Ultrasound examination is a modern, reliable method for searching for various formations and other abnormalities in our body. Such a study is considered practically safe, including for women during pregnancy and lactation, and is carried out painlessly.
When is soft tissue ultrasound prescribed?
What is soft tissue? Muscle tissue, joints, fatty tissue, lymph nodes. The procedure is usually prescribed before or after surgery to track the dynamics of treatment and study the condition of the scars left by the surgeon.
Other reasons for an ultrasound:
- painful sensations of unknown nature;
- muscle hernias;
- swollen lymph nodes;
- neoplasms and compactions in tissues;
- the appearance of foci of spread of pus;
- ruptures, hematomas and so on.
The procedure will determine the presence of a tumor, but will not make it clear whether it is benign or malignant. For more detailed information, further research is necessary.
How is the procedure done?
The ultrasound algorithm is the same for all zones:
- The patient sits on the couch and takes a comfortable position.
- Frees the necessary area from clothing and jewelry.
- A special gel is applied to the skin and the device’s sensor. This is necessary to improve gliding.
- The specialist slowly moves the sensor over the patient's skin. The internal organs are displayed on the device monitor in real time.
Ultrasound of soft tissues takes place without any discomfort. The only thing the patient experiences is a slight chill from the special gel. If necessary, the study can be repeated. Ultrasound is often prescribed for infants.
When is soft tissue ultrasound prescribed?
Ultrasound of the anterior abdominal wall
usually prescribed for acute pain, suspected hernia, or tumor.
Ultrasound of soft tissues of the extremities.
If a lump of unknown origin appears on the arm, leg, or thigh, an ultrasound is prescribed. Also, reasons for referral for an ultrasound of the soft tissues of the extremities may be the consequences of injuries, the appearance of pain at rest or movement, suspected inflammation of the joints or an abscess (purulent inflammation), etc.
Ultrasound of soft tissues of the groin area.
Prescribed for enlarged lymph nodes as a result of infection or inflammation, suspected tumor or inguinal hernia, abscess of the iliopsoas muscle, hemorrhages, etc.
Ultrasound of the face, neck and maxillofacial area. An ultrasound examination is performed when signs of inflammation appear, cysts or other neoplasms on the face are suspected, or after plastic surgery.
Ultrasound of the soft tissues of the neck is prescribed when the lymph nodes are enlarged, there is a need to assess the condition of the arteries, etc.
Types of ultrasound scanning
For ultrasound diagnostics of leg vessels in modern diagnostic practice, 3 main types of ultrasound scanning are used:
- Doppler ultrasound, classical two-dimensional Doppler ultrasound. Allows you to record the main parameters of blood flow with determination of its speed. More often than other methods, it is used to identify pathologies of the veins, arteries and vessels of the legs. Such devices are extremely portable and are present in all medical institutions in the country.
- Ultrasound scanning, duplex angioscanning. It combines standard Dopplerography and color mapping, which makes it possible to determine not only the structure and speed of blood flow, but also its direction - multidirectional flows are painted in colors different from each other, which makes it possible to comprehensively monitor the main indicators of veins and vessels.
- Triplex scanning. The most informative technique that allows you to obtain a three-dimensional color image of the vascular system of the legs. It should be taken into account that triplex angioscanning does not allow one to determine the speed of blood flow - in this situation, if necessary, the equipment switches to a two-dimensional mode and scanning is performed using the classical ultrasound Doppler technique.
It should be noted that all of the above ultrasound diagnostic methods are used universally for monitoring the vascular system in the soft tissues of both extremities and other parts of the body. Preparation for an ultrasound examination of the veins and vessels of the lower extremities does not require long-term and comprehensive preparation, and in severe cases it is carried out without it at all. The basic rules for preparing ultrasound of the veins and vessels of the extremities are usually considered by diagnosticians:
- Refusal to take medications. If possible, 3 days before the procedure, it is necessary to avoid taking medications that may affect systemic blood flow parameters. If it is impossible to refuse (vital medications), you need to inform the diagnostic doctor about the regular use of such substances, indicating the active substance and the scheme of use - this information will help adjust the monitoring process.
- Limiting the consumption of foods that speed up the heart. We are talking about strong coffee and tea, chocolate, natural or artificial heart rhythm stimulants. The ban on their use must be adhered to for 24 hours.
