Introduction
Lung cancer annually affects more than 63,000 Russians, 53,000 of whom are men. Many people believe that their disease is caused by smoking. The truth is that most smokers do not develop lung cancer, and not all people who are diagnosed with lung cancer smoke. Lung cancer is a disease that can affect anyone. A malignant tumor is always treatable, regardless of its size, location, metastasis and degree of spread.
Functionality of the lungs and their structure
When a person inhales air, the lungs absorb oxygen and deliver it to the bloodstream for transport to other organs and systems. When cells in the body absorb oxygen, they release carbon dioxide. The bloodstream carries it back to the lungs. Carbon dioxide leaves the body when you exhale. The lungs contain different types of cells. Most of them are epithelial cells. They line the airways and produce mucus that lubricates and protects lung tissue. The lung also contains nerve, hormone-producing, blood, and structural or supporting cells.
Non-small cell lung cancer
There are 2 main types of lung cancer: small cell lung cancer and non-small cell lung cancer (NSCLC). These 2 types require different treatment.
NSCLC begins when healthy cells change and begin to grow uncontrollably, forming a mass called a tumor, lesion, or nodule. A lung tumor can form anywhere in the lung tissue. The tumor can be cancerous or benign. As it grows, it begins to produce cells. They are carried in the blood or in the fluid called lymph that surrounds the lung tissue. Lymph flows through tubes (lymphatic vessels) and enters places where lymph accumulates (lymph nodes). Lymph nodes are small, bean-shaped organs that help fight infections. They are located in different parts of the body (including the lungs and the sternum area). The natural drainage of lymph from the lungs is directed to the center of the chest, which is why lung cancer often spreads there first. The process by which a cancer cell travels to a lymph node or distant part of the body through the bloodstream is called metastasis.
Types of NSCLC
NSCLC begins in epithelial cells. NSCLC can be classified based on the type of epithelial cell that is the ancestor of the cancer process:
- Adenocarcinoma begins in cells that secrete mucus.
- Squamous cell carcinoma begins in the cells lining the airways.
- Large cell cancer begins in other types of cells.
To determine treatment options, it is important for your doctor to distinguish lung cancer that starts in squamous cells from lung cancer that starts in other cells.
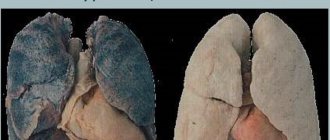
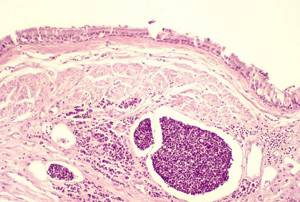
Normal lung tissue
Lung: adenocarcinoma
Lung: squamous cell carcinoma
Pain after recovery
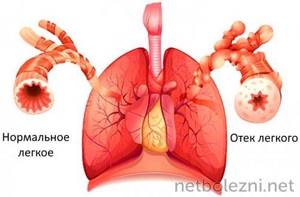
When a person is sick with a coronavirus infection that causes pneumonia, his lungs are affected. If a prolonged inflammatory process occurs, normal alveolar tissue is replaced by scar tissue. This complicates the functionality of the respiratory tract and increases the risk of relapse of covid-19 or infection with other viruses.
There can be a lot of scarring on the lungs. This causes discomfort to patients. They describe the condition as follows:
- difficulty inhaling, it is impossible to take a deep breath;
- feeling of lack of air with minor viral infections;
- a decrease in the number of red blood cells and hemoglobin in the blood, which leads to pallor and lethargy of the patient.
If a person does not have a new viral pathology, the coronavirus has completely receded, and no pain in the chest should appear. Normal health occurs even in patients who have acquired multiple scars on the lungs. They do not contain nerve fibers, so no pain impulses are sent to the central nervous system.
If the patient repeatedly describes discomfort in the chest, this is a reason to see a pulmonologist. It is better to undergo additional X-ray or CT examination to eliminate the risk of complications. In addition to coronavirus, there are many diseases that need to be detected in a timely manner.
