The thyroid gland is located in the front of the neck and is part of the endocrine system. Produces hormones that coordinate the processes of growth, tissue differentiation, and metabolism. Sometimes patients are prescribed a CT scan of the thyroid gland. This type of diagnosis allows you to obtain many high-quality images of an organ in a short time, on the basis of which you can create a volumetric reconstruction with detailed visualization of the pathology.
Computer tomogram of the thyroid gland
Computed tomography is used only when other methods are insufficiently informative, since thyroid tissue is highly sensitive to radiation. At the initial stage, the examination is performed using palpation, ultrasound, laboratory technologies and functional tests. If these methods could not show the full picture or the doctor doubts the information received, a tomography is needed. X-ray computer diagnostics is relevant for the retrosternal location of an enlarged organ and for contraindications to MRI.
What does a thyroid CT scan show?
Using computer scans, a specialist can judge the shape, size, structure and position of the organ, the condition of the lymph nodes, parathyroid glands, trachea, esophagus, and the presence or absence of pathological changes.

Thyroid tumor on computed tomography
CT scan shows:
- enlargement of the thyroid gland;
- focal changes (cysts, nodes, adenomas, calcifications);
- inflammatory processes;
- neoplasms (benign or malignant will be determined after the material is submitted for analysis);
- tumor invasion of the trachea or neurovascular bundles;
- atrophy or hypoplasia (congenital reduction of the entire organ or underdevelopment of one of the lobes);
- local circulatory disorders (arterial and venous hyperemia);
- hemorrhages into the gland tissue.
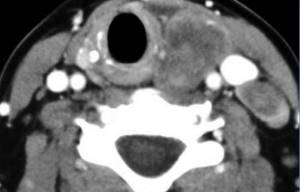
CT scan of the thyroid gland with contrast
CT scanning of thyroid tissue requires contrast, since conventional images do not show nodules, vessels, or tumors. In order to improve visualization, special iodine-containing drugs are administered intravenously. Once in the bloodstream, the contrast agent quickly fills the vascular network of the organ and clearly highlights on tomograms not only the latter, but also the pathologically altered areas.

Photo of CT scan of the thyroid gland with contrast
After administering the indicator solution immediately or after some time, a person may feel nausea, a metallic taste in the mouth, or a feeling of warmth in the body. This is a standard reaction to a contrast agent and does not require outside intervention.
Warning symptoms:
- facial swelling;
- severe dizziness;
- skin itching, rash;
- sore throat;
- difficulty breathing (bronchospasm);
- a sharp decrease in blood pressure;
- pathological excitement.
If at least one of them appears, you need to contact medical personnel without waiting for the thyroid tomography to be completed.
Preparing for a thyroid test
A thyroid CT scan does not require extensive preparation. One or two days before the test, you should only give up iodine-containing products and medications (including those for external use). Otherwise, the diagnostic data may be distorted.
Before the procedure, it is advisable to eat moderately; on an empty stomach, the side effects of the contrast agent are more pronounced. Women during lactation are advised to express and store milk in advance, since the diagnostics carried out exclude breastfeeding for several hours.
A CT scan of the thyroid gland with contrast is done only if the results of a creatinine test are available. The concentration of this compound in the blood directly depends on the functioning of renal filtration. The slightest deviation from the norm increases the risk of deterioration in health after administration of an iodine-containing drug.
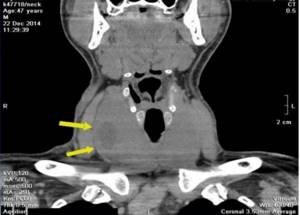
Nodular goiter of the thyroid gland on a computed tomogram (focal changes are indicated by arrows)
When is radiography indicated?
This study is prescribed extremely rarely, since today there are safer and more accurate methods. An appointment for a study can be obtained if a goiter is visualized, or if there are disorders of the esophagus or trachea.