- Elimination of alcohol and tobacco smoking. 2 days before the ultrasound, you need to stop drinking alcohol in any form. Smoking cigarettes is prohibited 2-3 hours before the procedure.
- Personal hygiene. Before ultrasound diagnostics, it is recommended to shave off excess hair from your legs and wash your legs thoroughly.
Possible results
Ultrasound of the soft tissues of the neck, limbs and other parts of the body does not normally reveal any structural abnormalities or neoplasms. Using this method, the doctor can detect suppurations caused by the inflammatory process, tendon ruptures, nerve damage, enlarged lymph nodes, etc. Various tumors become clearly visible on ultrasound. They look different, which makes it possible to assume or accurately determine their nature. Thus, a lipoma (a neoplasm of adipose tissue) is homogeneous and does not have its own blood supply, a hematoma is filled with blood, malignant tumors have unclear boundaries and a good blood supply. You will find all the detailed information about the examination results in the doctor’s report.
Advantages of contacting the Central Clinical Hospital of the Russian Academy of Sciences
- highly qualified doctors with extensive practical experience, able to quickly recognize not only common, but also rare diseases;
- attentive, caring attitude of medical staff towards each patient;
- the possibility of undergoing comprehensive diagnostics;
- use of advanced equipment with high precision;
- affordable cost of elastography (significantly lower than in many other clinics in Moscow and the Moscow region).
At the Central Clinical Hospital of the Russian Academy of Sciences, it is possible to conduct elastography of internal organs, soft tissues, and mammary glands. If pathological changes are detected, the patient can immediately seek help from the appropriate specialist in order to immediately begin treatment according to an individual program.
You can make an appointment for an ultrasound with elastography or an appointment with a doctor by phone or on the website.
What can an ultrasound specialist detect?
Ultrasound of soft tissues allows you to assess their functional state, detect changes in structure, identify benign or malignant tumors, and signs of inflammation. When performing an ultrasound of soft tissues, it is possible to identify pathologies such as lipoma (adipose tissue that forms a benign tumor that does not contain fluid and blood vessels), hematoma (due to bruises a cavity filled with blood appears), hygroma (a benign subcutaneous formation that is filled with serous fluid), atheroma (suppuration of the sebaceous gland), cysts, abscesses.
A contraindication for soft tissue ultrasound is an open wound in the area where diagnosis is planned.
Symptoms that indicate the need for examination
the appearance of compactions in the area of the mammary glands, neck, lymph nodes, soft tissues;- frequent nausea, vomiting with bile, digestive disorders, the appearance of plaque on the tongue;
- the appearance of a yellowish tint to the skin or whites of the eyes;
- the appearance of nipple discharge not related to feeding;
- pain, pulling sensations in the chest;
- urinary disorders;
- significant deviations from the norm in the results of blood tests;
- noticeable weight loss or gain for no obvious reason;
- a sharp deterioration in general health without a specific reason.
Despite the absence of dangerous side effects, performing ultrasound with elastography may be undesirable in some cases:
- during pregnancy;
- if you have an installed electrical stimulator;
- in case of disturbances, confusion or exacerbation of mental illness;
- in the presence of free fluid in the abdominal cavity;
- in the late stages of obesity.
The final decision on the need and admissibility of performing the study is made by the doctor, based on the patient’s complaints, examination data and test results.
Possibilities of ultrasound diagnosis of acute paraproctitis. Clinical observation

Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Introduction
Acute paraproctitis is an acute inflammation of the peri-rectal tissue, caused by the spread of the inflammatory process from the anal crypts and anal glands [1-3].
Acute paraproctitis is the most common disease in the practice of emergency surgical coloproctology. Patients in this group make up about 1% of all patients hospitalized in various surgical hospitals and 5% of those suffering from diseases of the colon and rectum [4]. Among acute purulent lesions of the anorectal area, the frequency of acute paraproctitis approaches 45% [5]. Acute paraproctitis is widespread and has been the subject of lively discussions in the pages of domestic and foreign literature for many decades. The most frequently discussed are ischiorectal, pelviorectal, retrorectal and horseshoe-shaped abscesses, which, according to various sources, occur on an impressive scale: from 5 to 58% of cases of acute paraproctitis [6, 7]. The development of acute paraproctitis is due to a number of predisposing factors, such as: weakened immunity due to concomitant acute or chronic infection, vascular changes due to diabetes mellitus, gastrointestinal disorders, the presence of hemorrhoids, anal fissure, cryptitis [1, 3, 8].
