Fluorographic examination is carried out to diagnose pulmonary pathologies. Doctors primarily conduct a study to look for signs of tuberculosis, but fluorography can also detect other abnormalities.
The radiation dose during fluorography is sufficient to suggest tuberculosis and malignancy.
Why is fluorography necessary?
Fluorography is performed to detect abnormalities in the lungs. The procedure is rarely performed on children, only for indications. Only when they reach the age of fifteen do adolescents undergo periodic fluorographic examinations. The frequency of fluorography is once a year. You can visit the radiologist's office more often if a person has diseases that need to be monitored using x-rays.
For some categories of the population, the study is carried out twice a year. These are people working in hazardous industries, medical and teaching workers, patients, and those who live with a person suffering from tuberculosis. These people need to be tested more often because they are in contact themselves or can transmit the disease to others.
X-ray of healthy lungs
After the examination, the doctor, based on the diagnostic results, makes a short statement for the patient. It indicates the date of the examination, the data of the person undergoing diagnostics, and what dose of radiation the patient received during the X-ray.
In most cases, patients receive a spine indicating “no pathologies found” or “lungs and heart without changes.” The document confirming the completion of fluorography is valid for a year. It may be required in the following cases:

- when applying for a job;
- before a comprehensive examination;
- upon enlistment for military service;
- before surgery;
- when traveling abroad;
- for delivery to the maternity hospital.
Fluorographic examination helps not only to suggest tuberculosis of the lungs, but also neoplasms in the lung tissue, for example, cysts or malignant tumors. X-ray examination will help detect foreign bodies in the bronchi.

Compaction syndrome. Low to medium density lesion. Tuberculosis.
The following diseases can be identified from the image:
- pneumonia;
- cancer;
- sclerosis or fibrosis of lung tissue;
- tuberculosis.
By the presence of certain markers (pronounced network of blood vessels, dilated bronchi), doctors can directly or indirectly determine the disease the patient has. The lungs will also show the consequences of previously suffered pathologies, since adhesions, scars, and calcifications appear on their tissues.
Pulmonary tuberculosis manifests itself as oval spots in the body of the respiratory organs. Since fluorography is a fairly informative study, it is recommended to do it annually for the timely diagnosis of pulmonary pathologies.
System and non-system units of measurement
In the process of scientific discovery and subsequent study of sources of ionizing radiation and radioactivity, the need arose to introduce special units of measurement. The first such units were the Curie and Roentgen. Initially, in the world practice of studying radioactive background there was a complete lack of systematization, so today the primary units of measurement are usually called non-systematic.
Currently, the vast majority of states have adopted a unified international measurement system (CI). In the Russian Federation, the transition to CI began in January 1982. It was expected that it would be completed by January 1990, but political and economic events in the country significantly delayed the process. However, all modern dosimetric equipment is produced taking into account calibration in new units of measurement.
Over several decades of active study and practical application of X-ray radiation, a large number of different units of dose measurement were introduced: Rem, Gray, Becquerel, Rad, Curie and many others. They are used in various measurement systems and radiology applications. In the context of X-ray diagnostics, the most commonly used are Sievert and Roentgen.
Applications of X-ray and Sievert
The X-ray is today considered an obsolete unit of measurement. The scope of its application has narrowed significantly in recent years. Most often it is now used to display total radiation, while the amount of dose received by a person is indicated by Sieverts.
Another modern use of the X-ray unit is to determine the characteristics of an X-ray machine, including the level of penetrating radiation it emits.
For an objective and most accurate assessment of the impact of background radioactivity on the human body, the concept of equivalent absorbed dose is used. EPD makes it possible to determine the quantitative amount of energy absorbed by the body. The analysis is carried out taking into account the biological response of individual body tissues to ionizing radiation. When determining indicators, the unit of measurement used is the sievert. It is equal to approximately 100 Roentgen.
Thousands and millionths of Sievert/Roentgen
The radiation dose received during X-ray diagnostics is tens of times lower than 1 sievert. Many times lower than this unit of measurement and the natural background radiation. Therefore, to carry out more correct measurements, concepts such as millisievert (mSv) and microsievert (μSv) were introduced. One sievert is equal to a thousand millisieverts, or one million microsieverts. Similar values apply to X-ray.
Dose rate is usually displayed as a quantitative part of the received radiation over a certain time period. The most common units of time are seconds, minutes and hours. Consequently, frequently used indicators are: sv/h, msv/, r/h, mr/h and so on.
