Ureaplasma (family Mycoplasmaсea) is constantly present in the mucous membranes of the human genital organs and respiratory tract. But the harmless symbiosis lasts for the time being. Once you relax and boost your immune system, these microorganisms become active and cause a serious infectious disease - ureaplasmosis. Gynecologists and urologists advise timely testing for ureaplasmosis (ureaplasma), since this disease ends in purulent infections, infertility and other very unpleasant diseases.
CONSULTATION ON THE RESULTS OF TESTS or ultrasound with a UROLOGIST, GYNECOLOGIST - 500 rubles.
CLICK TO SIGN UP
What is ureaplasma and why is it so dangerous?
The content of the article
The size of ureaplasmas is close to viruses, but the composition of cells is close to bacteria, which have DNA and RNA. This is rather a transitional stage from microorganisms to unicellular organisms. Pathogens do not penetrate into the nucleus or cytoplasm (liquid part of the cell) of the host cell, but are located on the surface of cell membranes, penetrating into them. Thus, ureaplasmas “escape” phagocytosis (attack by immune cells), which determines their ability to live in the body for a very long time. This condition is called persistence.
Ureaplasmas were previously classified as similar microorganisms - mycoplasmas, but due to their distinctive ability to break down urea, ureaplasmas were placed in a separate group. At the same time, the ability to form ammonia from urea is the main reason for the harmfulness of these microorganisms. Ammonia has a toxic (poisonous) effect on the cells of the urogenital tract in men and women and disrupts the biocenosis (composition of living flora) of the vagina, reducing local immunity. This is associated with torpid (acute) and recurrent (repeated) course of urethritis and vulvovaginitis.
Disputes still continue over the true classification of the pathogen. In Russia, in 2000, Order No. 315 of the Ministry of Health of the Russian Federation was issued, excluding ureaplasmosis from the list of sexually transmitted infections - i.e. the disease is not classified as an STI. But according to the WHO (World Health Organization) classification of sexually transmitted infections, in 2006 the subspecies Ureaplasma urealyticum (ureaplasma urealyticum) was specifically classified as a causative agent of sexually transmitted infections. Therefore, we can say that analysis for ureaplasmosis is included in the spectrum of examination for sexual and non-genital infections.
Cause and epidemiology
Mycoplasma hominis and Ureaplasma spp. – opportunistic microorganisms that, when realizing their pathogenic properties, can cause urethritis (U.urealyticum), cervicitis (inflammation of the cervix), cystitis, pelvic inflammatory disease (PID), as well as complications during pregnancy and post-abortion complications.

For me personally, the big question is how to reliably determine that a pregnancy complication is caused by the presence of ureaplasmas, if statistically they occur in 50-70% of people.
The frequency of detection of Ureaplasma varies widely in different population groups, ranging from 10% to 50% (according to some authors - up to 80%, while usually true pathology does not exceed 10%). (Author's note - usually true pathology does not exceed 10%)
WHO experts (World Health Organization, 2006) identified U.urealyticum as a potential causative agent of urethritis in men, and possibly PID in women. At the same time, experts from the US Centers for Disease Control and Prevention (CDC, 2010) do not consider the presence of ureaplasma to be proven as a cause of the development of inflammatory processes in the genitourinary system.
Why do you need to get tested for ureaplasmosis?
A gynecologist or urologist refers patients for tests, suggesting that this pathogen is the cause of inflammation in the genitourinary system. The reason is an ongoing treatment that is not yielding results.
Due to the absence of a cell wall - it was replaced by a three-layer cell membrane, ureaplasmas are resistant (resistant) to drugs that destroy pathogens precisely through their effect on cell walls. The number of drugs that cannot cope with ureaplasma includes penicillin and its derivatives, which are the main drugs prescribed for the treatment of most sexually transmitted infections.

A complete test for ureaplasmosis identifies the microorganism itself, determines its concentration, and checks the resistance of ureaplasma to various drugs. Treatment will be prescribed after identifying a drug that can affect the pathogen.
Official information
Below, I quote verbatim excerpts from the fundamental document that should guide doctors (dermatovenereologists, gynecologists, urologists) in matters of diagnosis and treatment of ureaplasma. (Author's note - this document is in the public domain and can be easily found on the Internet)
“Federal clinical guidelines for the management of patients with urogenital diseases caused by Ureaplasma spp, Mycoplasma hominis”, Moscow, 2015.