Currently, in clinical practice, a classification is used that subdivides acute paraproctitis according to the nature of the pathogen, the localization of the lesion, the localization of the crypt involved in the inflammation process, and the nature of the purulent course. The classification is used to determine the severity of the lesion and select a treatment method [3, 9]. In clinical practice, this classification is most often used in the following form (table).
Table.
Classification of acute paraproctitis.
| I. By the nature of the pathogen |
|
| II. By location of the lesion |
|
| III. According to the localization of the crypt involved in the inflammation process |
|
| IV. According to the nature of the purulent course |
|
In recent years, ultrasound (US) diagnostics has been increasingly used for topographic characterization of acute paraproctitis. Compared to the huge number of ultrasound studies of various organs and systems, the experience of their use in coloproctology is presented rather modestly in both domestic and foreign literature [10, 11].
Ultrasound allows one to assess the localization, size, structure of the pathological focus, the presence of additional passages, the degree of involvement of the rectal wall and external sphincter fibers in the inflammatory process, the depth of the pathological focus from the skin [10, 12, 13]. The information content of an ultrasound examination in determining acute paraproctitis is 80-89% [10, 12, 13].
Material and methods
The study is carried out using ultrasound machines using linear and cavity sensors in gray scale mode and ultrasound angiography using a transperineal or transrectal/transvaginal approach.
When examining a transperineal linear sensor, a linear sensor is installed on the perianal area and the walls of the anal canal, subcutaneous fat and perineal muscles are examined polypositionally.
When examining transrectally (TRUS), a cavity sensor is inserted into the anal canal to a patient lying on his left side at a distance of up to 8 cm with a rubber balloon previously placed on it and the air pumped out of it. Through the adapter, the canister is filled with distilled water (30-50 ml), which ensures good conductivity of the ultrasound beam. The sensor is used for rotational movements clockwise and a linear ultrasound scan is performed by obtaining longitudinal sections of the anal canal by rotating the sensor. The accuracy of ultrasound examination reaches 90% [14-18].
D.Yu. Fillipov [19], L. Stewart et al. [20] came to the conclusion that endorectal sonography makes it possible to more reliably determine the nature of pathological changes in the cellular spaces and carry out a differential diagnosis of acute paraproctitis with diseases of neighboring organs. The sensitivity and specificity of the method, according to D.Yu. Fillipov [19], were 89 and 80%, respectively, and the overall accuracy was 86%. L. Stewart et al. indicate that preoperative sonography data were confirmed during surgery in 85% of cases [20].
Clinical observation
Patient A., 43 years old, came to the clinic with complaints of pain in the anus and the appearance of a painful lump in the anus. The above complaints bothered the patient for a week. Upon examination, the general condition is satisfactory. The skin and visible mucous membranes are pale pink in color. There are no respiratory or hemodynamic disturbances. Blood pressure 120/80 mm Hg. Art. Pulse - 72 beats/min, rhythmic. The abdomen is not swollen, soft, painless on palpation. The stool is regular and formed. There is no dysuria. Status localis: upon palpation in the subcutaneous tissue of the left buttock, an irregularly shaped infiltrate measuring 4x2 cm, of a tight-elastic consistency, painful on palpation, the skin over it is not changed. During a digital examination of the rectum at 2-3 o'clock on a conventional dial in the distal third of the anal canal, a funnel-shaped retraction (internal fistula opening?) is not clearly defined in the scars. The patient was given a clinical diagnosis: “acute subcutaneous paraproctitis.”