Contraindications to fluorography
There is no need to talk about absolute contraindications when conducting research. The procedure is non-invasive and does not cause harm to the body as long as it is performed within acceptable standards. Relative contraindications to fluorography are:
- the patient's health condition in which he cannot maintain a vertical position during the examination (with the exception of a device with a rotating stand);
- respiratory failure, which, if you hold your breath, can cause health problems in the patient;
- pregnancy (lactation period);
- under fifteen years of age.

Pregnant women should not undergo fluorography, but close relatives living with the pregnant woman should take a photo of the lungs. It is not recommended to do fluorography at the stage of pregnancy planning. X-ray effects on the fetus are unfavorable, so doctors try to protect women from unnecessary radiation exposure.
In case of urgent need, if a person needs to take a picture of vital signs, he must undergo a chest x-ray.
Harm of fluorography
Fluorography is extremely important for the timely detection of lung pathologies. However, despite the value of the study, doctors are wary of this diagnostic method, which is primarily due to radiation exposure.
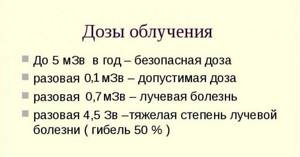
With a high radiation load on the body, rays can cause mutations in tissue cells and provoke the active growth of malignant tumors. X-ray exposure can cause radiation sickness. But there is no need to panic - patients are protected from exceeding the permitted annual dosage not only in practice, but also in law, since sanitary acts prohibit more than 5 mZV.
Digital scanning fluorograph (the safest and most modern diagnostic method)
X-ray examinations for preventive purposes are carried out safely, since patients do not receive additional radiation. Therefore, the procedure does not cause any harm, provided that the frequency of x-rays is observed.
Consequences of exposure to X-ray radiation on humans. Reference
Biological experiments on mice, rabbits and fruit flies have shown that even small doses of systematic radiation lead to harmful genetic effects. Most geneticists recognize the applicability of these data to the human body.
The degree of danger of X-ray radiation for people depends on the number of people exposed to radiation. This primarily applies to professionals working with X-ray equipment. This category includes radiologists, dentists, as well as scientific and technical workers and personnel maintaining and using X-ray equipment. The next category is patients. There are no strict criteria, and the safe level of radiation that patients receive during treatment is determined by the attending physicians. Doctors are advised against exposing patients to X-rays unnecessarily. Particular care should be taken when examining pregnant women and children. In this case, special measures are taken.
The accumulation of knowledge about the effects of X-ray radiation on the human body has led to the development of national and international standards for permissible radiation doses.
There are control methods that include three aspects: 1) availability of adequate equipment, 2) monitoring compliance with safety regulations, 3) correct use of equipment.
During X-ray examinations, only the desired area should be exposed to radiation, whether for dental examinations or lung examinations. Immediately after turning off the X-ray machine, both primary and secondary radiation disappear; there is also no residual radiation.
In addition to X-ray radiation, which is purposefully used by humans, there is also the so-called scattered, side radiation, which occurs for various reasons, for example, due to scattering due to the imperfection of the lead protective screen, which does not completely absorb this radiation. In addition, many electrical devices that are not designed to produce X-rays nevertheless generate them as a byproduct. Such devices include electron microscopes, high-voltage rectifying lamps (kenotrons), as well as picture tubes of outdated color televisions. The production of modern color picture tubes in many countries is now under government control.
The material was prepared based on information from open sources
All inquiries>>
Permissible dose of radiation
Diagnosis of the lungs is carried out in one projection. This means that the patient will receive a lower dose of radiation than with other diagnostic methods.
The dose of fluorographic examination with a digital scanning apparatus is 0.02-0.05 mSV. With a matrix type of device, 0.03-0.06 mSV. Film version (harmful) 0.1-0.3 mSV. To obtain more accurate numbers and assess harmfulness, please use the “Dosimeter”
X-ray of the lungs in two projections on a digital device will be 0.06-0.1 mSV, which is two times higher than fluorography.
Radiation exposure to the patient during pulmonary fluorography
Radiation diagnostics combines many types of intrascopy, of which the most common is the x-ray method, which has been used in medicine for more than 100 years. Preventive fluorography of the respiratory system in our country is traditionally considered one of the most common procedures. However, over the past decade, the attitude towards fluorography as an effective diagnostic method has changed dramatically. This is due to the poor state of fluorographic equipment, and hence the high radiation exposure to the patient, the low quality of film fluorogram images and the complexity of archiving the resulting images.