During the procedure, you can detect: metastases that remain after removal of the cancer; the presence of hyperthyroidism and hypothyroidism; determine the boundary between a node and a diffuse lesion.
It is important to understand that this type of research negatively affects all other vital organs, since the radiation dose increases at least tenfold.
How is a thyroid CT scan done?
Before entering the room where the examination will be carried out, you must remove all things that contain metal. Computed tomography of the thyroid gland is performed on a machine equipped with a movable table and a scanning system consisting of an X-ray tube and sensors. The patient lies down with his back down, a stand is placed under the neck. Using an automatic injector, contrast is injected into the vein halfway through the procedure.

Computer tomograph - photo
The doctor observes the examination process from the next room through glass. There is a speakerphone in the room where the staff is located, through which the patient receives instructions and can report any discomfort that has arisen.
The diagnostic procedure is absolutely painless. The X-ray tube rotates around the neck and chest area, a fan-shaped beam of rays passes through the human body and is recorded by a system of detectors. The information is sent to a computer, where it is subsequently analyzed by a radiologist.
During scanning, you should relax and maintain a still position so that the pictures are as clear as possible. CT diagnostics of the thyroid gland with contrast takes 15 minutes, after which you can almost immediately return to your usual activities.
Where to do research
This procedure can be carried out in government medical institutions and in special diagnostic centers. It is important that the facility has the necessary equipment and a competent radiologist.
Content:
- Who prescribes diagnostics
- Where to do research
- When is radiography indicated?
- Contraindications to X-ray diagnostics
- How to prepare for an X-ray examination
- Decoding the results
- What diseases can be determined using X-ray diagnostics?
Tomography of the thyroid and parathyroid glands
Parathyroid glands are called endocrine glands located on the back of the thyroid gland. Usually a person has four of them - the lower and upper pairs, but there can be from one to twelve. The main function of the parathyroid glands is the production of parathyroid hormone, which regulates phosphate-calcium metabolism. Violation of this process leads to a malfunction of most important systems, which is why various diseases develop.
CT scanning of the thyroid and parathyroid glands is prescribed in the following cases:
- tetany (involuntary painful muscle contractions);
- convulsions;
- paresthesia (feeling of numbness, crawling or tingling in the limbs, face, tongue);
- the appearance of neurological symptoms - irritability, psychosis, epileptic seizures;
- osteoporosis of unknown origin;
- urolithiasis disease;
- the presence of a voluminous neoplasm in the neck area;
- control after surgery.
Tumor of the parathyroid gland on a CT scan
A contrast study allows you to accurately determine the location and size of the parathyroid glands, even if they are located in the retrosternal space.
Indications and contraindications
The main indications for CT analysis of the thyroid gland:
- sudden change in voice;
- respiratory disorders due to compression and displacement of neighboring anatomical structures by the thyroid gland;
- difficulty swallowing food and liquids;
- enlarged cervical lymph nodes;
- atypical location of the organ (when the lower part or the entire gland is located behind the sternum);
- presence of nodes (according to ultrasound results);
- suspicion of a tumor;
- the need to exclude or confirm metastasis;
- congenital anomalies of the thyroid gland;
- preparation for surgery and monitoring after it.
General contraindications to the procedure:
- pregnancy regardless of stage;
- children under 5 years of age;
- body weight over 150 kg and chest (abdomen) girth over 150 cm.

Magnetic resonance imaging (MRI) in St. Petersburg
The thyroid gland consists of two lobes connected by an isthmus. The isthmus is located between the 2nd and 4th tracheal cartilages. The size of the lobe is approximately 4.0 x 1.5 x 2.0 cm (length-width-depth). The lower pole reaches the 5-6 tracheal ring. From above, the lobe reaches the thyroid plate. The gland is covered with bundles of the hyoid muscle. 40% of people have a pyramidal lobule located in the area of the upper pole of the isthmus. The gland weighs 15-25 g. The gland is supplied with blood from the superior and inferior thyroid arteries and its own artery, which arises from the aortic arch or innominate artery. The outflow of blood goes through the upper, middle and lower thyroid veins.