Recommendations were developed by the Russian Society of Dermatovenereologists and Cosmetologists and the Russian Society of Obstetricians and Gynecologists.
Code according to the International Classification of Diseases (ICD-10) – A63.8 – Other specified diseases transmitted predominantly
sexually. (Author's note - the operative word here is "primarily")
When is a test for ureaplasmosis necessary?
The analysis is prescribed in the absence of other possible causes of inflammation. The main indications for determining ureaplasma: diagnosis of ureaplasma infection, urethritis, pelvic inflammatory disease, infertility.
This analysis is necessary to identify the etiological (main, determining) factor of chronic inflammation in the genitourinary system, for differential diagnosis (comparison when clarifying the diagnosis) with chlamydia, gonorrhea, mycoplasma infection, for choosing antibacterial therapy, assessing the results of taking antibiotics, and conducting a preventive examination.
If the cause of infertility is established, it is especially important to identify the species Ureaplasma urealyticum (previously indicated in the transcript of test results as “biovar T-960”). This opportunistic microorganism parasitizes the sperm membrane and the epithelial layer (upper, integumentary) of the mucous membrane of the genitourinary system.
Introduction
Ureaplasmas received their name due to the ability to break down urea in urine under the action of the produced enzyme urease (urina - urine, translated from Latin).
In the genus Ureaplasma spp there are two species – Ureaplasma urealyticum and Ureaplasma parvum. Differences between ureaplasmas and obvious pathogens
(sexually transmitted infections)
- found in 50-70% of healthy people
- may be detected in children
- often detected in only one of the two partners
- as a rule, they are very difficult to treat and are often diagnosed again after 2-3 courses of antibiotic therapy
What tests are taken for ureaplasma?
Ureaplasmas include two types of parasites - U. Urealyticum, U. Parvum. Doctors use the term U. species to denote both species when interpreting tests. Ureaplasma species are so-called unidentifiable ureaplasmas, in other words, all possible species that were not typed during the analysis.
Culture for ureaplasma does not determine its type, therefore, if it is necessary to clarify which pathogen - U. urealyticum or U. parvum is present in the body, you need to take a PCR test. The material for inoculation for ureaplasma urealiticum is discharge from the urogenital tract.
Ureaplasma (U. species) is considered as a cause of inflammation in the genitourinary tract, if tests do not reveal other pathogenic microorganisms that cause these diseases. For accurate diagnosis, the method of cultivation on nutrient media (seeding is done) is suitable. Practice shows that in 80% of cases with ureaplasma, other pathogens are also detected - mycoplasma, chlamydia, and other anaerobic (not requiring oxygen) flora.
Story
Microorganisms of this genus were discovered in the mid-20th century while studying bacteria living in the genitourinary tract. At the same time, it was suggested that they might be involved in the development of inflammation in this area in some cases. Then nothing was heard about them for several decades. This is due to the fact that, being small in size and unable to grow on nutrient media, there was no possibility of diagnosing them in practical medicine. And only with the advent of the PCR (polymerase chain reaction) diagnostic method in the 80s, they began to be identified and treated abroad. This was convenient for doctors, since sometimes not understanding the true cause of inflammation in the genitourinary organs, ureaplasma was almost always detected and was the basis for prescribing antibacterial therapy.
However, over time, their frequent detection and repeated presence in control tests after treatment made scientists think about the true pathogenicity of these microorganisms. Articles of that time talking about possible involvement in infertility, miscarriage, fetal pathology, inflammation in the genital organs did not have scientific validity and statistical evidence. Since approximately 2000, most progressive countries in Europe and North America have not carried out examination and treatment of ureaplasmas, considering them to be normal endogenous (internal) flora, which is often detected even in children.
How does a person become infected with ureaplasmosis?
The source of infection is a patient with ureaplasma infection or a carrier of ureaplasma. You can get infected in several ways:
- Antenatal
- intrauterine. Up to 23% of unborn children become infected from sick mothers. - Intrapartum
- infection during childbirth. Only 50% of newborns have a chance to remain healthy. Once in the genital tract of a newborn, ureaplasma can remain there in an inactive state for an unlimited time. If there is a normal microflora - a kind of physiological barrier, the infection does not manifest itself in any way. - Contact-household
- this happens very rarely, since the pathogens are not viable in the external environment. And yet, this is possible if the microorganism is in humid, warm conditions, with poor air access, for example, in a public shower that is not cleaned or ventilated. Slippery walls, slimy from dampness, which do not get hot water, are very reminiscent of the conditions in the body. - Sexual
is the main route of infection. A sick person can infect a healthy partner during sexual intercourse. Most often, carriers of ureaplasmosis are women.