Both fluorography and x-ray are accessible and quite effective procedures for the early detection of preclinical forms of tuberculosis and lung cancer. At the same time, doctors are literally sounding the alarm about the dangers of such research, openly declaring that the radiation dose received by the patient can negatively affect health. Moreover, experts today claim that due to the large number of diagnostic studies during the year, the size of the radiation exposure to the patient has become so large that they are forced to talk about an ever-increasing collective radiation dose.
The structure of collective radiation doses to the population of Russia consists of the following main sources:
- natural
sources of ionizing radiation (radon and long-lived radon decay products - contribution to the collective dose 56%,
cosmic
radiation 14%, 70% in total); - medical
sources of ionizing radiation (x-ray diagnostics and radionuclide diagnostics - only 29%); - man-made
sources of ionizing radiation (only 1%).
The contribution to the total radiation dose of the population from sources of ionizing radiation used for medical purposes ranks second after natural sources. The average effective annual dose in Russia reaches 1.4 mSv per person per year. By structure in percentage: radiography – 34.1; fluoroscopy – 32.1; preventive fluorography – 23.5; diagnostic fluorography – 10.3. For comparison: in the UK - 0.3 mSv; in the USA and France - 0.4 mSv; in Japan - 0.8 mSv. On average, during medical examinations, one inhabitant of the Earth receives a radiation dose equivalent to 0.4 mSv per year.
By decision of the World Health Organization, traditional film fluorography is prohibited in the civilized world and is not recommended for use in underdeveloped countries due to its increased radiation exposure to the patient. As a result, due to a reduction in the frequency of preventive examinations of the population, the average annual level of medical exposure of the Russian population decreased from 1.4 to 1.2 mSv. However, due to the increasing frequency of tuberculosis outbreaks around the world in recent years, the importance of mass fluorographic examinations as a method of prevention has increased. In developed countries, this anxiety allows them to more actively seek ways to solve this problem. This primarily concerns the development, production and use of highly efficient X-ray diagnostic devices and the introduction of the latest computer technologies in medicine.
Since 1996, leading developers of X-ray technology have offered digital lung imaging systems to the international medical equipment market, based on various physical methods for obtaining X-ray images:
- on a large-diameter electronic image intensifier - (SIEMENS); TH59447HD (Thales); FSC-U-01 (SpektrAP).
- on the “selenium drum” - (PHILIPS); DR-1000 (Hologic).
- on “stimulated phosphor” - (FUJI); Orex (Israel); Agfa (Belgium).
- on the principle of optical transfer of images from the screen to one or more CCD matrices - (SWISSRAY); "Renex-Fluoro" Gelpik; "FPsF-01" X-ray industry; "KFC" Electron; "Dears-MR" Mosrentgen.
- on full-scale matrices made of amorphous silicon - (GENERAL ELECTRIC, SIEMENS, PHILIPS); Epex Hologic (USA); Pax Scan Varian (USA); Pixium-4600 (France); CXDT-11 Canon (Japan).
Such systems, in comparison with film fluorography, make it possible to slightly reduce the radiation dose without compromising the image quality required for phthisiopulmonology. However, the high cost of these devices (350-500 thousand US dollars) will not allow our country to carry out a mass replacement of more than 5,000 film devices, of which more than 2,000 are 15 years old or older.
But thanks to the introduction of knowledge-intensive and digital technologies in domestic production, real opportunities have been created to solve this problem at the modern level. Thus, JSC NAUCHPRIBOR (Orel), ELEKTROKHIMPRIBOR (Lesnoy) and BEMZ (Berdsk) serially produce microdose digital fluorograph MTsRU SIBERIA-N, which, with the best ratio of price and image quality, allows reducing radiation exposure to the patient by more than 30 times. This unique development of scientists from the INSTITUTE of Nuclear Physics named after. G.I. Budkera SB RAS (Novosibirsk) is one of the representatives of a new generation of digital radiographic devices based on scanning a patient with a narrow fan beam and recording the radiation passed through the object of study with a multichannel gas detector.