Clinical manifestations of pathologies consist of hypo- or hyperthyroidism. Hypothyroidism is associated with impaired hormone production, mainly in various types of thyroiditis. Hyperthyroidism is associated with various types of thyrotoxicosis.
ETIOLOGICAL CLASSIFICATION OF THYROID DISEASES
- I. Autoimmune thyropathies.
- Graves' disease.
1.1. Isolated thyropathy.
1.2. Thyropathies with extrathyroidal manifestations.
- Autoimmune thyroiditis.
2.1. Chronic autoimmune thyroiditis.
2.2. Transient autoimmune thyroiditis.
2.2.1. Painless (“silent”) autoimmune thyroiditis.
2.2.2. Postpartum autoimmune thyroiditis.
2.2.3. Cytokinin-inducing autoimmune thyroiditis
- II. Colloidal, proliferating goiter to varying degrees. Diffuse goiter.
- Nodular and multinodular goiter.
2.1. Nodular and multinodular goiter without functional autonomy.
2.2. Nodular and multinodular goiter with functional autonomy.
III. Infectious thyropathies.
- Subadult thyroiditis.
- Acute purulent thyroiditis.
- Specific thyroiditis.
- IV. Tumors Benign.
- Malignant.
- V. Congenital (hereditary) thyropathies.
- VI. Diseases of the thyroid gland in the pathology of other organs and systems.
Nodules in the thyroid gland occur in 4-7% of the adult population. These can be colloid nodes, adenoma, focal hyperplasia, cysts, metastases, thyroid tumor.
Diagnostic methods: radionuclide, ultrasound, and MRI .
Iodine-123 scintigraphy shows “hot” and “cold” nodes. Iodine-131 and technetium preparations are also used. “hot” nodes are usually adenomas, “cold” nodes can be malignant in 1-4% when studied with iodine and up to 30% when studied with technetium.
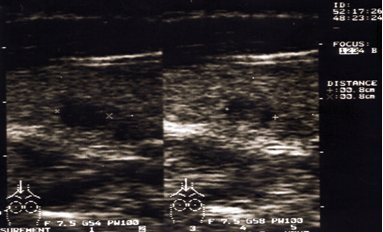
Ultrasound perfectly shows the anatomy of the gland and hypoechoic nodes, as well as cysts. A disadvantage is poor visualization of lymphadenopathy and surrounding tissue. Ultrasound is the most accurate in terms of diagnosing cysts. However, complicated cysts may turn out to be carcinoma. For accurate diagnosis, ultrasound is supplemented with fine-needle biopsy.
Tomographic studies better reflect the anatomy and are possible in thin sections. Since the administration of iodine contrast is undesirable, MRI is preferable to CT. MRI excellently demonstrates extension toward the mediastinum. It is believed that MRI reliably shows nodes up to 4 mm.
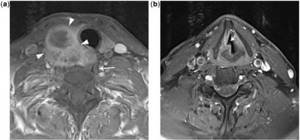
MRI. Thyroid cancer with invasion of the recurrent nerve. T1-dependent and T2-dependent axial tomograms.
The most common pathologies of the thyroid gland include nodular hyperplasia. On ultrasound, nodules are detected in 30% of subjects aged 19-50 years, and in 60% or more of those over 60 years of age. Only 1 in 20 nodes turns out to be malignant.
CT and MRI for tumors reflect signs of malignancy: infiltrative growth and vascular invasion. Carcinoma is contrasted on CT and MRI .
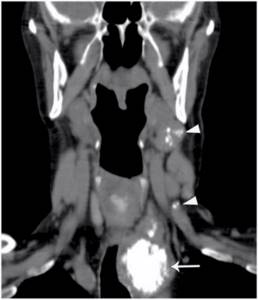
CT. Reformation into the coronal plane. Lymph nodes of the neck with calcifications.