Risk factors and prevention of non-small cell lung cancer
A risk factor is anything that increases the likelihood of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause cancer. Knowing your risk factors and discussing them with your doctor can help you make more informed lifestyle and health care choices. NSCLC most often occurs in former or current smokers. However, non-smokers may also be at risk.
The following factors may increase your risk of developing NSCLC:
- Tobacco and smoking. Tobacco smoke damages lung cells, causing them to grow abnormally. The risk that smoking will lead to cancer is higher among long-time, heavy smokers. Regular exposure to smoke from other people's cigarettes, cigars, or pipes can increase the risk of disease, even for a non-smoker. This is called exposure to environmental tobacco smoke, or secondhand smoke. Smoking marijuana and e-cigarettes also increases the risk of developing cancer.
- Asbestos . The hair-like crystals found in many types of rocks are often used as fire-retardant insulation in buildings. Inhalation of asbestos fibers causes lung irritation. Many studies show that the combination of smoking and asbestos exposure is especially dangerous. Smokers whose jobs involve asbestos in fields such as shipbuilding, asbestos mining, insulation, or automobile brake repair have a higher risk of developing NSCLC. Using respiratory protection reduces this risk.
- Radon. A colorless, odorless gas released from some types of soil and rocks. Exposure to radon is associated with an increased risk of developing cancer.
- Other substances. Other substances, such as gases or chemicals at work or in the environment, can increase the risk of developing cancer. Lung cancer is also caused by radiation, arsenic, nickel and chromium.
- Genetic factors . Some people have a genetic predisposition to lung cancer, especially those with a strong family history.
Prevention
The main way to prevent lung cancer is to quit smoking. Non-smokers have the lowest risk of developing a tumor. People who quit tobacco are less likely to get sick, but they will still be more likely to get sick than those who have never smoked.
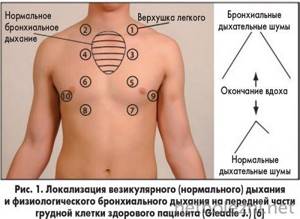
How to properly perform topographic percussion?
The pessimeter finger is installed at the point from which the study begins (for example, when determining the upper border of the lung along the anterior surface, it begins above the middle part of the clavicle), and then moves to the point where approximately this measurement should end. The border is determined in the area where the pulmonary percussion sound becomes dull.

For ease of research, the pessimeter finger should lie parallel to the desired boundary. The displacement step is approximately 1 cm. Topographic percussion, unlike comparative, is performed by gentle (quiet) tapping.
Follow-up and control
Treatment for people diagnosed with cancer does not end when active therapy is completed. Your doctors will continue to check to see if the cancer has returned, monitor any side effects, and monitor your overall health. This is called follow-up.
Follow-up care may include regular medical examinations and tests. Doctors want to track your recovery over the coming months and years.

One of the goals of follow-up is to monitor recurrence, that is, the return of cancer. The tumor recurs due to the fact that a small number of malignant cells may remain in the body. Over time, these cells may increase in size until they appear in test results or cause signs or symptoms. During follow-up, a doctor familiar with your medical history can provide you with personalized information about your risk of recurrence. Your doctor will ask specific questions about your health. Some may need to have blood tests or imaging tests as part of routine follow-up, but follow-up recommendations depend on several factors, including the type and stage of the disease initially diagnosed and the type of treatment received.
Monitoring long-term and delayed side effects
Most experience side effects during treatment. If unpleasant consequences persist after cancer therapy, they are called long-term. Delayed side effects occur months or even years later. Long-term and delayed effects may include physical and emotional changes.
Common problems after treatment include pain, fatigue, and shortness of breath. Your doctor will work with you to develop a plan to address any problems that continue after treatment.