Infection is not yet a disease, but already a carrier state. Those. a person is already capable of infecting sexual partners.
What is ureaplasma?
Ureaplasma is a bacterium whose properties are similar to unicellular microorganisms and viruses.
This bacterium is a membrane parasite and does not have its own cell wall.
To survive, ureaplasma needs to penetrate another cell.
This structural feature makes this bacterium resistant to most antibacterial drugs.
In the human body, ureaplasma may not cause changes in health status for a long time.
According to official data, it is part of the intimate microflora of 75% of adult women and 45% of men.
People do not report any unpleasant sensations when they are carriers.
However, many people do not even realize that ureaplasma lives in their body.
And many do not even know about the existence of this bacterium and are tested for it only as prescribed by a doctor.
Symptoms of ureaplasmosis
Symptoms of ureaplasmosis are minor, sometimes they do not appear at all. 20-30 days after infection, the patient may experience itching and burning when urinating. Men may experience discomfort in the groin area, and sometimes there is mucous discharge from the urethra.
Women are much less likely to experience symptoms of the disease: pain in the lower abdomen, burning during urination, vaginal discharge. The symptoms of ureaplasmosis are similar in many ways to other inflammatory processes. Advanced ureaplasmosis in women often causes inflammation of the appendages, vagina and uterus, can lead to complications of pregnancy and infertility, and in men cause urethritis and prostatitis. Consequently, patients experience new symptoms of urological diseases.
If the patient’s immunity is very weak, then ureaplasma spreads higher up the genital tract (ascending route). The result of this is inflammation of the uterus (endometritis) and appendages (adnexitis). Signs of widespread inflammation are menstrual irregularities with intermenstrual bleeding. Critical days become abundant and long. An important sign is nagging pain in the lower abdomen.
Detailed description of the study
Ureaplasma urealiticum is a type of tiny mycoplasma bacteria. The absence of a complete cell wall allows ureaplasma to easily penetrate the epithelium of the genitourinary tract. The life cycle of these bacteria takes place inside epithelial cells, where they are protected from attack by immune cells and can remain in the body for a long time. U. urealiticum is classified as an opportunistic inhabitant of the genitourinary tract. Normally, ureaplasma can be detected in the microflora of a healthy person, without causing inflammatory reactions, but under certain circumstances they can provoke the development of this process. They can be transmitted through sexual contact through mucous membrane secretions. Cases of infection of newborns from infected mothers during passage through the birth canal have been reported. Pathological reproduction of ureaplasma with an imbalance of microflora occurs against the background of decreased immunity, hormonal imbalance, chronic diseases, stress, and disruption of work and rest. Men infected with U. urealiticum may experience the development of urethritis and, less commonly, lesions of the testicles and their appendages. Seeing a doctor is usually associated with a burning sensation when urinating, discharge from the urethra, pain and swelling of the testicle. Women also suffer from urethritis caused by pathological reproduction of ureaplasma. In addition, the infection can enter the vagina, uterus and its appendages, resulting in inflammatory diseases of the pelvic organs - cervicitis, endometritis, adnexitis. A visit to a gynecologist is often associated with pain in the lower abdomen, including during sexual intercourse, an increase in the amount of vaginal discharge with an unpleasant odor, and cutting pain when urinating. The chronic course of ureaplasmosis can disrupt the patency of the fallopian tubes and promote the formation of adhesions in the pelvis, which makes pregnancy difficult. Infection negatively affects the health of pregnant women and the fetus and poses a threat of premature birth. Sowing the material obtained by scraping from the urogenital tract allows you to confirm the diagnosis and prescribe treatment to avoid complications of the disease.
Due to the annual update of the criteria for assessing the sensitivity of flora, the range of selected antibacterial drugs for a particular microorganism may differ from the previously provided list of drugs for this microorganism; some antibiotics may be missing.
Why is ureaplasmosis dangerous for men and women?