Staging of thyroid cancer is carried out according to the TNM system:
T-tumor
- TX – Primary tumor cannot be assessed
- T0 – No evidence of tumor
- T1a - Tumor ≤1 cm, limited to the thyroid gland
- T1b – Tumor >1 cm but ≤2 cm in greatest dimension, limited to the thyroid gland
- T2 – Tumor >2 cm but ≤4 cm in greatest dimension, limited to the thyroid gland
- T3 – Tumor >4 cm in greatest dimension, limited to the thyroid gland or any tumor with minimal extension beyond the thyroid gland
- T4 - Extensive disease T4a - Moderately extensive disease - tumor of any size extending beyond the capsule into the subcutaneous soft tissues, larynx, trachea, esophagus, or recurrent nerve
- T4b – A very common disease - the tumor invades the paravertebral fascia or engulfs the carotid artery or mediastinal vessels
- cT4a – Intrathyroid anaplastic carcinoma
N: Lymph nodes
- NX – Regional lymph nodes cannot be assessed
- N0 – No metastases to regional lymph nodes
- N1 – There are metastases to regional lymph nodes N1a – Metastases up to level VI (pretracheal, paratracheal, and preglottic)
- N1b – Metastases to unilateral, bilateral and contralateral cervical (Levels I, II, III, IV, or V) or retropharyngeal or upper mediastinal lymph nodes (Level VII)
M: Metastasis
- MX – Distant metastases cannot be assessed
- M0 – No distant metastases
- M1 – There are distant metastases
In addition to the TNM system adopted by WHO, there is also a simplified TIRADS , adopted by radiology diagnosticians in some countries (for example, the USA). The system involves a visual assessment of the condition of the thyroid gland, for example, using ultrasound.
ULTRASONIC DIAGNOSTICS OF THYROID DISEASES
- Autoimmune thyropathies
Graves' disease (Diffuse toxic goiter, Graves' disease).
It is characterized by hyperplasia of the thyroid gland with an increase in its function. Echographically, unevenness or scalloping of the contours of the gland is determined. A decrease in echogenicity is not a specific sign of hyperthyroidism, since it can occur due to increased vascularization of the parenchyma or other processes leading to an increase in the hydrophilicity of the thyroid tissue (lymphocytic infiltration, reactive changes in the thyroid gland against the background of adenovirus infection). Hypervascularization of the thyroid gland using Doppler echo was first described by Rails in 1988 and called “Thyroid inferno” - “fire” in the thyroid gland. The uniformity of blood flow indicators in all regional vessels of the thyroid gland, as well as in the region of the lobes, in patients with Graves' disease confirms the well-known opinion about the uniform functional activity of the entire parenchyma of the thyroid gland. Against the background of hyperproduction of thyroid hormones, recanalization of the previously collapsed vessels of the gland parenchyma occurs.
Autoimmune thyroiditis.
This group includes acute, subacute and chronic inflammatory diseases of the thyroid gland, which are based on autoimmune, cytotoxic processes, with simultaneously occurring processes of degeneration and tissue regeneration. The echographic picture largely depends on the functional state of the gland. The gland can be either enlarged, normal or reduced in size, its contours are often uneven. The echo density of the gland is often reduced, the echo structure is heterogeneous due to multiple hypoechoic areas of various shapes and sizes, mostly without clear contours, as well as hyperechoic strands that give the gland a lobular structure. Large foci of low, or less often increased, echogenicity may resemble nodes, however, with ultrasound, the vascular pattern in the “node” zone does not differ from neighboring areas. Parenchymal blood flow is characterized by an increase in the total number of visualized vessels. In this case, a direct proportional relationship is found between the number of visualized vessels and the activity of chronic autoimmune thyroiditis (the higher the number of vessels, the higher the activity of the pathological process), the uniform distribution of vessels throughout the entire volume of the organ, the increase in speed indicators and the resistance index.
Autoimmune thyroiditis ( Hashimoto's goiter).