Patients who have overcome NSCLC and have a history of smoking cigarettes also have a high risk of developing heart disease, stroke, emphysema and chronic bronchitis. Certain cancer treatments may further increase these risks. Even for those who don't smoke, making healthy lifestyle choices after illness is important for overall well-being.
Maintaining your own medical records
You and your doctor will work together to develop a personalized follow-up plan. Be sure to discuss any concerns you have about your future physical or emotional health.
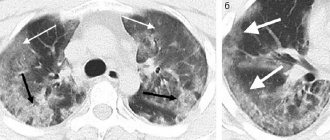
Pain due to complications
Pneumonia has dangerous complications. One of the typical manifestations is discoid atelectasis. This is a pathology in which one or more parts of the lungs decrease in volume. On radiography this is manifested by the following signs:
- darkening the area;
- formation of a long horizontal stripe;

- localization above the diaphragm;
- passes to the cortical parts of the lungs.
This pathology leads to changes in lung volume, causing decreased inhalation and exhalation. Other complications may also develop. They are formed during a prolonged inflammatory process. The following deviations are difficult to tolerate:
- infiltration of the diaphragm;
- blockage of a pulmonary vessel with necrosis of part of the organ;
- pulmonary edema;
- hypertrophy of the dome.
In these conditions, the pain syndrome not only persists, but can also intensify. The doctor is told about this in order to adjust the treatment. Many patients are placed on a ventilator.
To monitor the patient’s condition during treatment for severe pneumonia, it is recommended to repeat x-rays and other tests.
In some patients, complications may go away soreness. This is also a dangerous symptom, indicating tissue necrosis. For example, if a lung infarction occurs, some of the small nerve fibers die.

Stages of NSCLC
Staging is a determination of where the cancer is located, whether and where it has spread, and its effect on other parts of the body.
Doctors use diagnostic tests to determine the stage of cancer; they may need information based on tissue samples obtained at surgery, so staging may continue until all studies are completed. Information about the stage helps the doctor determine which treatment is optimal and predict the possibility of recovery. For different types of oncological process, there are different descriptions of stages.
In general, the lower the NSCLC stage sequence number, the better the outcome. However, no doctor can predict how long a patient will live with lung cancer based solely on the stage of the disease. This is due to the fact that the disease progresses differently, and treatment affects each tumor individually.
Classification of cancer stages
NSCLC staging is based on a combination of several factors, including:
- Tumor size and location
- Whether the tumor has spread to the lymph nodes and/or other parts of the body. There are 5 stages of NSCLC: stage 0 (zero) and stages I to IV (1 to 4). One way to determine the stage of NSCLC is to see if a surgeon can completely remove the cancer. To completely eliminate the tumor, it is necessary to excise it along with the surrounding healthy tissue.
Stage 0
This is called in situ disease, which means the cancer is "in place"; did not grow into adjacent tissues and did not spread beyond the lung.
Stage I
Stage I lung cancer is a small tumor that has not metastasized to the lymph nodes, allowing the surgeon to completely remove it. Stage I is divided into 2 substages depending on the size of the tumor:
- Stage IA tumors are no larger than 3 cm. Stage IA tumors are classified as IA1, IA2 or IA3 depending on the size of the tumor.
- Stage IB tumors 3-4 cm.
Stage II
Stage II lung cancer is divided into 2 substages:
- Stage IIA cancer is a tumor measuring 4-5 cm, without metastatic spread.
- Stage IIB lung cancer is a tumor (5 cm or larger) that has spread to the lymph nodes. Stage IIB cancer is an oncological process that has metastasized to the lymph nodes. Sometimes stage II tumors can be removed surgically; in other cases, more procedures are required.
Stage III
Stage III lung cancer is divided into stages IIIA, IIIB or IIIC. Staging is based on the size of the tumor and which lymph nodes the cancer has spread to. This type of cancer does not metastasize to other distant parts of the body.
In most cases in stage IIIA and almost always in stage IIIB, the tumor is difficult and sometimes impossible to remove surgically.
