general description
Electroencephalography (EEG) is a functional diagnostic method that allows you to assess the state of the human brain based on its bioelectrical activity; it is widely used in modern neurophysiology, neurology and psychiatry.
The EEG method is completely harmless, non-invasive, does not require special preparation for the study, is painless and highly sensitive. There are no contraindications to this method of functional diagnostics. Indications for EEG:
- Epilepsy. It is possible to identify the areas of the brain that are involved in the generation of epilepsy attacks and monitor the effect of antiepileptic drugs.
- In the presence of seizures of unknown origin.
- Frequent fainting.
- If a brain tumor is suspected (as a screening method).
- To establish a diagnosis in patients with dizziness, headaches, vegetative-vascular dystonia, increased or fluctuating blood pressure, neurotic disorders, signs of vertebrobasilar insufficiency.
- To assess the severity and recovery of brain function after traumatic brain injury.
- Patients with dyscirculatory encephalopathy.
- After brain surgery to control normal brain function.
- Inflammatory diseases of the central nervous system (meningitis, encephalitis, arachnoiditis, etc.).
- Acute and chronic cerebrovascular accidents.
- Paroxysmal behavioral disorders.
- Delayed mental and speech development of unknown origin.
- Endocrine diseases.
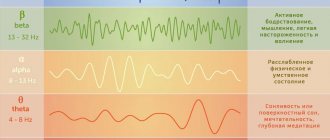
Depending on the frequency and amplitude on the EEG, waves are distinguished, denoted by Greek letters:
- Alpha (α) activity is detected when performing an electroencephalogram in a state of passive wakefulness and represents sinusoidal oscillations with a frequency of 8-13 Hz and an amplitude of 40-100 μV. Alpha activity in the mature brain is typically modulated in spindles and predominates predominantly in occipital regions.
- Beta (β) activity is an oscillation with a frequency of 14-40 Hz and an amplitude of up to 15-20 μV. It is detected mainly in the anterior parts of the brain during active wakefulness. In the structure of beta activity, low-frequency (with a frequency of up to 22-24 Hz) and high-frequency (with a frequency of more than 22-24 Hz) activity is distinguished.
- Mu (μ) activity is detected in the central regions of the brain with a predominance in the area of the Rolandic sulcus (associated with proprioceptive sensitivity). It corresponds in frequency and amplitude to alpha activity, but has a characteristic arch-like shape.
Rhythms and phenomena that are pathological for an adult include:
- Theta (θ) - activity - slow-wave activity with a frequency of 4-7 Hz of varying amplitude, increasing with emotional arousal and during sleep. The appearance of activity on the EEG at other time intervals indicates a decrease in the level of functional activity of the cortex and the entire brain as a whole.
- Delta (Δ) - activity - slow wave activity with a frequency of 1-3 Hz of varying amplitude, most pronounced during sleep. The appearance of activity on the EEG at other time intervals indicates a decrease in the level of functional activity of the cortex and the entire brain as a whole.
- Epileptic (epilentiform, convulsive, convulsive) activity.
- A peak or spike (from the English spike) is a peak-shaped potential. Its duration is 5-50 ms, the amplitude exceeds the amplitude of background activity and can reach hundreds and even thousands of microvolts.
EEG in the diagnosis of epilepsy
EEG is the first and often the only neurological outpatient study that is performed during epileptic seizures. With EEG you can:
- identify areas of the brain involved in triggering seizures;
- monitor the dynamics of the action of drugs;
- resolve the issue of stopping drug therapy;
- identify the degree of brain dysfunction in interictal periods.
Epileptic activity characterizes the state of the brain outside of an attack, and is distinguished:
- adhesions;
- sharp waves;
- spike-slow wave complexes;
- complexes sharp wave - slow wave;
- multiple spikes followed by slow waves.
In 90% of patients with epilepsy, EEG changes can be detected.
EEG in the diagnosis of neoplasms
- If the tumor is located close to the surface of the brain and affects mainly the cortex and subcortical structures, changes in the EEG occur on the affected side. Local pathological changes are noted in the area of tumor projection - inhibition of the alpha rhythm, increase in the amplitude of delta waves.