In men
ureaplasma - the cause of inflammation of the urethra (diagnosis - non-gonococcal urethritis), bladder (acute and chronic cystitis), prostate (acute and chronic prostatitis), damage to the testicles (orchitis), and epididymis (epididymitis). Also, ureaplasmosis impairs the quality of sperm, causing a weakening of sperm motility and number, and this is guaranteed infertility. Ureaplasma also affects other organs, causing reactive arthritis and urolithiasis.
Among women
Ureaplasma is a common cause of inflammation of the vagina (vaginitis), cervix (cervicitis), and neoplasms. With weak immunity, inflammation of the uterus (endometritis) and its appendages develops (adnexitis with complications of the fallopian tubes (development of adhesions). This guarantees ectopic pregnancy and infertility. In addition, ureaplasmosis is the cause of cervical insufficiency, miscarriages, chorioamnionitis, the birth of premature, malnourished children ( less than 2500 g), as well as bronchopulmonary diseases (pneumonia, dysplasia), bacteremia and meningitis in newborns.
The problem with ureaplasmosis during pregnancy is that when ureaplasma is detected, the gynecologist has to choose between two dangerous consequences:
- If ureaplasmosis in a pregnant woman is not treated, then there is a risk that the child will be born sick immediately or the infection will manifest itself later.
- If ureaplasmosis is treated, and for this it is necessary to use a strong antibiotic, then the newborn can also expect consequences only caused by the drugs. Antibiotics can also cause miscarriage.
This is why gynecologists prescribe tests for ureaplasmosis when planning pregnancy and in the earliest stages. If ureaplasma is detected before 6 weeks of pregnancy, a woman can have a safe medical abortion by planning a pregnancy after treatment.
How is scraping for ureaplasma performed?
Material for research is taken using a sterile probe.

It is introduced into the cavity of the structures of the urogenital tract.
During scraping, epithelial cells, mucus and microorganisms are captured with a sterile probe.
The latter are found in it or colonize the surface of the mucous membranes.
In men, material is taken directly from the urethral mucosa.
Danger for children
In children infected by their mothers, ureaplasmosis is activated with weak immunity. The immune system is quickly weakened by colds, congenital pathologies, poor nutrition, living in a poor environment, etc. Ureaplasma is found in the lungs of premature babies with pneumonia, respiratory distress syndrome, and bronchopulmonary dysplasia. Its isolation from the spinal fluid (cerebrospinal fluid) in the absence of pleocytosis, with meningitis, and hemorrhages in the ventricles of the brain has been described.
It has been established that in children infected in utero with Ureaplasma urealyticum, in the first 7 years of life, the level of nonspecific inflammatory diseases of the respiratory system and gastrointestinal tract (gastrointestinal tract) is increased almost 4 times. But at the same time, determining ureaplasma in a child without signs of pathology is not an indication for prescribing an antibiotic. Treatment is carried out only for manifest disease with culture isolation.
What results can you get?
The interpretation of the results obtained is carried out by the attending physician.
If a culture (bacteria culture) was taken for ureaplasma and mycoplasma, you can see the designations in the form of a titer in the laboratory document.
If the titer is less than 105 CFU/ml, there is no infection; if the titer is higher, treatment will most likely be required.
When taking a PCR test, the test results will have two options - “negative” or “positive”.
In the first case there is no infection, in the second there is.
The results of ELISA analysis have three options - “negative”, “positive” or “doubtful”.
ELISA diagnostics determines the presence of antibodies.
Therefore, receiving a negative indicator may indicate the absence of a disease or an infection that occurred recently.
If a questionable result is obtained, a repeat test is scheduled a few weeks later.
When and what tests to take for ureaplasmosis
The peculiarity of ureaplasmosis is that it can be asymptomatic. That is why the infection is most often detected through laboratory testing. Examination of ureaplasmosis is done if there are compelling reasons for this: threat of miscarriage, before pelvic surgery, in case of infertility, miscarriage, etc.

This disease is detected using methods:
- serological method;
- PCR (polymerase chain reaction);
- bacterial culture;
- immunofluorescence reactions (RNIF, RPIF).
For a more accurate diagnosis, it is better to use several methods simultaneously. This will make it more likely that you have an infection. The most common and primarily prescribed are two test options:
- Bacterial culture.
It helps identify two types of virus (U. parvum and U. urealyticum) and determine the number, as well as their sensitivity to certain antibiotics. For analysis, a smear is taken (from the cervix, urethra or vagina) and a culture is done. - PCR analysis
, for which scrapings from mucous membranes or blood from a vein are used as the test material.
