Home — Services — Ultrasound — Ultrasound of the heart
- What is transthoracic cardiac ultrasound?
- Price
- Indications?
- What does it reveal?
- How is the procedure done?
- How to prepare?
- How to sign up
What is transthoracic cardiac ultrasound?
Cardiac ultrasound is a safe and reliable method for diagnosing heart disease. Unlike the well-known ECG (electrocardiogram), echocardiography provides a much more detailed, voluminous and accurate picture of the state of the cardiovascular system. However, both methods are quite actively used in modern medicine and can complement each other. An ECG records contractions of the heart muscle using electrical impulses and demonstrates the presence of problems such as ischemia, blockade, and angina. Echocardiography allows visualization of organs and vessels in a three-dimensional projection and reveals a wider range of pathological conditions.
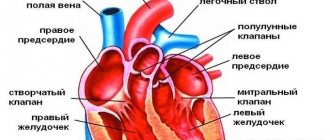
The method of transthoracic ultrasound of the heart is based on the use of ultrasonic waves, which, reflected from the internal organs and blood, transmit information about their condition to the computer, in particular, they allow one to assess the position of the heart, its size, tissue density, and features of the anatomical structure. ECHO of the heart also measures blood pressure, examines blood flow, the cavities of the atria and ventricles.
Echocardiography with Doppler analysis
Doppler echocardiography is a variant of ultrasound examination that allows one to evaluate blood flow (velocity and turbulence) in the cavities and large vessels of the heart. The method is based on the Doppler effect: the speed of an object affects the frequency of the supplied signal. This version of echocardiography is highly informative and safe, so it is mandatory for pregnant women and children.
Advantages of the method:
- non-invasive;
- fast processing of information in real time;
- accuracy.
The examination helps to identify:
- pathological blood flows;
- mitral valve prolapse;
- blood clots and cardiac aneurysms;
- defects, congenital and acquired.
Three main modes of echocardiography with Doppler analysis:
- Pulse-wave . Diagnostics of low-speed flows.
- Constant wave . Assessment of blood flow velocity in the aorta (diagnosis of aortic stenosis).
- Color mapping . Visualization of valve and turbulent flows at the site of blockage. Diagnosis of blood clots, aneurysms, atherosclerotic plaques, determination of the nature of the neoplasm.
When is an echocardiogram necessary?
Ultrasound is safe for health, has no contraindications or side effects, and can detect serious diseases in the early stages. Therefore, a preventive annual examination can be recommended to absolutely everyone. Moreover, its cost in medical treatment, even taking into account the use of the most modern equipment, remains quite affordable.
In addition, an ultrasound of the heart must be performed:
- patients who were previously diagnosed with cardiovascular, endocrine and immune diseases;
- obese;
- pregnant women;
- people over 50 years of age;
- hypertensive patients;
- professional athletes.
It will also be useful to undergo the procedure in cases where:
- headaches, dizziness, loss of consciousness;
- there is regular shortness of breath and swelling (it may also be a good idea to undergo an ultrasound of the kidneys);
- there was pain, tingling or a feeling of squeezing in the chest;
- cholesterol levels increased;
- there is a feeling of weakness and loss of strength;
- suffered chest injuries.
If you find yourself with any of the listed symptoms and you need to consult a doctor performing cardiac ultrasound (ECHOCG) in St. Petersburg or any other specialist, contact a medical specialist - write to us or call +7 (812) 611-33-03. We will select a convenient time for your appointment and answer any of your questions.
There are no contraindications to undergoing the procedure.
Interpretation of results and norms of EchoCG
Decipher the results of cardiac ultrasound yourself; there are many types of interpretations of pathologies, which only a specialist can understand.
Table of normal indicators
| Index | Normal value |
| Myocardium weight | 95–182g. |
| Myocardial mass index | · men – 70–93 g/m2. m: · women –71–81 g/sq. m. |
| Left/right ventricular volume | 35–57/9–26 mm |
| Right atrium volume | 19–40 mm |
| Ejection fraction | 55–60% |
| Blood volume per contraction | 0.06–0.1 l |
| Thickness of the wall and septum between the ventricles | No more than 11, but not less than 6 mm |
| Amplitude of the interventricular septum at the level of the middle third/at the upper point | 3–8–5–12 mm |
| Aortic diameter | 20–37 mm |
| Diameter of the pulmonary artery at the mouth/in the trunk | 18–24–30 mm |
| Blood speed | 17–27 sms |
The condition of the valves is also assessed to identify stenosis or insufficiency, and signs of reverse blood flow are determined. There is no fluid in the heart of a healthy person, no adhesions in the pericardium, no signs of proliferation of valve tissue.
All indicators are multiplied by coefficients that depend on the area of the body; the indices are entered into special diagrams.
- Myocardial mass is the norm, calculation and index, what does it mean?
Types of Echo CG and their differences
There are several types of cardiac ultrasound. Basically, methods are divided according to the method of access to the muscle organ.
- Classic or transthoracic form, through the anterior wall of the sternum. This is the most common option. Gold standard for primary diagnosis. The ultrasound sensor is placed on the chest, after which the doctor changes its position. To visualize tissues in different projections and from several angles.