- Intracerebral tumors cause significant general changes in the EEG, masking focal disturbances of biopotentials. To more clearly identify focal pathology, EEG studies are indicated after dehydration and hormonal therapy, leading to a decrease in diffuse slow waves.
- For tumors of temporal localization, EEG diagnosis indicating the focus of pathological electrical activity in the temporal region is most accurate (up to 90%). As a rule, focal beta activity is observed.
EEG for vascular disorders
- When the lesion is localized in the cerebral hemispheres, in most cases (80%) the EEG shows pronounced interhemispheric asymmetry due to the predominance of pathological forms of activity in the affected hemisphere; At the same time, focal changes in the bioelectrical activity of the brain in the corresponding area of the lesion can be recorded. In 20% of cases, in the presence of foci in the hemispheres, the EEG reveals only diffuse changes of varying degrees of manifestation.
- With brainstem localization of the lesion, changes in the EEG are not as significant as due to damage to the cerebral hemispheres. The structure of the EEG is changed more clearly with damage to the upper parts of the brain stem, either by the type of increased rhythm desynchronization reaction, or with the presence of bilateral synchronous a-, Θ-activity. As a result of damage to the lower parts of the brain stem, EEG changes are insignificant.
EEG after brain injury
- With a mild injury, there may be no changes or only minor disturbances in brain potential indicators are recorded in the form of increased frequent oscillations and uneven α-rhythm. In this case, there may be interhemispheric asymmetry, as well as electrographic signs of damage to the brain stem.
- In severe traumatic brain injury (with deep loss of consciousness), the EEG is characterized by dominance in all areas of high-amplitude Θ-waves, against the background of which discharges of rough Δ-activity are determined (1.5-2 oscillations per 1 s), indicating significant changes in the functional states of the brain and, first of all, its medial structures.
In these conditions, the greatest value of an EEG is not in confirming the diagnosis—the injury itself is “not visible” during examination. But repeated EEG studies help assess the speed and completeness of the disappearance of signs of brain dysfunction.
Synchronization and desynchronization of EEG signals
Synchronization of brain potentials is a process in brain tissue when a significant number of nerve elements, entire fields of nerve cells, or even large systems of nerve formations begin to work in a single rhythm and in phase. Electrical summation occurs over the amplitude of many individual processes, apparently occurring in different circuits of neurons and in different parts of the brain with small amplitudes. The result will be a relatively simple and clear rhythm recorded. It is assumed that certain physiological phenomena correspond to this electrical synchronization, for example, equalization of lability, generalization processes, etc.
Synchronization is also observed in response to certain stimuli.
The opposite process is called desynchronization. This is a disruption of the synchronous functioning of large masses of nerve cells as a result of any internal reasons (changes in the course of metabolic processes) or external influences, for example, when a particular stimulus is turned on (which, of course, is also associated with a change in the course of metabolic processes in nerve cells) . Typically, slow oscillations are susceptible to desynchronization. In this case, different nerve units that worked in phase experience, for some reason, a phase shift.
Another type of desynchronization is as follows. The slow rhythm in all nerve units is replaced by fast rhythms of different frequencies. An example is the classic case of alpha rhythm suppression. Inhibition means a decrease in signal amplitude. Another type of desynchronization is a decrease in the frequency of synchronous oscillations in different foci of excitation, and this decrease occurs in different ways. Then the total encephalogram will represent a desynchronized signal with an undetermined frequency. Such desynchronization is observed in humans during a drowsy state, when the alpha rhythm stage is replaced by the sleep spindle stage.
Artifacts during EEG recording
Artifacts during EEG recording are of physical and biological origin. The physical causes of artifacts are alternating current interference with a frequency of 50 Hz, less often 100 Hz, poorly pressed electrodes, or disturbances in the contact of the electrodes with the skin, for example, the paste has dried out, the electrodes have oxidized, etc.