Stage IV
Stage IV means the cancer has metastasized to more than 1 area in another lung, the fluid surrounding the lung or heart, or distant parts of the body through the bloodstream. Once tumor cells enter the bloodstream, cancer can spread to any part of the body. NSCLC most often metastasizes to the brain, bones, liver, and adrenal glands. Stage IV NSCLC is divided into 2 substages:
- Stage IVA cancer - has spread to the chest and/or 1 area outside the chest.
- Stage IVB cancer - has spread beyond the chest to more than 1 site in 1 organ or in more than 1 organ.
In general, surgery is not successful in most stage III or IV cases. The tumor also cannot be removed if it has metastasized to the lymph nodes above the collarbone or has grown into vital organs in the chest (the heart, major blood vessels, or the main trachea leading to the lungs). In these situations, your doctor will recommend other treatment options.
NSCLC relapse
Cancer recurrence is the return of the disease after treatment. In case of relapse, additional research methods will help determine the extent of the disease. These tests are usually the same as those used for the initial diagnosis.
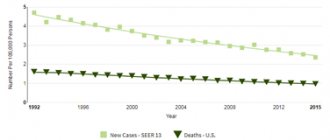
Forecasts
Although NSCLC is treatable at any stage, at some stages only a few patients can be cured.
Doctors measure a patient's overall strength and health using a general condition score. Patients who are strong enough to carry out activities of daily living without assistance and work outside the home can safely receive chemotherapy, radiation therapy, and/or surgery. Treatment may not be as effective for patients who have bone or liver metastases, have excessive weight loss, continue to smoke, or have chronic conditions such as heart failure or emphysema.
The patient's age should never be used as the sole reason for a treatment modality, especially for older patients who are otherwise in good physical condition and have no medical problems other than the underlying disease.
How long does the pain last?
When the inflammatory process caused by coronavirus begins, it is impossible to say with certainty how long the negative symptoms will last. It all depends on the degree of activity of the immune system. If it is sufficiently developed, the influence of the pathogenic microorganism is suppressed quickly, so recovery is observed in a short time. The condition rarely leads to complications. Even with the development of pneumonia, when there is pain in the chest.
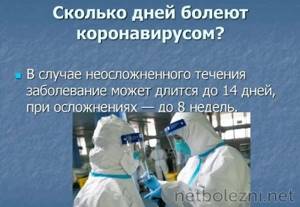
With moderate severity, it takes 2-3 weeks to recover. The time depends on the functional capabilities of the body and the activity of the doctor. If the patient takes prescribed medications in a timely manner, performs inhalations, and undergoes physical procedures, recovery will occur faster. This will reduce the risk of fibrosis and other complications for the lungs, so the pain syndrome will be minor and will pass quickly.
The disease is more severe for patients with chronic diseases of the respiratory and cardiovascular systems. Chest pain can occur not only due to pneumonia, but also due to heart failure, bronchial asthma, bronchospasm, and heart attack. Therefore, it is impossible to do without differential diagnosis of pain symptoms.
Symptoms of non-small cell lung cancer
Sometimes patients with NSCLC do not notice any changes in their health. Patients with NSCLC may experience the following symptoms;
- fatigue
- cough
- dyspnea
- chest pain if the tumor spreads to the mucous membrane or other parts of the body near the lungs
- loss of appetite
- coughing up phlegm or mucus
- blood when coughing
- unexplained weight loss
- hoarseness
In many cases, the cause of complaints may be non-oncological conditions. If you are concerned about any changes in your body, contact your doctor. It will ask, among other things, how long and how often you have been experiencing the symptom(s). This conversation will help determine the cause of the problem, establishing the correct diagnosis.