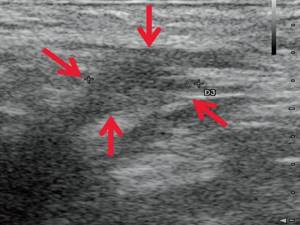
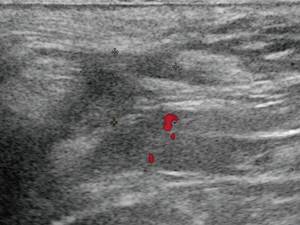
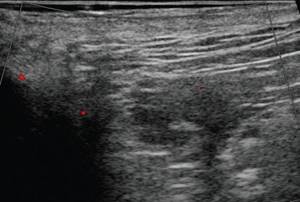
Ultrasound examination of the soft tissues of the perineum revealed: in the perianal area on the left in the projection of a palpable compaction at 2-3 o'clock on the conventional dial closer to the anal canal at a depth of 0.6 cm from the surface of the skin, a hypoechoic liquid formation with clear uneven contours with the presence of heterogeneous hyperechoic mobile contents measuring 3.9×2.1×1.9 cm, volume 8.24 ml with walls thickened to 0.3 cm. The described formation is adjacent to the anterolateral thickened wall of the anal canal and is not clearly differentiated from it (see Fig. 1, a, b). Along the periphery of the formation there is a pronounced vascular reaction (see Fig. 1, c). Along the periphery of the formation, closer to the gluteal region, there is a developing fistula tract measuring 1.3×0.6×0.6 cm (see Fig. 1, d).
Rice. 1.
Ultrasound of soft tissues of the perineum. Patient A.
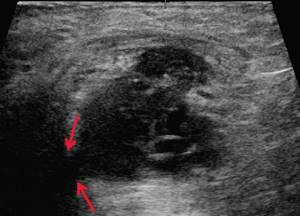
a, b)
B-mode. In the perianal area on the left, at a depth of 0.6 cm from the surface of the skin, a hypoechoic liquid formation with clear uneven contours with the presence of heterogeneous hyperechoic mobile contents measuring 3.9 × 2.1 × 1.9 cm, volume 8.24 ml, thickened to 0 .3 cm walls. The described formation is adjacent to the anterolateral wall of the anal canal, thickened to 1.0 cm, and is not clearly differentiated from it (arrows).
V)
Color flow mode. In the subcutaneous fat along the periphery of the formation, an enrichment of the vascular pattern is noted.

G)
B-mode. Along the periphery of the formation, closer to the gluteal region, there is a developing fistulous tract measuring 1.3×0.6×0.6 cm (arrows).
With TRUS, the anterior wall of the anal canal is thickened to 1.3 cm, has a heterogeneous structure, and reduced echogenicity; the posterior wall is thickened to 0.8 cm, has a somewhat heterogeneous structure, and moderately reduced echogenicity. The vascular pattern in the anterior wall is moderately enriched.
For emergency reasons, the patient underwent surgical intervention to open and drain the subcutaneous acute paraproctitis.
In the postoperative period, the patient was given antibacterial therapy, daily dressings were performed (washing the wound with antiseptic solutions, applying bandages with water- and fat-soluble ointments).
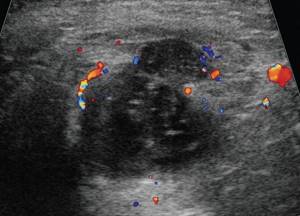
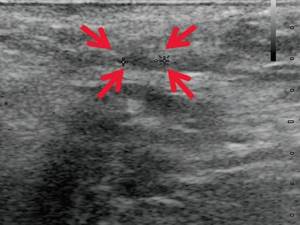
During a control study 3 days after surgery: the described hypoechoic liquid formation with clear uneven contours and the presence of heterogeneous hyperechoic moving contents decreased in size to 2.4×1.7×1.8 cm and volume to 3.84 ml (Fig. 2, a, b). In the subcutaneous fat along the periphery of the hypoechoic formation, a decrease in the severity of the vascular reaction is noted (Fig. 2, c). The described fistulous tract decreased in size to 1.1×0.2×0.5 cm (Fig. 2, d).
Rice. 2.
Ultrasound of soft tissues of the perineum. Patient A, 3 days after surgery.
a, b)
B-mode. The described hypoechoic liquid formation with clear uneven contours with the presence of heterogeneous hyperechoic moving contents decreased in size to 2.4 × 1.7 × 1.8 cm, to a volume of 3.84 ml (arrows).
V)
Color flow mode. 3 days after surgery. In the subcutaneous fat along the periphery of the hypoechoic formation, a decrease in the severity of the vascular reaction is noted.

G)
B-mode. 3 days after surgery. The described fistulous tract decreased in size to 1.1 × 0.2 × 0.5 cm (arrows).