Artifacts of biological origin may be due to the fact that muscle potentials, which are difficult to distinguish from rapid fluctuations in brain potentials, are recorded on the electroencephalogram. Sometimes the cardiogram signal is superimposed on the EEG. This can be detected by the regular appearance of sharp peaks on the EEG in time with the heartbeats. Galvanic skin reflex in the form of a smooth shift of the zero recording line. Eye movements and blinking, that is, the EOG signal can also be recorded on the EEG. The EEG potential is small, ranging from a few microvolts to 500 μV.
Electrodes used for EEG recording.
When the German doctor G. Berger began recording a human electroencephalogram for the first time in 1929, he used electrodes that stuck into the scalp (needle electrodes). He soon abandoned them and began using foil electrodes with a flannel pad moistened with a solution of table salt. Disc and wire electrodes are now used. If silver electrodes are used, it is better to chlorine them to protect them from polarization, but this is not necessary, since the constant polarization potential is not amplified by an alternating current electroencephalographic amplifier. The disk or wire is wrapped in a thin layer of cotton wool and gauze and moistened with a solution of table salt (5-10% solution). The electrodes are attached to the subject's head with an aphid collodion bandage. They are used on areas not covered with hair. Another type of electrodes is in the form of cups, the space in which is filled with electrically conductive paste. The diameter of the electrodes is 10 – 12 mm. They are made of silver. There is a hole in the cup for additional paste pressing. A fabric ring is sewn along the edge of the cup to prevent the metal from touching the koi. The electrode is also strengthened with adhesive tape or collodion.
There are also bridge electrodes. They are widely used, although less reliable in use. But there is no need to remove hair from the surface of the head. Ear electrodes are made in the form of a clothespin or clip. Contact is made either with a disk electrode wrapped in gauze soaked in saline solution, or with a disk with electrically conductive paste. The electrodes should fit snugly on the ear, but not cause discomfort, much less pain. The nose bridge electrode resembles a spectacle frame.
Helmets
Helmets for EEG recording are made of elastic rubber bands, the tension of which is adjustable. Bridge electrodes are either simply slipped under these cords, pressing them to the head, or cling to them with special hooks.
Application of EEG in space flight (based on materials from the book by R.M. Baevsky “Physiological measurements in space and the problem of their automation”).
Electroencephalography is used for the examination and selection of pilots and astronauts, as well as for the purpose of monitoring a person’s state of consciousness and mental stress during flight. American researchers widely use the capabilities of EEG to assess the tension of an astronaut during flight. Soviet scientists were the first to use EEG to record the condition of astronauts. Spontaneous brain activity was recorded on the Vostok spacecraft. Frontal-occipital leads were used. The resulting EEG is called a survey EEG. The advantage of this lead is that there is minimal interference. Interference occurs from opening the eyes, clenching the jaw, turning the head, moving the arms and body, and blinking. This lead is also used to monitor the condition of patients during surgical operations under anesthesia.
Electroencephalography is carried out during professional medical examinations of pilots, and in this case a rheoencephalogram of the head (brain rheogram) is also taken. Let us remember that this is a measurement of the complex electrical resistance (impedance) of the head, which provides information about the state of the blood vessels of the head. Electrodes for recording the rheogram are installed on the forehead and behind the ears. Rheoencephalography is used to study hemodynamics (i.e. blood movement) of the brain. At the same time, an ECG is recorded, and the rheoencephalogram is time-linked to it.
There are three main areas of use of electroencephalography in astronautics.
1) When selecting and during the training of cosmonaut pilots, EEG is used as an indicator of the reaction of the central nervous system to the action of various functional tests that simulate the influence of individual flight factors.
2) EEG is used as the most important indicator, which is included in the symptom complex that determines the general condition of a person during the development of acute pathological conditions.
3) To assess the levels of wakefulness and sleep of an astronaut (in particular, sleep phases) during different periods of the flight.
The last two cases arise, for example, when performing work associated with risk and stress (responsible work on orbit correction, going into outer space or onto the surface of another planet, etc.).