The disease is characterized by an increase in quantitative indicators equally in all regional vascular collectors with normal values of qualitative parameters. In the active stage, it is practically indistinguishable echographically from Graves' disease. Detection of hypoechoic pretracheal lymph nodes with a diameter of 4-8 mm is an indirect sign of thyroiditis activity. Clinical diagnosis is based on the detection of an increase in the titer of antibodies to thyroglobulin.
Ultrasound. Hashimoto's thyroiditis.
Chronic thyroiditis.
In the process of treating thyroiditis with medications, it is not always possible to achieve normalization of the structure of the thyroid tissue. At one of the stages of improvement of the patient’s general condition, the echographic picture seems to be frozen, and remission is defined as subclinical. When echography, a gland of normal, enlarged, and even sometimes reduced size is visualized, with alternating areas of reduced, medium, and increased echogenicity.

Ultrasound. Chronic autoimmune thyroiditis.
Fibrous-invasive thyroiditis (Riedel's goiter).
A very rare form of thyroiditis, characterized by focal or diffuse enlargement of the gland, most often one lobe and the isthmus change. As a result of the replacement of the parenchyma with hyalinized fibrous tissue, on echograms the iron appears heterogeneous due to the presence of iso.- and hyperechoic areas.
Ultrasound. Fibrous-invasive thyroiditis.
Atrophic thyroiditis.
The thyroid gland is reduced in size, its echostructure becomes heterogeneous, and is poorly differentiated from the surrounding muscle structures. Ultrasound angiography shows reduced vascularization of the thyroid gland.
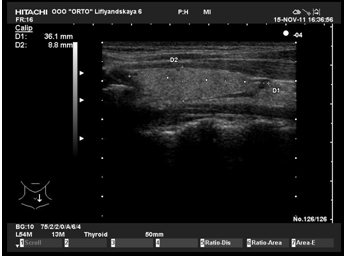
Ultrasound. Atrophic thyroiditis.
Hypertrophic (nodular) thyroiditis.
The thyroid gland is enlarged due to intraparenchymal nodes. With ultrasound, one can see the displacement of parenchymal vessels by nodes to the periphery.
Ultrasound. Hypertrophic thyroiditis.
Colloidal, proliferating goiter to varying degrees
Diffuse goiter.
Characterized by an increase in the volume of the thyroid gland by more than a third. The following degrees of enlargement of the thyroid gland are distinguished:
grade 0 - the gland is not visible and not palpable;
grade 1 - the gland is not visible, but the isthmus is palpable and visible during swallowing movements;
degree 2 - clearly visible and palpable during swallowing, but the shape of the neck is not changed;
grade 3 - the gland changes the contour of the neck, giving it a thick appearance;
degree 4 - the enlarged gland reaches enormous sizes, which is often accompanied by compression of the esophagus and trachea with impaired swallowing and breathing.
The echostructure of the gland is medium- and coarse-grained, with areas of cystic degeneration in the form of anechoic and hypoechoic zones. With ultrasound, a slight increase in the number and size of the vessels of the gland is noticeable, which is associated with an increase in its volume.
Nodular goiter.
With nodular goiter, the thyroid gland is enlarged in size due to single or multiple nodes. The contours of the gland are clear, often even, but can also be uneven if the nodes are localized at the edges. The structure of the nodes is characterized by pronounced polymorphism - from clearly visualized formations of reduced or increased echogenicity to confluent isoechoic foci, barely distinguishable from the surrounding parenchyma. With ultrasound, three-dimensional reconstruction of the vessels of colloid nodes allows one to clearly determine the course of vascular structures, assess the vascularization of the node, both in the periphery and in the center, and also identify the vessels supplying the node. Colloidal formations are often characterized by extranodular blood flow.