In patients with NSCLC who do not have any symptoms, the cancer may be seen on a chest X-ray or CT scan done for any other reason, such as a heart test. In most people, NSCLC is diagnosed when the tumor grows, takes up space, or causes discomfort to organs near the lungs. The tumor can secrete fluid that accumulates in the lung or the space around it and causes the lung to collapse. This prevents oxygen from entering the body and carbon dioxide from leaving the body, blocking the flow of air into the lungs and taking up space normally needed for oxygen to enter and carbon dioxide to leave the lungs.
NSCLC can spread anywhere in the body through a process called metastasis. It most often spreads to the lymph nodes, bones, brain, liver, and structures near the kidneys called the adrenal glands. NSCLC metastases can cause:
- additional breathing difficulties;
- bone pain;
- abdominal or back pain;
- headache;
- weakness;
- convulsions;
- speech difficulties;
- Rarely, a lung tumor may release hormones that cause problems such as low blood sodium levels or high blood calcium levels.
Once cancer is diagnosed, symptom relief remains an important part of cancer care. This is palliative or supportive care. It often begins soon after diagnosis and continues throughout treatment.
Signs of recovery
If coronavirus infection is gradually eliminated from the body, this is evidenced by disappearing symptoms. This does not happen immediately, since toxic metabolites of the virus remain in the blood for a long time. The following symptoms are being eliminated every day:
- body temperature drops instantly, one day it can reach 39 degrees, the next it drops to 36.6 degrees;
- the sense of smell and taste gradually returns (within 5-14 days);
- copious amounts of green sputum cease to be released, it becomes transparent, and then disappears altogether;
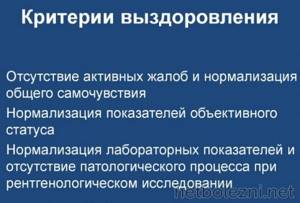
- the cough continues for at least 1 month after the end of the illness, irritation of the trachea is not eliminated immediately;
- pain behind the sternum can also be long-lasting, since the pneumonia has resolved, the inflammatory process in the bronchial tree can last a long time;
- breathing becomes smooth, its frequency decreases to normal, and attacks of suffocation are completely absent.
Breathing becomes normal immediately after eliminating the inflammatory process in the bronchi and lungs. This is the main sign indicating a gradual recovery.
Other symptoms may persist even after complete recovery for a long time. For example, cough and sputum production. You should not put your health at risk - adhere to prolonged bed rest, use medications prescribed by a pulmonologist.
Treatment methods for non-small cell lung cancer
“Standard of care” means the best known methods of treatment. When deciding on a treatment plan, you are encouraged to consider clinical trials as an option. This type of research helps to analyze a new approach to treatment. It is an option for cancer care at all stages of cancer. Clinical trials may test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments.
Treatment Overview
When treating cancer, different doctors often work together to create a unifying treatment plan for the patient. This is called an interdisciplinary team. Oncology care teams include a variety of other health care professionals, such as physician assistants, oncology nurses, social workers, counselors, dietitians, and other specialists.
There are 5 main treatments for NSCLC:
- Surgical intervention
- Radiation therapy
- Chemotherapy
- Targeted therapy
- Immunotherapy
Surgical intervention
An oncologist surgeon is a doctor who specializes in the treatment of oncology using surgical methods. A thoracic surgeon is specially trained to perform surgery to treat lung cancer. The goal of the operation is to completely remove the lung tumor and nearby lymph nodes in the chest. The tumor is removed along with surrounding healthy tissue. A "negative margin" means that when the histologist examined the lung or a piece of lung removed by the surgeon, no cancer was found in the healthy tissue surrounding the tumor.
The following types of surgery may be used for NSCLC:
- Lobectomy . The lungs consist of 5 lobes, 3 in the right lung and 2 in the left lung. A lobectomy is the removal of an entire lobe of the lung. Currently, this method is considered the most effective, even when the tumor is very small.
- Wedge resection. If the surgeon cannot remove an entire lobe, the tumor surrounded by the edge of a healthy lung can be removed.
- Segmentectomy . This is another way to remove a tumor when it is impossible to remove an entire lobe. In a segmentectomy, the surgeon removes the part of the lung where cancer has developed.