For leads, electrodes mounted on the inner surface of the helmet are used. Contact electrically conductive pastes and depilatory agents were used. On the “cosmic” electroencephalogram, the alpha rhythm, beta rhythm, delta and theta rhythms are clearly visible. In the first hours and days of flight, high-frequency components (beta rhythm) predominate. American investigators note an increase in the beta rhythm during flight and an increase in the cross-correlation of signals from the leads during sleep.
The most common method of automatic EEG processing is to determine the spectral density of biopotentials using spectrum analyzers. There are also a number of simple but EEG-specific methods.
1) Recording the envelope with compression and summation of biopotentials.
2) Determination of the arithmetic mean values of all amplitudes for a given time.
3) Determination of the number of waves with an amplitude of more than 50 μV.
4) Calculation of the asymmetry coefficient, which is the ratio of the sum of the durations of the ascending phases of the EEG to the sum of the durations of the descending phases for a given time.
Cross-correlation analysis is used to assess the functional connectivity between brain regions.
EEG method and psychology (based on the book by G.T. Kaminskaya “Fundamentals of Electroencephalography” 1989)
Researchers have always tried to find a connection with the type of EEG signal recording and any psychological qualities of a person. Success was not achieved here, but some useful information about the characteristics of the EEG of healthy people was obtained. Here is what is known about the features of the manifestation of the alpha rhythm on the human electroencephalogram.
There are areas on the EEG recording where the alpha rhythm persists for several seconds. In this case, beats of alpha rhythm oscillations are observed, which consist of alternating areas of decreasing and increasing the amplitude of oscillations. These beats are caused by a slight change in frequency within the alpha frequency band (8 – 13 Hz). Typically, the alpha rhythm is widely distributed throughout the brain structures. It is also well recorded in various subcortical formations. To characterize the alpha rhythm, an indicator called the alpha rhythm index is used. This is the fraction of time during which the alpha rhythm is recorded in the selected recording segment. This is sometimes called the percentage of alpha time. The duration of the entire EEG recording is called an EEG epoch. The most pronounced is the alpha rhythm of the occipital areas of the cerebral cortex. The individual EEG characteristics of carved people are quite stable.
There are different classifications of people according to alpha rhythm. There are people with large and moderate values of alpha rhythm indices in various areas of the cortex. At the same time, a large and moderate amplitude of alpha waves is also observed. In other individuals, the EEG is characterized by polyrhythmicity and a low alpha index, with alpha waves having low or moderate amplitude and appearing in different areas of the cerebral cortex simultaneously. The general conclusion of various researchers is that the alpha rhythm is closely related to the activity of the visual analyzer.
It is known that the alpha rhythm is constantly present in the EEG in 15% of normal adults, in 10% it is not detected, and in 70% it appears at rest with eyes closed, i.e. in the absence of visual information. Absolutely blind people have no alpha rhythm when they are awake. If a person is in absolute darkness, then the intensity of the signal from the occipital region (where the focus of the alpha rhythm is located) decreases significantly.
The alpha rhythm is naturally associated with memory. Memorizing words turns out to be less effective if they are presented to the subject against the background of the most pronounced alpha rhythm compared to memorizing them against the background of polyrhythmic brain activity, i.e. with desynchronization of electroencephalographic signals.
Depression (destruction) of the alpha rhythm occurs under the influence of various sensory and non-sensory factors. The alpha rhythm disappears when opening the eyes, even in the dark, if the subject is trying to see something. Emotions such as anxiety and fear also cause alpha depression.
Various types of mental activity, such as visual-motor reactions, solving chess problems, multiplying numbers in the mind, are accompanied by depression of the alpha rhythm of varying depth with different spatial distribution of the focus of activity in the cerebral cortex. Depression of the alpha rhythm is an obligatory component of the indicative reaction. These facts give reason to assume that it is not the irritation itself, but the attraction of attention to the stimulus that causes depression of the alpha rhythm. This conclusion, expressed by G. Berger, was later confirmed.