Diagnosis of ureaplasma
Indications for examination for Ureaplasma spp.
is the presence of clinical and laboratory signs of an inflammatory process in the area of the urogenital tract and reproductive system, vaginal dysbiosis in the absence of pathogenic pathogens.
I translate into Russian - if there are no complaints and no signs of inflammation in the genitourinary organs, there is no need to be examined for ureaplasma.
If there are complaints and signs of inflammation, then men are first examined for STIs (sexually transmitted infections - chlamydia, mycoplasma genitalium, gonorrhea, trichomonas), women - STIs, thrush, bacterial vaginosis, aerobic vaginitis. And if only after this examination it is not possible to identify the cause of the inflammation, then by the method of exclusion we can assume that this inflammation is caused precisely by ureaplasmas and suggest being examined for them.
In the absence of clinical and laboratory signs of the inflammatory process, the following are subject to examination:
- sperm donors
- patients diagnosed with infertility
- patients with a history of miscarriage and perinatal losses
Considering the difficulty of identifying the true causes of infertility and miscarriage, the wariness of doctors around the world in prescribing antibiotics in cases where there are no absolute indications for this, in this case I consider the prescribing of antibacterial drugs to be a greater evil than a benefit.
Preparation for analysis
For the serological diagnostic method, blood is taken from a vein on an empty stomach in the morning. Within 5-7 days, the titer of antibodies of various classes can be determined. To ensure that the test is accurate, it is not recommended to perform it while the patient is taking any medications. One or two days before the serological examination, you need to exclude fatty, “heavy” foods and alcohol from your diet.
For PCR diagnosis of ureaplasma, smears are taken from the vagina, urethra and cervical canal in women 2-3 days after the end of menstruation. Before taking material, it is not recommended to douche, use vaginal ointments or suppositories. Men can be examined no earlier than 3 hours after urination, so that the pathogen is not “washed away” along with the urine. Before the test, patients are advised to abstain from sexual activity for a day or two.
For bacteriological culture for ureaplasma, smears from women are taken from the vagina, cervical and urethra. In men, the urethral mucosa, prostate secretions and urine are examined. For the study, morning urine is taken in a volume of 40-50 ml. Before the examination, it is recommended to abstain from sexual relations and alcohol. In this case, not only the pathogen itself is identified, but its sensitivity to antibiotics is also determined.
Immunofluorescence reactions (RNIF, RPIF), in which smears from the genitourinary tract are also examined. Preparation for them is similar to that recommended for bacterial culture and PCR diagnostics.
Blood ELISA for ureaplasmosis
An enzyme immunoassay examines blood.
The presence of antibodies is detected.
This test shows whether the body has antibodies to fight ureaplasma.
In this case, microorganisms may be absent.
Therefore, it is used only in conjunction with PCR.
Separately, ELISA is not a diagnostic criterion for ureaplasmosis.
Based on the ELISA results, you can judge how severe the infection is: the more acute the disease, the higher the antibody titer.
It is important not to forget that antibodies are present in human blood even after the bacteria are destroyed.
Patients are often interested in the question: what does it mean when the antibody test is positive, but the PCR test is negative, or vice versa?
In the first case, ureaplasmosis was successfully treated.
Antibodies indicate that there was an infection, and PCR indicates that it is no longer there.
The opposite situation is possible when the bacterium is present, but the body has not yet developed protective antibodies to ureaplasma.
Decoding the analysis for ureaplasma
To diagnose ureaplasmosis, several types of tests are used: serological method, PCR (polymerase chain reaction), bacterial culture for ureaplasma, immunofluorescence reactions (RNIF, RPIF).
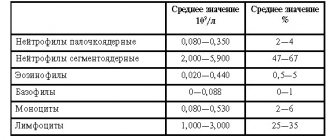
Interpretation of the results of serological examination
A serological examination of blood determines the presence of immunoglobulins in it. The decoding must indicate each of their types, as this is very important for diagnosis:
- The presence of class M antibodies
means that the disease is still in the development stage and a protective reaction to ureaplasma is being formed. - The detection of group G immunoglobulins
indicates that the infection has been present in the body for a long time. Sometimes a positive result can persist even after recovery. Sometimes the presence of G-antibodies indicates that the disease has already been cured, for example, when taking antibiotics for another disease.