Adenomas, when scanned in B-mode, do not have specific ultrasound signs that allow them to be distinguished from other nodular lesions. They can be visualized as single or multiple hyper-, hypo- or isoechoic formations of round or oval shape, with clear, even contours, homogeneous or heterogeneous structure (cystic hemorrhagic degeneration is observed in 1/3 of patients), with hypo- or hyperechoic perinodular capsule along the periphery. Sometimes single or multiple calcifications are visualized in adenomas. The presence of a hypoechoic rim along the periphery is primarily due to the vascular component, which is confirmed by ultrasound. Extranodular blood flow and/or a distal pseudoenhancement effect suggests a benign process.
Colloid nodes are the most common finding during surgical interventions and do not have pathognomonic ultrasound signs. In the case of multinodular colloid goiter, the structure of the gland can be represented by nodes of all echographic types. Ultrasound significantly improves the accuracy of diagnosing nodular formations. Thus, when nodes form in the gland tissue, there is a disturbance in the course of blood vessels, their displacement to the periphery with the subsequent formation of a vascular rim, where a high blood flow velocity is recorded - more than 40 cm/s. This is probably due to compression of the vessels by the nodular tissue. In relation to nodular formations, three types of vascular pattern can be distinguished: avascular, extranodular, mixed. In nodes less than 0.4 cm, vessels and blood flow are usually not detected (avascular type). The most typical image of a hyperplastic process is isoechoic formations with a hypoechoic rim of varying thickness (“halo”) along the periphery - hypervascularization around the node. Three-dimensional reconstruction of vessels in the nodes makes it possible to determine their course. More often, extranodular blood flow is detected in colloid formations. Nodules with extranodular blood flow are divided into hypovascular and hypervascular. Hypervascular (“hot”) nodes are characterized by: a significant increase in the number of visualized vessels, their concentration along the periphery of the nodes. Hypovascular (“cold”) nodes are characterized by an unchanged number of visualized vessels or their slight increase compared to the norm, extranodular blood flow. Sometimes in colloid formations a mixed type of vascular pattern is determined, which is characterized by the presence of extra- and intranodular blood flow.
Ultrasound. Colloidal nodes.
Ultrasound. Colloidal node.
Three-dimensional reconstruction of vessels makes it possible to differentiate the type of vascularization (normal or increased) due to the severity of the vascular pattern and the presence of dilated vessels, both along the periphery and inside the node. A mixed type of blood flow is characteristic of both non-toxic and toxic thyroid adenomas (autonomous adenoma, Plummer's disease). In most cases, they have the appearance of clearly defined hyperechoic formations with a perinodular rim 1-3 mm thick.
III . Infectious thyropathies
Subacute thyroiditis.
Subacute granulomatous thyroiditis (De Carvain's thyroiditis) is a rare disease. The occurrence of the disease is associated with a viral infection, but the causative agent has not been clearly identified. It is believed that subacute thyroiditis can be induced by the Coxsack virus, adenoviruses, endemic mumps virus, etc. Hereditary factors contribute to the development of De Carvin's thyroiditis. Genetic predisposition to this disease is associated with functional disorders of the histocompatibility system.
Most often occurs in women aged 40-50 years. It is characterized by degenerative-dystrophic changes in the follicles with simultaneous proliferation of the stroma. As a result of these processes, peculiar granulomas are formed, which contain giant cells and are immured among fibrous connective tissue. Diagnosis of the disease is difficult, which is explained by the vague symptoms and rarity of the disease.
Early signs of De Carvin's thyroiditis are: discomfort when swallowing, general malaise, pain in the thyroid gland. The stage of development of clinical symptoms is characterized by intense pain in the neck radiating to the lower jaw and occipital region. The pain intensifies when turning the head, chewing, and swallowing. Intense sweating, palpitations, insomnia, and arthralgia are noted.
On palpation, the thyroid gland may be moderately enlarged, dense, and painful. Regional lymph nodes are usually not enlarged. In most patients, symptoms of thyrotoxicosis are observed in the initial period of the disease.