The scanning method involves recording a signal during synchronous movement of the X-ray emitter, collimator and detector along the object of study. The use of the scanning method in x-ray practice minimizes radiation doses, significantly improves the quality and contrast of images, since irradiation with a narrowly collimated beam practically eliminates the contribution of scattered radiation to the main information flow of x-ray quanta, especially when studying thick objects. Obtaining a digital X-ray image using a highly efficient gas detector with a large dynamic range (for film radiography - photographic latitude), allows you to simultaneously display low-contrast and high-contrast objects (lungs and mediastinum) on a digital radiograph, which distinguishes a digital image from a conventional film image [4] .
For more than 5 years, the use of the MCRU Sibir-N on the basis of the Central Clinical Hospital of the Siberian Branch of the Russian Academy of Sciences in Novosibirsk confirms the promise and safety of using a digital fluorograph when examining the population, as well as low radiation doses to patients and personnel. Studies of children at MCRU are carried out starting from 5-6 years old. The organs of the chest, paranasal sinuses, cervical spine, and skull are mainly examined. The photographs are quite informative and do not require control photographs on film in 76% of cases. The experience of using a digital fluorograph at the Oryol Regional Tuberculosis Dispensary has shown the high efficiency of the ICRU in identifying early forms of respiratory tuberculosis. The sensitivity of the method was 91% with a complete absence of technical defects, while at the same time the sensitivity of the 12F7 fluorograph was lower and technical defects occurred in 17.8% of cases [5].
When working with Thoravision from Philips, the radiation dose per image obtained at the choice of the radiologist can range from 10 to 40 mR. For comparison, with fluorography – 60 mR, with plain radiography – 20-40 mR. The dose for fluorography followed by control radiography can range from 80 to 140 mR. While the radiation exposure to the patient during an X-ray examination of the chest cavity in the anterior direct and right lateral projections on the MCRU does not exceed 2.0 mR. Photographs in two projections on a 12F9 film fluorograph with a KF-400 give a dose of about 1.2-1.4 mSv.
Measurements of effective radiation doses at the SIBERIA-N ICRU were carried out by the Department of Radiation Hygiene of RAM PA (Russian Medical Academy of Postgraduate Education, Moscow), using the thermoluminescent dosimetry method using an anthropomorphic RANDO PHANTOM phantom made in the USA. The diameter of the detector based on lithium fluoride made it possible to record the dose value almost at a point, therefore, in each of the critical organs (to determine the effective dose) from 10 (thyroid gland, liver, kidneys, stomach) to 50 (lungs, active bone marrow) of such point points were placed detectors. Measurements have shown that the effective dose during preventive X-ray examinations at MCRU is 100 times lower than the maximum annual effective radiation dose established (NRB-99) SP 2.6.1.758-99, and 3 times lower than the dose level corresponding to the upper limit of unconditionally acceptable risk.
Table 1 shows the average effective doses for X-ray studies of the chest area.
Table 1
| Type of study | Effective dose μSv | ||||||
| 70 kV | 80 kV | 100 kV | |||||
| Straight. | Side. | Straight. | Side. | Straight. | Side. | ||
| 1 | X-ray (5 min) | 3500 | 3500 | 3000 | 3000 | 2500 | 2500 |
| 2 | X-ray (with sensitivity 0.008 mGy) | 160 | 180 | 120 | 150 | 100 | 120 |
| 3 | Fluorography (with sensitivity 0.1-0.2 mGy) | 1500 | 1600 | 1000 | 1300 | 600 | 800 |
| 4 | Fluorography (with sensitivity 0.03-0.05 mGy) | 600 | 800 | 500 | 600 | 300 | 400 |
| 5 | Digital fluorography (3-6 µGy) | 50 | 65 | ||||
| 6 | ICRU Sibir-N (1.5% at 0.87 µGy; 0.5% at 6.1 µGy) | <7 | <11 | <10 | <13 | ||
| 7 | Longitudinal tomography | 5000 — 7000 | |||||
| 8 | CT scan | 3500 — 5000 | |||||
Low radiation exposure to the patient allows the use of MCRU in those areas of medicine where standard X-ray diagnostics could be carried out only for health reasons. Thus, when performing X-ray pelvimetry in one study, the patient receives a surface irradiation dose of 60-70 mR instead of 2-3 R obtained with screen-film radiography. The values given in Table 1 show that the use of MCRU Sibir-N in preventive studies of diseases of the thoracic cavity organs, in some cases it will allow: firstly ,
carry out dynamic monitoring of the condition of dispensary patients from high-risk groups with any necessary frequency;
secondly ,
to reduce the risk of radiation to a safe minimum when assessing the effectiveness of treatment over the dynamics of patients with pulmonary tuberculosis, which in turn will allow timely corrections in treatment; thirdly, remove from consideration the issue of radiation danger during mass examinations of earlier age groups.