In addition to the presence of immunoglobulins, the analysis also indicates their quantity. If the result is negative, there are no antibodies in the tests.
Explanation of PCR analysis
In this case, the result of the analysis indicates whether Ureaplasma urealiticum is detected. This method is very accurate, but it requires care and experience. If the test is performed incorrectly or low-quality reagents are used, the result may be false positive or false negative.
With a deeper localization of the pathogen (ovaries, uterus) or the use of antibiotics, the PRC study may not diagnose the presence of ureaplasma even if it is present.
Interpretation of bacterial culture results
The material is sown in a nutrient medium, and the maximum concentration of microorganisms should not exceed 10*4 CFU/1 ml. (ureaplasma 10 to 4 degrees is the norm). This type of research also makes it possible to identify pathogen resistance to antibiotics. Which antibiotic will help with ureaplasma is indicated in the result. But the name of a group of antibiotics is not a medicine yet! The doctor will prescribe the drug for ureaplasma, and he will also take into account other types of pathogens that are found together with ureaplasma.
Decoding the results of RNIF, RPIF
Direct and indirect immunofluorescence reactions are positive and negative. In the first case, the pathogen is present in the body, and in the second, it is absent. In doubtful cases, it is recommended to conduct several types of studies - this will give more accurate results.
Mycoplasma/ureaplasma: diagnostic methods
Mycoplasmas are the smallest known bacteria. Their life depends on the cells of the organism in which they live. Certain methods can be used to diagnose mycoplasma infection.
Methods for diagnosing infections
There are direct and indirect methods for diagnosing infections. Direct methods make it possible to identify the infectious agent in the material. These include PCR, bacteriological examination, microscopy and others. Indirect ones include the determination of antibodies in the blood (that is, the determination not of the infectious agent itself, but of the immune response to it), identification of biochemical markers, etc. For each infection there is its own diagnostic standard.
Ureaplasma
Ureaplasma are representatives of the class Mollicutes, family Mycoplasmataceae. The family includes several genera, including the genus Ureaplasma and the genus Mycoplasma. Thus, several types of genital mycoplasmas can be distinguished: U. Urealyticum (biovar 2, includes several serotypes - 2, 4, 5, 7, 8, 9, 10, 11, 12, 13), U. Parvum (biovar 1 , includes several serotypes - 1, 3, 6, 14), M. hominis and M. Genitalium. Read more: Taxonomy Browser
See also “Changing ideas about ureaplasmas.”
No other group of prokaryotes has been involved in as much controversy and debate as this one. Even with growing evidence of their infectious and pathogenic potential, mycoplasmas still appear to be a group of mysterious microorganisms. However, they are evolutionarily advanced prokaryotes and their elite status as “next generation” bacterial pathogens requires new paradigms to fully understand their pathogenic potential.
Mycoplasmas are the smallest known bacteria. Mycoplasmas are descendants of gram-positive bacteria, which in the process of evolution have reduced their genome and lost their cell wall. The absence of a rigid cell wall allows them to pass through the smallest holes and be resistant to antibiotics that act on the cell wall. The mycoplasma genome is an example of extreme biological economy. The absence of many important genes leads to the fact that mycoplasmas lead a parasitic lifestyle; they are dependent on the supply of substances such as amino acids, nucleotides, fatty acids, and so on. Their life depends on the cells of the organism in which they live.
Ureaplasma is transmitted primarily through sexual contact. The infection rate of sexually active women reaches 60-80. Ureaplasma often does not cause disease, but its presence is important for pregnant women and women planning pregnancy, for newborns, as well as in the presence of a clinical picture of the disease.
The main methods for detecting ureaplasma are direct. Determination of antibodies to ureaplasma is practically not used.
PCR: a fast method with high sensitivity and 100% specificity*, the ability to determine the type of ureaplasma. Ureaplasma typing is important, since each type has its own clinical significance. In addition, during PCR diagnostics, unlike culture, not only living but also dead microorganisms are determined. * 100% specificity means that if the result is positive, then ureaplasma is present in the sample. High sensitivity means that with a minimum amount of ureaplasma in the sample, they can be determined by this method.