In recognizing De Carvin's thyroiditis, laboratory data acquire a certain significance. A general blood test reveals an increase in ESR and lymphocytosis in patients. Nonspecific markers of an acute inflammatory reaction appear in the blood serum. An increase in the level of thyroxine and triiodothyronine in the blood is also characteristic. Some patients experience a sharp increase in thyroglobulin in the blood. The described changes are not pathognomonic for subacute thyroiditis. The final diagnosis is usually formulated by cytological examination of aspirates from thyroid tissue.
Ultrasound examination reveals an increase in the size and volume of the thyroid gland with a diffuse decrease in the echogenicity of the parenchyma. In a number of patients, loci of a distinct decrease in acoustic density are visualized.
Painless subacute thyroiditis.
It usually occurs sporadically or after pregnancy. Its peculiarity is the absence of pain. Painless subacute thyroiditis is manifested by symptoms of thyrotoxicosis in 30-40% of patients and hypothyroidism in 25-40%. A characteristic feature of this disease, accompanied by symptoms of thyrotoxicosis, is the relatively low level of accumulation of I¹³¹ by the thyroid gland during a scintigraphic study, which is the main criterion for differential diagnosis.
Ultrasound examination reveals an increase in the size and volume of the thyroid gland with a slight diffuse decrease in the echogenicity of the parenchyma and hypoechoic areas with unclear contours. FNA allows us to exclude the diagnosis of malignant tumors.
Acute purulent thyroiditis (strumitis).
A very rare disease caused by a bacterial infection. Damage to the thyroid gland is usually secondary (against the background of tonsillitis, sepsis, etc.). The infection spreads to the thyroid gland directly from a nearby purulent focus, lymphogenously or hematogenously.
An increase in the size and volume of the thyroid gland with a diffuse decrease in the echogenicity of the parenchyma is determined. As the disease progresses, an abscess forms.
IV Tumors
Benign tumors.
Benign thyroid tumors develop due to local hyperplasia of thyrocytes. Under the influence of unknown factors, there is a sharp increase in the rate of division of individual follicular cells, due to the growth of which adenomatous nodes are formed.
Thyroid adenomas are quite common. They make up 17-25% of all volumetric formations removed during surgical diseases of the thyroid gland. Adenomas usually occur in the form of single nodular formations, but often multiple adenomatous nodes form in the thyroid tissue. There are macro- and microfollicular adenomas, papillary adenomas, follicular-papillary adenomas, adenomas from Ashkinasi-Hurthle cells and adenomas from C-cells. All these benign tumors of the thyroid gland, regardless of the type of their histological structure, are characterized by the presence of a connective tissue capsule located around the formation.
During ultrasound examination, in most cases, the adenoma has the appearance of a clearly defined hyperechoic formation. In typical cases, it is surrounded by a rim 1-3 mm thick with a sharply increased intensity of reflected echo signals (“hyperechoic rim”). In a third of cases, the echostructure of the tumor is homogeneous. In more than 50% of diseases, hypoechoic inclusions appear in the tissue of adenomas, which are a consequence of hemorrhages in the parenchyma of adenomas. In 10% of cases, calcifications are detected in the structure of tumors.
Ultrasound. Multiple adenomas.
However, there are benign thyroid tumors with a density indistinguishable from unchanged tissue (10% of adenomas) or hypoechoic (4% of adenomas), which is associated with the type of their histological structure. Only cytological analysis of biopsy specimens allows one to determine the benign nature of the cells.
Malignant tumors.
Thyroid cancer has no specific ultrasound signs and is echographically indistinguishable from an adenoma or colloid node. Malignant epithelial tumors of the thyroid gland with different histological structures can have a variety of ultrasound features.
Undifferentiated thyroid cancers are identified on sonograms as hypoechoic zones of various sizes and shapes, with uneven “eaten” edges and unclear delineation from unchanged thyroid tissue. In most cases, signs of tumor growth into surrounding tissues are visualized, which is accompanied by a violation of the integrity of the thyroid capsule. With color Doppler mapping, extra- and intranodular blood flow is determined.