According to the conclusion of leading phthisiatricians and radiologists, diagnostics at the SIBERIA-N MCRU makes it possible to achieve the highest level of detection of tuberculosis in the early stages, with no less than a 30-fold reduction in patient radiation doses in comparison with film fluorography.
Mass examinations using the traditional method of recording X-ray images leads to increased time and material costs associated with a rather complex process of photochemical development and the use of expensive silver-containing materials. The maintenance of a film archive formed as a result of the activities of the radiology department becomes expensive, since the shelf life of X-rays and fluorograms is two years in the absence of pathology, five years or more for images reflecting pathological changes. Pictures of sick children are stored for ten years. At the same time, according to world statistics, up to 20% of radiographs are lost when stored in archives or are difficult to reclaim in time. The loss of an image in the archive and defects, which are inevitably present in the production of radiographs, necessitate repeated studies, which leads to an increase in radiation exposure and additional labor costs.
The digital appearance of images makes it easy to organize compact and easily accessible X-ray archives. The benefits of digital archiving of medical images are presented in Table 2.
Table 2.
| Parameter | Digital archive | Film archive |
| Space occupied | 1 m3 | 900 m3 |
| Lost Films/Images | No | 5-20% |
| Access to images | Fast, simple | Complex, labor-intensive |
| Real time communication | Eat | No |
| Repeated studies | No | Eat |
| Cost and storage costs | Low | High |
| Individual accounting of radiation exposure | Eat | No |
| Fire hazard | No | Eat |
| Staff | No | Eat |
The accumulated information in the archive allows the image to be replicated many times, so there is no need for repeated examinations or can be used for a quick, comprehensive comparison of the results of examinations recorded over different periods of time. Digital ARCHIVE reduces the cost of an image and reduces the cost of diagnostic procedures, and makes it easy to carry out statistical analysis of the accumulated information. Printing images on the UP-895D thermal printer and accompanying information on a laser printer reduces the cost of consumables. Thus, expenses in the second quarter. 1999, when using film in the 30x40cm format, the cost was 38 rubles per photograph, for fluorographic 70x70mm - 12, for MTsRU - 6 rubles.
If necessary, you can send images over any distance for prompt consultations over computer networks, and the consultant is not given a subjective report of the examining doctor, but primary diagnostic information. To restrict unauthorized access to archive data, a security key is entered. The high information content of a digital radiograph and the ability to quickly work with the archive make it possible in many cases to quickly make a diagnosis and reduce the number of additional X-ray examinations by 10-20 times. Among other advantages of digital radiographs, it should be noted the possibility of mathematical processing using modern algorithms that improve the quality of images by converting them to a form that is most convenient for visual analysis. This will enable the physician to make an earlier radiological diagnosis in many cases.
Recently, at the bureau of the Scientific Medical Council, the Ministry of Health of the Russian Federation reviewed and recommended for use a method for active detection of tuberculosis based on computer technology. The entire adult population was divided into three groups according to the degree of risk of getting sick - high, medium and low. The first group is examined annually, the second - once every two years, and the third group is not yet examined at all. This makes it possible to conduct a fluorographic examination of approximately half of the adult population and at the same time identify 80-85% of patients with tuberculosis. The remaining 15-20% is the business of general practitioners, where people go with complaints of cough and malaise. Excluding the low-risk group from examinations and examining the medium-risk group once every two years will reduce the collective radiation dose. However, in the future, healthcare will be forced to restore the system of mass fluorographic screening in the same or even larger volumes due to the emergency epidemic situation regarding tuberculosis. Therefore, the use of outdated models of X-ray machines in medical practice will lead not only to a decrease in the quality of diagnostics, but also to the inevitable duplication of many X-ray procedures. There is also a danger that the worn-out fleet of fluorographic equipment in the country will not be promptly updated with modern low-dose devices; this will lead to a forced increase in dose loads on patients and personnel, which will inevitably increase the average dose of medical radiation to the population by 1.5 times.