- Pneumonectomy . If the tumor is close to the center of the chest, the surgeon may have to remove the entire organ.
The time required to recover from surgery depends on how much of the lung is removed and the patient's condition before surgery.
Adjuvant therapy
Adjuvant therapy is treatment given after surgery. It is designed to remove tumor cells that may remain in the body after surgery. This helps reduce the risk of relapse.
Adjuvant therapy for NSCLC includes radiation therapy and systemic therapy, such as chemotherapy, targeted therapy, and immunotherapy.
Radiation therapy
Radiation therapy (radiotherapy) is the use of high-energy X-rays or other particles to destroy cancer cells. A doctor who specializes in administering radiation therapy is called a radiation oncologist. The most common type of radiotherapy is called external beam radiotherapy, which is radiation emitted from a machine outside the body. A radiation therapy regimen, or regimen, consists of a specific number of treatments given over a period of time. It can range from several days to several weeks.
Like surgery, radiotherapy cannot be used to treat advanced cancer. It destroys only cancer cells directly in the path of the radiation beam, also damaging healthy cells along the way. For this reason, it cannot be used to treat large areas of the body.
Sometimes a CT scan is used to precisely plan the direction of radiation to reduce the risk of damage to healthy parts of the body. This is called intensity modulated radiation therapy (IMRT) or stereotactic radiotherapy (SBRT). This option is not suitable for everyone, but may be used in patients with early stage disease and small tumors when surgery is not an option.
Side effects of radiation therapy
People with lung cancer who receive radiation therapy often experience fatigue and loss of appetite. If the radiation is aimed at the neck or center of the chest, side effects may include a sore throat and difficulty swallowing. Patients may also notice skin irritation, similar to a sunburn, in the area where the beam was directed. Most side effects disappear soon after treatment ends.
When radiation therapy affects the lungs, patients develop a cough, fever, or shortness of breath months and sometimes years after radiation treatment ends. Approximately 15% of patients develop this condition (radiation pneumonitis). If it is mild, it does not require treatment and goes away on its own. If pneumonitis is severe, the patient will require treatment with steroid drugs (prednisolone). Radiation therapy can also cause permanent scarring of lung tissue near the site of the primary tumor. Scarring usually does not cause symptoms, but large scars may cause persistent coughing and shortness of breath. For this reason, radiation oncologists carefully plan treatment using chest CT scans to reduce the amount of healthy lung tissue exposed to radiation.
Drug therapy
Systemic therapy is the use of medications to kill cancer cells. Such drugs are administered through the bloodstream to reach cancer cells throughout the body. Systemic therapy is usually prescribed by a chemotherapy physician who specializes in treating cancer with drugs.
Common systemic treatments include inserting an intravenous (IV) catheter into a vein using a needle or swallowing (oral) tablets or capsules.
The following types of systemic therapy are used for NSCLC:
- Chemotherapy
- Targeted therapy
- Immunotherapy
Each of these types is described in more detail below. A person can receive 1 type of systemic therapy or a combination of several types at the same time. They may also be part of a treatment plan that includes surgery and/or radiation therapy.
Drugs used to treat cancer are constantly being evaluated. The best way to get information about the medications you are prescribed, what they do, and possible side effects or interactions with other medications is to talk to your doctor.
Chemotherapy
Chemotherapy is the use of drugs that destroy cancer cells, preventing them from growing, dividing, or producing new cells. It has been shown to improve the length and quality of life of people with lung cancer at all stages.
A chemotherapy regimen or regimen usually consists of a certain number of cycles given over a period of time. The drugs used in chemotherapy depend on the type of tumor: adenocarcinoma or squamous cell carcinoma.
Typically, lung cancer is treated with 2 or 3 drugs given together, or 1 drug given separately.
