentiate the effectiveness of the methods and increase the analgesic effect after surgery.
Pain and complications of shoulder arthroscopy
If the surgeon complied with all safety standards and the recommendations were followed during the rehabilitation period, complications are usually not observed. However, there are always risks. These include:
- damage to nerves or choroid plexus, clots in the area of surgical access;
- skin diseases (eczema, ulcers, psoriasis);
- inflammatory process in the joint itself;
- cartilage tissue may be damaged, resulting in complete
- fusion of bone tissue (up to the development of the clinical picture of stage IV arthrosis);
- pain of various types in the joint itself and the tissues around it; thrombotic complications.
The most common complication is a postoperative infectious complication. The causative agents are Propionibacterium acnae and Staphylococcus aureus. Such an infection gives a more acute onset, the rapid development of a vivid picture of the infectious lesion: swelling and swelling of the joint, local hyperemia (which, without proper treatment, can become a generalized form), pain and limited mobility of the joint.

Infection.
Pain almost always accompanies the person undergoing surgery in the first days after surgery. During this period, it is important to fix the operated limb as much as possible and use any available drugs to relieve pain - NSAIDs, glucocorticoids and their intra-articular injections, intra-articular injections of sodium hyaluronate (depending on the severity of pain). The duration of this period varies for each patient, however, most often the condition improves by the end of the first week after arthroscopy.
How is the operation performed?
Typically, this type of intervention is performed under general mask or endotracheal anesthesia. Therefore, the question “whether it hurts or not” disappears here by itself, as does the fear of seeing what is happening.
The operated area is treated with an antiseptic and marks are made on the position of the joint and puncture sites for insertion of the arthroscope. Using a puncture needle, the joint capsule is punctured and synovial fluid is removed from it. The synovial fluid is quite thick, as it serves to lubricate the joint, and the arthroscope - the main instrument of this operation - is equipped with a small video camera through which the image is transmitted to a large screen. To ensure good visibility inside the joint, the liquid is replaced with saline solution.
After the examination, the surgeon takes material for further research and, depending on what problem is found inside the joint, decides its fate:
- strengthens the joint capsule;
- removes inflamed areas;
- fixes ligaments;
- strengthens the labrum, etc.
The operation can last from one to three hours. When the procedure is completed, the instruments are removed and the incisions are covered with sutures and a sterile dressing. Using a shoulder brace, the joint is fixed in the desired position.
Regarding stitches, it’s worth saying right away that arthroscopy is a minimally invasive operation and leaves no scars. In the first days, the puncture sites will have slight swelling and possibly hematomas. The shoulder joint itself will feel painful, since the tissues need time to recover. During this period, the patient is required to be hospitalized: several days under the supervision of a doctor to exclude any complications.
General principles of rehabilitation
Rehabilitation after arthroscopy is a matter for patient and dedicated patients. The feeling of complete recovery will come in six months (~4-6 months). The greatest danger during the recovery period can be the progressive atrophy of the muscular frame and congestion. To prevent the development of such conditions, it is necessary to engage in therapeutic exercises, the purpose of which is to strengthen the shoulder joint and its muscle layers.
First loads