Taking into account the experience of using ICRU SIBERIA-N in medical institutions, as well as laws adopted for the safety of the population and in order to strengthen measures to combat tuberculosis, we can recommend ICRU for the gradual replacement of film fluorographs currently in operation with all the necessary methodological, organizational and technical measures. The rapid implementation of ICRU in practical healthcare will significantly reduce the collective radiation dose, automate individual accounting of radiation doses to the population and prepare reports on the volume and structure of x-ray studies in Form No. 30 for the year.
Fluorography for children
The study is usually not performed on children. If you need to screen for tuberculosis, doctors use the Mantoux test or Diaskintest, which indicate infection with tuberculosis bacilli.
This is why “buttons” are so common in children at school age - the main markers of the presence of tuberculosis. Fluorography is allowed from the age of fifteen.

X-rays for children are performed when absolutely necessary, if the child has external signs of tuberculosis or other severe abnormalities. For children, the smallest dose is chosen.
Harm of annual fluorography
Lung examinations are carried out every year. This is not harmful with a digital type of examination, since a person receives 0.01-0.02 mSV during the day, plus talking on the phone - 0.01 mSV, a trip to the subway due to marble and granite - 0.04 mSV.
The natural background of Moscow is 0.02 mSV. Therefore, fluorography is not considered a fact that can lead to complications.

Fluorography does not exceed the dose of x-ray radiation received per year, and according to the established annual standards, the study can be done several times a year. If necessary, doctors give a referral for an extraordinary study.
How dangerous is the dose of radiation received during an X-ray of the spine?
To understand this, you need to consider that in a year of normal life (that is, without fluorography, CT scans and x-rays), a person receives from 2 to 3 mSv. The numbers vary, because... this indicator strongly depends, for example, on the altitude above sea level.
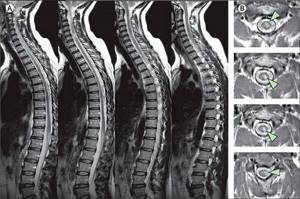
The indicated figure consists of:
- Cosmic and solar radiation 0.3-0.9 mSv;
- Natural soil background 0.25-0.6 mSv;
- Radiation from building materials from 0.3 mSv;
- Dose received from air 0.2-2 mSv, etc.
By the way, during a 10-hour flight at an altitude of 12 km, an airplane passenger receives a radiation dose equal to 0.03 mSv.
Having carried out a simple comparison of the obtained figures, we will see that in terms of the dose received, a flight from Russia to the USA is quite comparable to an X-ray of the spine with digital data recording; radiation from building materials and air causes much more harm.
Based on the data presented, it becomes clear that, although there is harm from an X-ray of the spine, it is not much greater than the harm from flying on an airplane or from living in a city with an abundance of building materials and is definitely not worth refusing the examination due to the potential danger . We must always remember that the danger of X-ray radiation is much lower than the consequences of poor diagnosis of spinal diseases, incorrect diagnosis and errors in determining the location of the problem, which can lead to severe complications, disability and even death of the patient.
Alternative to fluorography
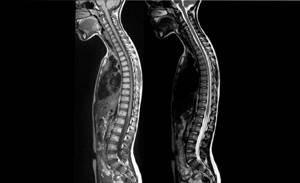
If there is a suspicion of pathology after undergoing fluorography, or for some reason the patient cannot undergo fluorography, then the doctor will prescribe alternative methods.
Internal organs can be visualized using radiography. This study is more harmful and more informative, since the radiation exposure is twice as high. A chest x-ray can accurately determine the presence or absence of tuberculosis.
Computed tomography (CT) in relation to tuberculosis and neoplasms will be more informative and harmful.

The most harmful diagnostic method
How to reduce the harm of x-rays
During an X-ray examination, the patient is protected from the spread of rays throughout the body. In this case, the health care worker fixes a lead apron on the patient’s body that does not transmit x-rays. This is the first stage at which you can protect yourself from harmful effects.
After the diagnosis, care must be taken to remove the effects of the x-ray. Patients are advised to drink fresh milk, juices, and walk more.
Residual effects after fluorography are eliminated on their own, but taking Polyphepan to cleanse the body will not cause harm.
Fluorography of the lungs is an indispensable procedure for diagnosing tuberculosis, cancer and other pathologies. All people should undergo a scheduled examination once a year in order to diagnose abnormalities in time and not become a source of infection for others.