Bacteriological research (cultural method, isolation of ureaplasma culture) is a less sensitive method; it does not allow determining the type of ureaplasma; in addition, the test is carried out longer than PCR. The structural and physiological features of ureaplasmas, which are described above, make the analysis quite difficult: mycoplasmas are very capricious, they are difficult to cultivate, they require special media, and they do not tolerate transportation well. Even under ideal conditions in a scientific laboratory, sensitivity does not reach high numbers (up to 50%), specificity could reach 100% if there were no subjectivity factor in the evaluation of microbiological preparations. M.genitalium is more difficult to cultivate than other mycoplasmas; it grows very slowly on nutrient media, so cultures are not used in clinical practice.
Sensitivity Comparison: Brief Full Article
The advantages of the bacteriological method include determining the titer of ureaplasma and the ability to determine sensitivity to antibiotics. Let's try to understand these theses. Recommendations regarding the prescription of treatment (“Interdisciplinary Russian consensus on genital mycoplasmas” (2006)) include the prescription of treatment when the ureaplasma titer is more than 10^4 CFU/ml (the figure obtained as a result of bacteriological examination). It is assumed that the resulting titer corresponds to the content of ureaplasma in the body. In reality, during a bacteriological study, the amount in the collected material is determined, and this is not the same as the amount in the vagina. This depends on the quality of the scraping, the amount of mucus, and many other factors. In addition, the concentration of ureaplasma changes during the menstrual cycle, depends on the use of medications, etc. Therefore, quantitative analysis for ureaplasma is a rather conditional method and its result should not be the basis for prescribing or not prescribing treatment.
Cultures with sensitivity determination (resistogram) are used only for scientific purposes to develop optimal principles for the treatment of microbial associations. This is due to the fact that mycoplasmas are difficult to cultivate microorganisms that do not tolerate transportation well and require special conditions for cultivation. Another problem is the very slow reproduction of some mycoplasmas in culture (for example, M. genitalium). Determining sensitivity to antibiotics in vitro does not reflect the real situation of sensitivity or resistance of the entire microbial association to antibiotics in vivo, and therefore cannot be a research method on the basis of which treatment will be prescribed.
When to conduct the examination?
Ureaplasma sows dissent between physician brothers
Indications for examination for mycoplasma (ureaplasma):
- Preparing for pregnancy
- Pregnancy
- Presence of symptoms of inflammatory diseases of the pelvic organs (urethritis, colpitis, etc.)
- Presence of symptoms of bacterial vaginosis
- Changes in the results of additional examination methods (see below)
- Infertility, miscarriage, pregnancy complications
- Identification of an infectious agent in a partner
Considering the significance of mycoplasmas in the development of inflammatory processes of the genitourinary organs in men and women, the risks associated with the role of colpitis and bakvaginosis in the development of premature rupture of water and some other complications of pregnancy, the preferred method of examination is PCR.
In Western recommendations, if there are signs of inflammatory diseases of the pelvic organs or bacterial vaginosis, the following tests are recommended: microscopy of discharge (gynecological smear in women or smear from the urethra in men), smears to detect gonococci, trichomonas, chlamydia. We recommend more sensitive PCR diagnostics of these infections. With obvious clinical symptoms of an inflammatory disease in the absence of gonococci, trichomonas and chlamydia, they speak of so-called non-chlamydial non-gonococcal urethritis and other inflammatory processes. Isolation of non-chlamydial, non-gonococcal inflammatory processes is very important clinically, as it highlights the importance of microbial associations in the development of inflammation. It can be very difficult to isolate separately the role of each microorganism in the development of the inflammatory process. General treatment of bacterial vaginosis results in a significant reduction in populations of potentially pathogenic microbes. Therefore, in case of microbial associations involving mycoplasmas, significant improvement often occurs with the use of drugs metronidazole or clindamycin, which do not directly act on mycoplasmas, but eliminate the conditions for the favorable survival of mycoplasmas in the body.
“To treat or not to treat?”
Treatment for a positive result of PCR (ureaplasma positivity) or bacteriological examination (culture) is not always necessary. In the first place should be the degree of clinical manifestations of the inflammatory process and the clinical context (for example, pregnancy, the presence of pelvic inflammatory process activity, discharge, symptoms of urethritis, etc.). The main indications for treatment are the following cases of detection of ureaplasma:
- Infection caused by ureaplasma (signs of urogenital infection without identifying other agents that could cause the disease).