- The second option is an ECHO study with contrast enhancement. In essence, it’s the same transthoracic ultrasound. But this time special substances are injected intravenously. They accumulate in blood vessels, tissues and enhance the reflection of ultrasonic waves. Makes the picture clearer. In general, the method differs little from the previous one. From a technical point of view, everything is the same. But with contrast you can get much more information.

- Finally, transesophageal echocardiography. Invasive research. Due to its high complexity, it is performed only in a hospital setting. Moreover, problems and unforeseen disorders are possible afterwards. It is considered a particularly accurate method compared to others. The technique is used if previous modifications have not produced results.

Another way of classification is by the nature of the study.
- ECHO at rest. Occurs especially often. This is a typical cardiography.
- Assessment of cardiac condition after exercise. Appointed in controversial situations.
What you need to know before having an echocardiogram
If you are referred for an echocardiogram, please bring a towel or diaper with you (which can be placed on the couch during the examination and used after the examination to remove any remaining gel). Try to arrive for the examination in advance (5-10 minutes) so that you have time to rest and the echocardiography is performed in a calm state. Be sure to take your ECG film (preferably no more than 1 month old). If you have several ECG films left, take them all. Previous EchoCG findings are also required if you have had this study previously; a report from your doctor (cardiologist or therapist), which may indicate the purpose of the echocardiography.
Progress of the study
The patient goes to the office of a functional diagnostics specialist. Next, the procedure is carried out according to the usual scenario for many, like a regular ultrasound.
- You need to lie down on the couch.
- The doctor will lubricate the chest with a special gel. It conducts ultrasonic waves better, so the picture will be more accurate.
- The specialist places a sensor and begins to study the anatomical area.
- During the procedure, the doctor changes the position of the scanner and examines the organ from different angles. Works in several modes. Do not be afraid of the strange sounds that the device makes. This is fine.
- During the scan, the specialist may ask you to hold your breath. Roll over on your side. The patient's job is to follow the doctor's instructions. After the procedure is completed, you can go home.
Other modifications differ. If a contrast study is prescribed, a standard ultrasound is first performed, then contrast is administered and the procedure is repeated. Everything takes about 10-20 minutes. Plus or minus. Transesophageal ultrasound of the heart requires more time.
The echocardiogram is given to the patient after another 10-20 minutes. Because a specialist must give an opinion. Sometimes a person receives only a diagnostic protocol, without the doctor’s explanation.
Indications for echocardiography
An echocardiogram or cardiac ultrasound is recommended if the following symptoms are present:
- Audible heart murmurs, rhythm disturbances;
- Chest pain;
- Symptoms of heart failure (eg, enlarged liver, swelling of the legs);
- Ischemia;
- If you have the following symptoms: fatigue, shortness of breath, lack of air, bluish skin around the lips, ears, arms and legs.
Unfortunately, echocardiography cannot be performed successfully and informatively in all patients. Penetration of ultrasound into tissue may be difficult in elderly people suffering from obesity and emphysema.
The method is non-invasive and painless. It is carried out using an ultrasound machine.
Decoding the results
After completion of the procedure, an echocardiographic study protocol is completed. Based on this document, anamnesis and data from other studies, the cardiologist forms the final diagnosis.
In the process of echocardiography, the following indicators are assessed:
- myocardial structure;
- condition of the valve apparatus;
- dimensions of the lumens of large vessels;
- vascular wall thickness;
- the presence of atherosclerosis;
- condition of the walls, partitions between the ventricles and atria;
- blood flow speed;
- pulmonary artery pressure.
Normally, echocardiography reveals:
- diastolic volume of the right ventricle – 9–25 mm;
- thickness of the posterior wall of the left ventricle in diastole – 6–11 mm;
- amplitude of movement of the posterior wall of the left ventricle in systole – 9.1–14.1 mm;
- thickness of the interventricular septum in diastole – 6–11 mm;
- aortic orifice diameter – 20–35 mm;
- left ventricular cavity at the end of diastole – 35–57;
- daily index – 2–4.1 l/m2;
- cardiac output – 3.5–7.5 l/min;
- the mouth of the pulmonary trunk is 1.8–2.4 cm; trunk – up to 3.0 cm;
- no signs of regurgitation;
- dysfunction of the papillary muscles, accessory chordae;
- valve leaflets are smooth, without vegetations;
- there are no clots or thrombotic masses in large vessels and in the cavity of the chambers;
- ejection fraction 55–60%;
- lack of fluid in the pericardium.
If all criteria are met or if there are minor deviations that do not affect hemodynamics, the following entry is made in the conclusion: “No echo pathologies were identified.”
During the study, the following pathologies can be identified:
- Congenital malformations: septal defects, patent oval window or Batalov's duct, tetralogy or pentade of Fallot. All these defects are characterized by the presence of abnormal blood circulation due to a defect in the vessel wall. Ultrasound reveals an echo-negative (dark) formation, through which abnormal communication between the parts of the heart occurs.