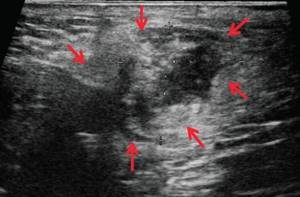
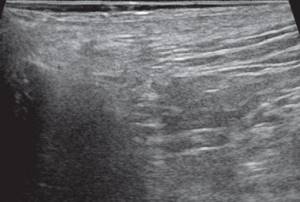
During a control ultrasound examination 14 days after surgery: the described hypoechoic liquid formation with clear uneven contours decreased in size to 1.1 × 0.6 × 0.8 cm and volume to 0.29 ml (Fig. 3, a, b). The vascular reaction in the subcutaneous fat is not determined (Fig. 3, c). The fistula tract is not clearly visualized and has decreased in size to 0.8×0.2×0.4 cm (Fig. 3, d).
Rice. 3.
Ultrasound of soft tissues of the perineum. Patient A, 14 days after surgery.
a, b)
B-mode. 14 days after surgery. The hypoechoic liquid formation with clear, uneven contours in the perianal area decreased in size to 1.1×0.6×0.8 cm, volume 0.29 ml (arrows).
V)
Color flow mode. 14 days after surgery. The vascular reaction in the subcutaneous fat is not determined.
d, e)
B-mode. 14 days after surgery. The fistula tract is not clearly visualized and has decreased in size to 0.8×0.2×0.4 cm (arrows).
After 3 months, at a follow-up examination, the patient had no complaints. Status localis: at 1-2 o'clock, a linear postoperative scar without signs of inflammation is determined on the conventional dial at a distance of 2.0 cm from the edge of the anus. During a digital examination of the rectum at 2-3 o'clock, scar changes are determined in the distal third of the anal canal (obliterated internal fistulous opening?).
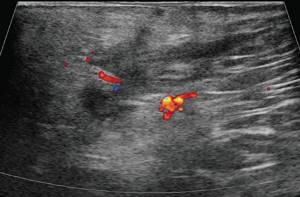
During the control ultrasound examination: the previously described liquid formation in the subcutaneous fat tissue is not clearly visualized; in its projection there is moderate tissue heterogeneity without clear focal changes (Fig. 4, a). The vascular pattern in the subcutaneous fat in this projection is not enriched (Fig. 4, b).
Rice. 4.
Ultrasound of soft tissues of the perineum. Patient A, 3 months after surgery.
A)
B-mode. The previously described fluid formation with a fistulous tract in the subcutaneous fat is not clearly visualized; its projection shows moderate tissue heterogeneity without clear focal changes.
b)
Color flow mode. The vascular pattern in the subcutaneous fat is not enriched in this projection.
Conclusion
Thus, an ultrasound examination of the perianal area in acute paraproctitis makes it possible to determine the location, size of the abscess, the nature and amount of the contents of the purulent cavity, the depth of the pathological focus from the skin, infiltration of the subcutaneous tissue, the presence of fistulous tracts and additional purulent leaks, which is of particular importance to establish a diagnosis and then select the scope of treatment.
Literature
- Dultsev Yu.V., Salamov K.N. Paraproctitis. M.: Medicine 1981. 208 p.
- Kaiser Andreas M. Colorectal surgery. M.: BINOM Publishing House 2011. pp. 473-477.
- Shelygin Yu.A., Blagodarny L.A. Handbook of coloproctology. M.: Litterra 2012. 596 p.
- Zhukov B.N., Isaev V.R., Chernov A.A. Fundamentals of coloproctology for a general practitioner: monograph. Samara, RF: Etching 2009. 218 p.
- Akopyan A.S. and others. Improving the results of treatment of patients with acute paraproctitis // Collection: Problems of coloproctology. M., 2002. Issue. 7. pp. 24-28.
- Slesarenko S.S., Fedorov V.E. Results of surgical treatment of acute paraproctitis // Collection: Current problems of coloproctology. M., 2005. Issue. 8. pp. 125-126.
- Vasilveski CA Anorectal abscesses and fistulas. In: Wolff BG, Fleshman JW, Beck DE, Pemberton JH, Wexner SD, eds. The ASCRS Textbook of Colorectal Surgery. New York: Springer. 2007. R. 192-214.
- Bolkvadze E.E. Complex forms of acute paraproctitis. Literature review // Coloproctology. 2009. 27 (1). pp. 38-46.
- Vorobyov G.I. Basics of coloproctology. M.: Medical Information Agency, 2006. 430 p.