- Pregnancy
- Planning surgeries on the genitourinary system
For each case, the need for treatment should be assessed by the attending physician. The decision on treatment is made based on an assessment of the clinical picture and a set of examination data. Treatment is prescribed not on the basis of a resistogram, but on the basis of recommendations for the treatment of non-gonococcal, non-chlamydial inflammatory processes caused by microbial associations involving mycoplasmas. The Center for Immunology and Reproduction regularly monitors publications devoted to the study of the sensitivity of such microbial associations to antibacterial drugs and uses this data in its practice. Due to the resistance of microorganisms to antibiotics and the strong dependence on the general condition of the microflora, it is not always possible to achieve eradication of microorganisms even when prescribing modern treatment regimens. Too persistent treatment of mycoplasmas can lead to treatment complications.
Testing using the PCR method + additional examination + consultation with a gynecologist
Appendix: Diagnosis of urogenital infections
| In men | Among women |
| External examination, palpation | External examination, palpation |
| Microscopy of a smear from the urethra, microscopy of prostate juice | Microscopy of a gynecological smear |
| (during microscopy, mycoplasma/ureaplasma cannot be seen due to their small size, but microscopy allows one to assess the number of leukocytes and, in some cases, identify bacteria). | |
| General urine analysis | General urine analysis |
| Spermogram | |
| Ultrasound examination of the prostate and scrotal organs | Ultrasound examination of the pelvic organs |
Diagnosis of urogenital infections using PCR, including identifying:
| Diagnosis of urogenital infections using PCR, including identifying:
|
Back to section
Features of treatment of ureaplasmosis according to test results
Based on the test results, the doctor makes conclusions about prescribing medications. If ureaplasma is not detected or is present at an acceptable level, no treatment is required. If the permissible values are exceeded, based on research, the doctor prescribes those antibiotics that are most suitable for a given type of ureaplasma and associated infections - there is rarely one ureaplasmosis. Along with ureaplasma, chlamydia, gonococci and trichomonas, mycoplasma, gardnerella, human papillomavirus (HPV) and genital herpes are detected.
Treatment for ureaplasmosis is carried out for both partners if they are infected. During this period, you should avoid sexual contact or use a condom. In addition to antibiotics, drugs that enhance immunity and physical therapy are used. To prevent relapses, you need to eat right, normalize body weight, follow a daily routine, harden yourself, and be physically active.
What is ureaplasmosis?
However, if the body's immunity weakens, ureaplasma can cause painful manifestations.
When the bacterium is able to multiply uncontrollably, it causes inflammation of the tissues and organs of the urinary system.
This can happen in the background:
- infectious diseases,
- exacerbations of chronic diseases,
- immunodeficiency conditions,
- dysbacteriosis, especially local,
- hypovitaminosis,
- hypothermia.
In this case, a person develops a disease such as ureaplasmosis.
To date, the diagnosis of “ureaplasmosis”, as such, is absent in ICD-10.
Ureaplasma is not considered a pathogenic microorganism.
The disease is considered a consequence of dysbiosis.
Symptoms of the pathology are similar to those of many diseases of the genitourinary system:
- itching in the genital area,
- burning and discomfort when urinating,
- pathological discharge from the genitals, sometimes with a pungent odor,
- pain and discomfort during sexual intercourse,
- increase in body temperature,
- feeling of weakness due to intoxication of the body.
However, hyperthermia and intoxication are relatively rare.
Such symptoms usually indicate the transition of inflammation to the upper parts of the urinary system.
Due to the absence of specific signs of inflammation, an accurate diagnosis is made based on test results.
Treatment of ureaplasmosis
If ureaplasma is detected, treatment is carried out if the microbe is the cause of chronic inflammation, infertility, etc. If the cause of the disease is ureplasma, treatment is prescribed with antibiotics. The choice of antibiotic should be made by a doctor, since self-medication of ureaplasmosis often not only does not bring the desired result, but can also lead to the development of microbial resistance to the antibiotic. Thus, over the past few years, the number of tetracycline-resistant strains of Ureaplasma urealyticum and parvum has been increasing.
Of particular importance is the treatment of ureaplasma (parvum, urealiticum) in men and women when planning pregnancy. The decision to treat ureaplasma parvum and others during pregnancy is made taking into account its duration, as well as after carefully weighing the possible risks for the child and mother from ureaplasma and antibiotic therapy. Usually, they try to treat ureaplasma during pregnancy at a later stage (after 20 weeks), when the effect of antibiotics on fetal development becomes minimal.