Chemotherapy can also damage healthy cells in the body, including blood cells, skin cells, and nerve cells. Side effects of treatment depend on individual tolerance and the dose used and in most cases include fatigue, decreased red blood cell counts, risk of infection, mouth ulcers, nausea and vomiting, loss of appetite, diarrhea, numbness and tingling in the arms and legs, and hair loss. Your chemotherapy doctor may prescribe medications to reverse many of the negative effects of your treatment.
Targeted therapy
Targeted therapy is a treatment that targets specific genes, proteins, or tissue environments of cancer that promote tumor growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may do tests to identify genes, proteins, and other factors in the tumor. This helps doctors, whenever possible, select the most effective treatment for each patient.
Targeted therapy for NSCLC includes:
Antiangiogenic therapy. It is aimed at stopping angiogenesis, that is, the process of creating new blood vessels. To grow and spread, a tumor needs nutrients supplied through the blood vessels, so the goal of therapy is to “deplete” the tumor.
Epidermal growth factor receptor (EGFR) inhibitors . Research has shown that drugs that block EGFR may help stop or slow the growth of lung cancer. Drugs that target other genetic changes . Research has shown that targeting other genetic changes in lung tumors may help stop or slow the growth of NSCLC. This includes:
- Anaplastic lymphoma kinase (ALK) inhibitors. Mutations in the ALK gene are found in approximately 5% of patients with NSCLC.
- Drugs that target changes in a gene called ROS1.
- A certain genetic change called an NTRK fusion. This type of genetic change occurs in a number of cancers, including lung cancer.
Immunotherapy
Immunotherapy, also called biological therapy, is designed to enhance the body's natural defenses against cancer. It uses substances produced by the body or produced in a laboratory to improve, direct, or restore immune system function.
For most patients with advanced NSCLC who are not eligible for targeted therapy (see above), immunotherapy or its combination with chemotherapy is often the preferred primary treatment.
Different types of immunotherapy may cause different side effects. For example, skin reactions, flu-like symptoms, diarrhea and weight changes.
Physical, emotional and social consequences of cancer
Cancer and its treatment provoke not only side symptoms, but also emotional, social, and financial consequences. Managing all of these effects is called palliative or supportive care.
Palliative care aims to improve your well-being during treatment by managing symptoms and supporting the non-medical needs of patients and their families. Anyone, regardless of age, type or stage of cancer, can receive such care. It is most effective when started immediately after cancer diagnosis. Palliative care comes in a variety of forms and often includes medications, dietary changes, relaxation techniques, emotional and spiritual support, and other treatments. In some cases, chemotherapy, surgery, or radiation therapy are considered palliative options.
The following treatments are suitable to relieve symptoms of NSCLC:
- A tumor in the chest that is bleeding or blocking the airway may be reduced with radiation therapy.
- Bronchoscopy can be used to open airways blocked by tumors to make breathing easier.
- The surgeon may place a stent to keep the airway open or use a laser to burn out the tumor.
- Special medications are used to treat cancer pain. Most hospitals and cancer centers have pain management specialists who provide pain relief even for severe pain.
- Special medications may be used to stop coughing, open the airways, or reduce bronchial secretions.
- Prednisone or methylprednisolone reduces inflammation caused by lung cancer or radiation therapy and makes breathing easier.
- Supplemental oxygen from small portable tanks can help compensate for respiratory failure.
- There are medications available to strengthen bones, reduce pain, and prevent future bone metastases.
- Appetite stimulants and dietary supplements can improve appetite and reduce weight loss.
Treatment of NSCLC at different stages
Stage I and II NSCLC
Generally speaking, stages I and II NSCLC are treated with surgery. The patient may need to meet with a chemotherapy provider before and after surgery. A course of treatment may be given before surgery, called neoadjuvant, or induction, chemotherapy. It may also be given after surgery to reduce the chance of cancer coming back, called adjuvant chemotherapy.