- Orlova L.P. Ultrasonography in the diagnosis of diseases of the rectum and pararectal region: Abstract of thesis. diss. ... doc. honey. Sci. M., 1992. 44 p.
- Santoro GA, Di Falco G. Benign Anorectal Diseases. Diagnosis with Endoanal and Endorectal Ultrasound end New Treatment Options // Springer-Verlag Italia. 2006. 404 p.
- Santoro GA, Fortling B. The advantages of volume rendering in three-dimensional endosonography of the anorectum // Dis Colon Rectum. 2007. 50. R. 359-368.
- Toyonaga T., Tanaka Y., Song J.F. et al. Comparison of accuracy of physical examination and endoanal ultrasonography for preoperative assessment in patients with acute and chronic anal fistula // Tech Coloproctol. 2008. 12. R. 217-223.
- Buchanan GN, Bartram CI, Williams AB, Halligan S., Cohen CR Value of hydrogen peroxide enhancement of three-dimensional endoanal ultrasound in fistulainano // Dis Colon Rectum. 2005. 48. R. 141-147.
- West RL, Zimmerman DD, Dwarkasing S et al. Prospective comparison of hydrogen peroxide-enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging of perianal fistulas // Dis Colon Rectum. 2003. 46. R. 1407-1415.
- Shobeiri SA Practical pelvic floor ultrasonography. A multicompartmental approach to 2D/3D/4D ultrasonography of Pelvic floor // Springer Science+Business Media New York 2014.
- Pescatori M., Regadas FSP, Regadas SMM, Zbar AP Imaging atlas of the pelvic floor and anorectal diseases // Springer-Verlag Italia 2008.
- Tonolini M., Maconi G. Imaging of perianal inflammatory diseases // Springer-Verlag Italia 2013.
- Fillipov D.Yu. Ultrasonography in the diagnosis of acute paraproctitis. Author's abstract. diss. ...cand. honey. Sci. M., 1999. 25 p.
- Stewart LK, McGee J., Wilson SR Transperineal and transvaginal sonography of perianal inflammatory disease // Am. J. Roentgenol. 2001. V. 177 (3). P. 627-632.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Benefits of Ultrasound with Elastography

targeted scanning, providing high accuracy and information content;- painlessness;
- safety;
- no need for special preparation for the procedure;
- high research speed, quick results;
- low cost.
In many cases, elastography can provide accurate information about the presence of pathological changes without performing a painful biopsy procedure. This is a very important point, because some types of biopsy, for example, taking a sample of kidney tissue, are unsafe for health. However, it should be remembered that if elastography reveals the presence of a malignant formation, the attending physician may decide on the need to conduct a microscopic morphological examination of the tissue sample.
FAQ
- Is it painful to have an ultrasound examination?
No, this is a non-invasive and painless diagnostic method.
- Will ultrasound be enough to make a diagnosis?
It all depends on the disease; for some diseases, only an ultrasound is sufficient, while others will require a more in-depth examination, such as magnetic resonance imaging or blood tests.
- Does ultrasound replace radiography of the joint?
No, ultrasound does not make it possible to assess the nature of the bone fracture, the presence of fragments and displacement. Therefore, in case of injuries and suspected fracture, it is better to first conduct an X-ray diagnosis.
- How often can an ultrasound be done?
The ultrasound diagnostic method is absolutely harmless; if necessary, it can be done as many times as necessary.
- Is it possible to consult a specialist after an ultrasound?
Yes, you can get advice from a specialized specialist - a traumatologist, orthopedist, physiotherapist or sports doctor. You can also undergo treatment with us, and you can start on the same day you contact us.
- Do I need to somehow prepare for an ultrasound diagnosis of a joint?
No special preparation is required for ultrasound examination of joints and soft tissues. A contraindication to an ultrasound examination may be the presence of a plaster cast, wound or abrasion.
Preparing for the study
Ultrasound diagnostics of soft tissues does not imply any preliminary preparation. There is no need to follow dietary guidelines or drink large amounts of water. It is recommended to simply wear loose, comfortable clothing that can be easily removed if necessary. If you have recently had an x-ray, it is important to tell your doctor. Since during an x-ray, substances accumulate in the body that will be eliminated within five days, they can significantly distort the results of an ultrasound.