Papillary thyroid cancer during ultrasound examination is most often visualized as a hypoechoic area of irregular shape with unclear contours. In the center and periphery of the tumor node, hyperechoic areas are often visible, which are zones of calcification. In some cases, cystic degeneration of cancer tissue occurs. A characteristic feature of papillary thyroid cancers is their slow growth and relatively late metastasis. Color Doppler imaging demonstrates hypervascularity in the form of marginal and intranodal blood flow.
Follicular adenocarcinomas occupy an intermediate position in invasive growth among epithelial malignant tumors, which is characterized by a special variety of echosemiotic features. Quite often, low-echoic formations with a heterogeneous echostructure are identified (multiple calcifications are located in the center and along the periphery of the node). Along the periphery of the formation there is a wide low-echoic rim of uneven thickness. In other cases, the tumor tissue grew into the gland capsule. In most cases, follicular cancer nodes do not have clear boundaries. Color Doppler mapping determines extra- and intranodular blood flow, which is characterized predominantly by arterial vessels.
Medullary thyroid cancer during ultrasound examination is characterized by visualization of hyperechoic areas against the background of hypoechoic zones of various sizes and shapes. It is believed that areas of compaction in the tumor node are caused by the appearance of zones containing amyloid and reactive fibrosis. There may be an increase in the acoustic echodensity of the thyroid gland and the appearance of hyperechoic zones in the cervical lymph nodes. Color Doppler mapping determines intranodular blood flow.
Ultrasound. Medullary cancer.
In patients with suspected thyroid cancer, ultrasonography can be used only as a method to recognize local changes in the thyroid parenchyma. To make a final diagnosis, regardless of the echo density and size of the formation, it is necessary to perform a targeted biopsy from pathological areas.
Thyroid cysts
Simple thyroid cysts are extremely rare. Most cystic lesions of the thyroid gland are adenomas or adenomatous nodes that have undergone cystic or hemorrhagic degeneration. During ultrasound examination, a simple thyroid cyst is visualized as an anechoic formation of a round or oval shape, with clear, even contours, a smooth inner surface and distal pseudo-enhancement. In the cavity of the cysts, a coarse or fine suspension can sometimes be traced, sometimes with the formation of a horizontal level, which may be due to both the hemorrhagic contents of the cyst and the colloid. The structure of hemorrhagic cysts undergoes rapid changes due to the formation of clots and fibrin threads, which increase the echogenicity of the cyst. Complex thyroid cysts, in addition to the above symptoms, are characterized by the presence of a parietal tissue component.
Thus, ultrasound examination using color Dopplerography and energy mapping is a highly informative method for non-invasive diagnostic diagnosis of thyroid pathology. The results obtained indicate the high efficiency of the methods used in the differential diagnosis of benign and malignant processes.
The use of modern ultrasound technologies makes it possible to solve problems of diagnosing pathological processes at completely new qualitative and quantitative levels, as well as to monitor patients in the process of specific treatment. MRI of St. Petersburg rarely collides with the study of the thyroid gland. If ultrasound is unclear, we recommend MRI in St. Petersburg as a clarifying method in a high field or open MRI.
Leave feedback.
MRI in St. Petersburg USA
Contraindications to computed tomography
There are also a number of contraindications associated with the use of iodine-containing substances. The thyroid gland (CT with contrast) is not examined in patients with:
- severe renal or liver failure;
- iodine intolerance;
- hyperthyroidism (additional iodine in any form aggravates the disease);
- diabetes mellitus while taking metformin.
Contrast-enhanced CT scans are not usually performed on children under 12 years of age.
Decoding the results
After the procedure, the following actions are performed:
- After 30 minutes, the diagnostician gives the finished images to either the doctor or the patient;
- the doctor performs a full analysis of the received images;
- a diagnosis is made (if the research data is insufficient, a referral for MRI or CT is issued);
- treatment is selected and an appropriate diet is prescribed.
Trying to treat the disease on your own and prescribing medication for yourself is highly discouraged, so as not to aggravate the situation.