- Acquired defects: valve defects, presence of vegetations. In this case, the valve leaves do not close completely or grow together, forming a funnel. It is also possible to have vegetations - growths on the valves (the result of an inflammatory process).

- Dilated cardiomyopathy: an increase in the size of the chambers and a decrease in wall thickness are detected.
- Hypertrophic cardiomyopathy: pathological increase in myocardial mass and wall thickness.
- Signs of atherosclerosis: hyperechoic formations (light) are detected on the walls of blood vessels.
- Exudative pericarditis: the presence of excess fluid in the pericardial cavity.
It is important to understand that echocardiography is a complex and specific procedure. It is extremely difficult to decipher the results of the study on your own.
Who is the study contraindicated for?
Contraindications are minimal, but they still exist.
- Lung diseases. Because patients with respiratory failure find it difficult to lie still for 10-20 minutes.
- Deformation of the sternum. For example, a hump. In this case, there will be problems with visualizing heart tissue.
- Inflammatory processes of the skin of the breast.
- Mental disorders. Excluding adequacy. For example, exacerbation of schizophrenia.
Contraindications are not absolute. Doctors are considering options to perform the procedure.
Preparation
No special events needed. Conventionally, we can name the following requirements:
- The day before the test you should not smoke. Otherwise, the vessels will narrow and the doctor will detect false changes. In the coronary and pulmonary arteries.
- The same goes for alcohol. You should give up alcohol a few days in advance. To make the results more accurate.
- On the day of the procedure, you should not engage in intense physical activity. You need to follow a gentle regime. Peace is desirable.
- You must arrive at the appointed time. It is recommended to take a towel or disposable napkins with you. To remove excess gel after echocardiography.
Otherwise, no preparation is needed. You can do everyday, familiar things.
Reasons for referral for transnutritive echocardiography:
identification of possible blood clots in the cavities of the heart (especially in the left atrial appendage), which can be a source of systemic embolism; mandatory examination before restoring sinus rhythm in patients with atrial fibrillation with a paroxysm duration of more than 48 hours); assessment of the size, structure, degree of mobility and place of attachment of neoplasms (tumors) of the heart; identification of infective endocarditis and its complications; diagnosis of diseases of the thoracic aorta (dissecting aortic aneurysm, atherosclerotic lesions of the aorta and its complications); assessment of the valvular apparatus of the heart for acquired heart defects, including before the upcoming operation (condition of the leaflets, subvalvular structures, careful assessment of regurgitation); assessment of dysfunction of prosthetic heart valves (especially mitral prostheses); diagnosis of congenital heart defects, clarification of anatomical features before surgical treatment; monitoring during heart surgery; prolonged spruce fever of unknown origin.