Stage III NSCLC
More than 30,000 people are diagnosed with stage III NSCLC each year, and there is no single optimal treatment for all of these patients. Treatment options depend on the size and location of the tumor and the lymph nodes involved. The following options exist:
- Radiation therapy
- Chemotherapy
- Immunotherapy
- Surgical intervention
In general, people with stage III NSCLC receive 3 different types of treatment. A combination of chemotherapy and radiation therapy followed by immunotherapy is usually recommended for unresectable NSCLC. Chemotherapy and radiotherapy can be given together, this is called concurrent chemoradiotherapy. Or they may be given sequentially (sequential chemoradiotherapy).
Surgery may be appropriate after initial chemotherapy or chemotherapy with radiation therapy. Sometimes surgery may be the first treatment option, especially when cancer is unexpectedly found in the lymph nodes after a person was initially diagnosed with stage I or II cancer. In this case, surgery is usually accompanied by chemotherapy and often radiotherapy.
Metastatic stage, or stage IV NSCLC
If cancer spreads to another part of the body, beyond the organ in which it started, doctors call it metastatic cancer. Doctors have different views on the optimal standard treatment plan. Clinical trials may also be considered as a treatment option. Patients with stage IV NSCLC do not usually receive surgery or radiation therapy as primary treatment. Most receive systemic therapy such as chemotherapy, targeted therapy, or immunotherapy. Palliative care will also be important to relieve symptoms and side effects.
Upper limit
The position of the apexes of the lungs is assessed both anteriorly and posteriorly. On the front surface of the chest, the clavicle serves as a reference point, on the back - the seventh cervical vertebra (it has a long spinous process, by which it can be easily distinguished from other vertebrae).
The upper boundaries of the lungs are normally located as follows:
- In front, 30-40 mm above the level of the collarbone.
- Posteriorly, usually at the same level as the seventh cervical vertebra.
The research should be done like this:
- In front, the pessimeter finger is placed above the collarbone (approximately in the projection of its middle), and then moves upward and towards the inside until the percussion sound becomes dull.
- From the back, the examination begins from the middle of the spine of the scapula, and then the pessimeter finger is moved upward so as to be on the side of the seventh cervical vertebra. Percussion is performed until a dull sound appears.

How are the pulmonary boundaries located in a child?
Strictly speaking, the boundaries of the lungs in children practically correspond to those of an adult. The apexes of this organ are not identified in children who have not yet reached preschool age. Later they are detected in the front 20-40 mm above the middle of the collarbone, in the back - at the level of the seventh cervical vertebra.

The location of the lower boundaries is discussed in the table below.
| Boundaries of the lungs (table) | ||
| Field of study | Age up to 10 years | Age over 10 years |
| Line running from the middle of the collarbone | Right: 6th rib | Right: 6th rib |
| A line starting from the center of the armpit | Right: 7-8 rib Left: 9th rib | Right: 8th rib Left: 8th rib |
| Line descending from the angle of the scapula | Right: 9-10 rib Left: 10th rib | Right: 10th rib Left: 10th rib |
The reasons for the upward or downward displacement of the pulmonary boundaries in children relative to normal values are the same as in adults.
How to determine the mobility of the lower edge of the organ?
It was already mentioned above that when breathing, the lower limits shift relative to normal values due to the expansion of the lungs during inhalation and reduction during exhalation. Normally, such a shift is possible within 20-40 mm upward from the lower border and the same amount downward.
Determination of mobility is carried out along three main lines, starting from the middle of the collarbone, the center of the armpit and the angle of the scapula. The study is carried out as follows. First, determine the position of the lower border and make a mark on the skin (you can use a pen). The patient is then asked to take a deep breath and hold his breath, after which the lower limit is again found and a mark is made. And finally, determine the position of the lung at maximum exhalation. Now, focusing on the marks, you can judge how the lung shifts relative to its lower border.
In some diseases, lung mobility is noticeably reduced. For example, this occurs with adhesions or a large amount of exudate in the pleural cavities, loss of elasticity in the lungs due to emphysema, etc.