The very first movements of the shoulder joint should take place under the supervision of the attending physician. The main goal is to convey to the patient the rules and technique of performing physical therapy exercises. On day 2, the exercises are performed in three positions: lying on the healthy side, lying on the back and standing. From 3-4 days classes continue in the exercise therapy room.
From the end of the first week, it is necessary to begin to use and activate the injured limb. The exercises are aimed at improving local blood supply and preventing wasting of the shoulder muscles.
The patient's first movements are successive active and passive movements of the healthy shoulder. This technique will form a motor stereotype that will help the operated side to perform the exercises correctly. It is important to listen to your own feelings. If pain appears/increases during or after exercise, you should consult your doctor. Based on the results of the conversation, the set of exercises can be changed to another.
Rules for performing gymnastics
To achieve maximum strengthening effect, certain rules must be followed.
- A systematic approach is required! You need to exercise every day, strictly adhering to the prescribed recommendations. There should be no personal preference. If you feel unwell, the exercises are still performed, at least from the starting position while sitting.
- Compliance with safety regulations. Each movement is performed smoothly and progressively. It is important to consider the capabilities of your body so as not to harm the “sick” joint. If possible, for the first two weeks you should go to a physical therapy room and exercise under the supervision of a specialist.
- Weights and loads are increased gradually, in accordance with the recommendations. If not followed, there is a risk of repeated and irreversible damage to the joint. A new operation will be required.
- Sudden movements and excessive loads are avoided. The leverage should be in loyal mode.
Everyone wants to recover quickly so they can return to everyday life. But you should be patient - let your shoulder and muscles gain their necessary condition.
How the exercises are carried out
Active physical activity is allowed 3-6 weeks after surgery. At this point, the patient can already work with weights, rubber shock absorbers and block exercise machines. Exercise therapy is conditionally divided into three areas:
- simple actions to maintain muscle tone;
- power active loads affecting the entire shoulder area;
- loads using additional devices (expanders).
Exercises for shoulder recovery after arthroscopy
The very first movements performed are passive movements with abduction in the shoulder joint up to 90 degrees, flexion up to 90 degrees and external rotation up to 45 degrees. If the operation was extensive, then rotation should be excluded in the first stages. Exercises are performed from the starting position (IP): lying and sitting, at least 3 times a day. The lesson begins with the “pendulum” exercise (Codman exercise).
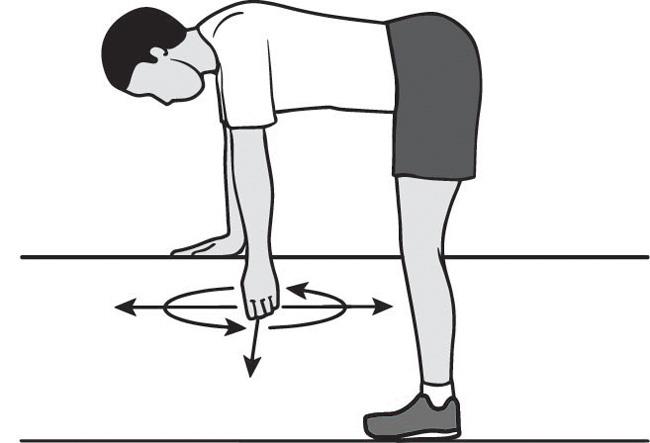
The patient rests his healthy arm on the table, while the patient hangs down freely. The exercise involves swaying your torso while keeping your arm completely relaxed. Over time, the movement of the body stops, and the hanging arm continues to swing like a pendulum. Movements are performed in different directions: left-right, forward-backward, in a circle.
Next, passive external rotation of the shoulder is performed using the healthy arm. A gymnastic stick is used as an auxiliary tool, with the help of which the affected arm is passively drawn into external rotation.
Then they perform exercises for early passive shoulder stretching in a closed circuit while sitting at a table.
Late rehabilitation period (3-6 weeks)
Tasks for this period: increase the range of motion in the shoulder joint and begin to gradually train the muscle strength of the upper limb (to be able to raise the arm to a horizontal level). Passive-active movements are added using shortened lever exercises.
Exercises are performed using a healthy hand:
In light positions:

In a closed kinematic chain (gymnastic stick):
To increase the amplitude in the shoulder joint, exercises are used with abduction of the upper limb along a sliding surface:

Using a fitball:

Using positions (position treatment):

When the shoulder is sufficiently strengthened, you can use isometric and active exercises:
- We “climb” to the top. The elbow is kept straight and, with the help of the fingers, we climb up along the wall or door lintel. The hand rises as high as possible.
- Shoulder internal rotation. The hand goes behind the back and reaches towards the opposite side of the body.
- Shoulder flexion. The arm rises to the ceiling, the elbow is kept straight.
- Bringing the arm to the body. Taking our hand to the side, we raise it, turning it palm down. In this exercise we do not move the shoulder and do not tilt the torso.
- Shoulder stretch. In a standing position, we lean the operated side of the body on the wall. In this case, the elbow is bent at an angle of 90 degrees.
- Shoulder internal rotation. We stand on the corner of the wall or at the doorway. We lean the operated shoulder against the wall and maintain this position for 5 seconds.
- Shoulder internal rotation. When lying on your side, the elbow joint is bent at 90 degrees. Holding a small dumbbell in your hands, raise your hand towards your stomach.
- External rotation of the shoulder. The technique is similar to “exercise 7”, only the hand is moved away from the stomach.
- Exercises with light weight while lying on your side.
At the final stage (8-12 weeks), it is recommended to exercise in the gym using shock absorbers and block exercise machines. Mechanotherapy (Kinetec) is in greatest demand.
Shoulder joint: structure, diseases and diagnosis
The shoulder joint is a ball-and-socket joint made of bones, cartilage, joint capsule, bursae (synovial bursae containing fluid), muscles and ligaments. Each component has its own structure and function, and together they protect joints from injury. For example, muscles and ligaments provide stability to the movable connection of bones, so we can perform movements with a wide amplitude: circular rotations, adduction and abduction of the arm, flexion and extension. If our arm consisted only of the shoulder joint, then it would not rise above the shoulders.
Paradoxically, it is the mobility of the shoulder joint and the complexity of the device that makes it vulnerable to dislocations, sprains and torn ligaments. Most often, these are injuries sustained during heavy lifting, sports, and falls. Inflammatory processes begin in damaged areas. If treatment is not started in time, you can develop diseases that not only cause pain, but also limit the mobility of your arm.
Sometimes inflammation appears as a concomitant symptom of autoimmune and allergic diseases, psoriasis, tuberculosis, diabetes, thyroid diseases, intestinal and urogenital infections. Finding the real cause of shoulder pain can only be done with the help of diagnostics and an experienced doctor.
Sports after shoulder arthroscopy
Injuries are especially common among athletes, especially in Olympic sports. The question arises: when and is it realistic to return to the previous level of one’s condition after arthroscopy of the shoulder joint? It is possible, with proper and obligatory implementation of the recommendations of the attending physician and the required recovery period.
The average recovery period (subject to continuous rehabilitation and satisfactory condition of the joint before injury) is 6 months. After decompression of the subacromial space: 2-3 months. After reconstructive surgery on the labrum (including the scapula) and acromioplasty: 6 months. After rotator cuff suture: 8-10 months.
The heavier and higher the load on the shoulder joint in a particular sport, the more carefully it is necessary to restore the muscles and their coordination.
Recovery period
In the first days after arthroscopy on the shoulder joint, symptomatic therapy and dressings are carried out under the supervision of the attending physician. The limb is fixed using a special orthotic bandage for 3-4 weeks after surgery. At the same time, rehabilitation treatment begins.
The rehabilitation course consists of carrying out a set of rehabilitation measures developed by specialists:
- specialized course of physical therapy for up to 3-4 months;
- use of devices for passive development of movements in the shoulder joint (“Artromot”);
- limiting sports and heavy physical activity for up to 4-6 months.
We perform all the joint manipulations listed in the article in the operating room of the CELT clinic, specially equipped for arthroscopic operations. Arthroscopy is often the only real opportunity to restore joint health, and, therefore, restore quality of life. If problems with the shoulder joints are relevant for you, come for a consultation with the author of the article, an orthopedic traumatologist with extensive experience in arthroscopic operations.
Of course, the best operation is the one that does not need to be done, but even in difficult cases we will try to help you!
The best doctors in Moscow and St. Petersburg
Milenin Oleg Nikolaevich
Milenin Oleg Nikolaevich
Traumatologist-orthopedist. Candidate of Medical Sciences. Specializes in the surgical treatment of ligamentous injuries and unstable conditions of the shoulder and knee joints.
Jojua Alkhas Walterovich
Jojua Alkhas Walterovich
Traumatologist-orthopedist kmn, associate professor, head of the department of traumatology of the National Medical Center named after N.I. Pirogov. Specializes in fracture surgery, osteosynthesis and endoprosthetics of large joints.
Igor Aleksandrovich Kuznetsov
Igor Aleksandrovich Kuznetsov
Professor, Doctor of Medical Sciences. Surgeon, traumatologist-orthopedist. One of the best specialists in the Russian Federation in the field of orthopedics and traumatology. 35 years of experience, of which 30 years were dedicated to arthroscopy, more than 10,000 operations were performed.
Types of arthroscopic interventions

Meniscus seam
- Cost: 70,000 - 110,000 rubles.
- Duration: 30-60 minutes
- Hospitalization: 1 day in hospital
More details
The CELT clinic performs arthroscopy of any large joints: knees, elbows, shoulders, hips, ankles, wrists. At the same time, the types of interventions are very diverse.
When pathology is detected in the ankle, wrist, elbow and hip joints, the following operations are performed:
- resection of adhesions;
- joint release;
- resection of exostoses;
- removal of chondromic bodies;
- treatment of intra-articular injuries;
- chondroplasty.
In the knee joints , in addition to the above, the following are also performed:
- resection of the damaged part of the meniscus;
- meniscal suture;
- plastic surgery of cruciate ligaments (anterior, posterior cruciate ligaments);
- plasty of the patellar retinaculum;
- mosaic chondroplasty.