About the performance of a human operator
The alpha rhythm, which alternates with beta waves and a small number of theta waves, characterizes maximum performance when performing complex operator activities. If the signal to action is given against the background of high alpha activity in the occipital region, the quality of the operator’s work deteriorates. This is expressed in an increase in the total error when performing the task. It has also been established that near-threshold stimuli are better distinguished against the background of low-amplitude alpha waves.
When recording EEG in space flight, a stagnant exaltation of the alpha rhythm is observed during prolonged physical inactivity of the astronaut in weightlessness. Almost all characteristics of the alpha rhythm and only the alpha rhythm are genetically determined.
Sleep spindles (or sigma rhythm) are observed during light sleep or under anesthesia. Their frequency is 14-16 oscillations/s, and the amplitude is 30-50 μV. In deep sleep they change into slower delta waves. The spindle rhythm is widely distributed throughout the brain structures. In the cerebral cortex, the sigma rhythm is confined to the anterior areas. Here, potential oscillations at this frequency, having a maximum amplitude, are recorded. Less pronounced oscillations can be traced to almost all areas of the neocortex. Of the subcortical structures, fusiform activity is well expressed primarily in the thalamic nuclei (both specific and nonspecific). Fusiform activity is also recorded in the reticular formation of the brain stem, in the striopallidal complex and in the hypothalamus.
Stress rhythm
The stress rhythm is called the theta rhythm (4-7 oscillations/s). It occurs not only in humans, but also in primates and even in animals with a low degree of brain corticalization, such as the rabbit and rat. In humans, the theta rhythm is detected in childhood, intensifying during emotional changes, as well as when the brain is damaged, when the brain is involved in the pathological process, especially when deep structures are damaged. The use of sensory stimulation against the background of the theta rhythm, as a rule, causes its inhibition. If consciousness is impaired in this case, the EEG rhythm remains unchanged. A normal EEG usually shows either irregular slow activity or slow waves with a theta period (4-7 oscillations/s). Their amplitude can vary from 20 to 50 μV, and more often it is 20-30 μV.
Beta rhythm
The frequency of beta waves is from 15 to 30 vibrations/s and they go along with gamma waves, whose frequency is more than 30 vibrations/s. The amplitude of beta waves is 2-4 times less than that of alpha waves, i.e. for beta waves it is 10-50 µV, and for alpha waves it is ~50-100 µV. Therefore, for many people, the beta rhythm is lower than the level recorded by devices. The shape of the beta rhythm oscillations is irregular, jagged. It is difficult to judge the continuity of beta waves because they overlap or are masked by alpha waves (and pathological waveforms). Often beta waves are seen between the spindles of alpha waves. Their amplitude increases when alpha activity is suppressed by external stimuli. Beta waves are most regular and better expressed in the anterior parts of the hemispheres.
Slow waves
These waves with a rhythm below 4 oscillations/s are characteristic of childhood. Only by the age of 12–15 is the alpha rhythm formed. This slow rhythm is like a stage in the development of the alpha rhythm in children. It, like the alpha rhythm, is better expressed in the occipital areas and also responds to eye lighting. With developmental delay, for example, in infantile young people, more or less slow rhythms in the EEG can be observed. Delta waves occur in healthy adults during sleep. Slow waves often occur as a type of pathological electrical oscillations, arising, for example, as a result of disturbances in cellular metabolism due to endocrine disorders, traumatic brain injuries, tumors and inflammatory processes of the brain.
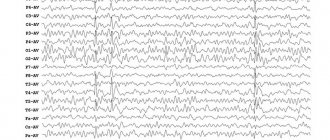
Norms
Characteristics of a normal EEG of an adult who is in a state of wakefulness: in the majority (85-90%) of healthy people, when closing their eyes at rest, a dominant alpha rhythm is recorded on the EEG. Its maximum amplitude is observed in the occipital regions. Towards the frontal lobe, the α rhythm decreases in amplitude and combines with the beta rhythm. In 10-15% of healthy subjects, the regular alpha rhythm on the EEG does not exceed 10 μV and high-frequency low-amplitude oscillations are recorded throughout the brain. This type of EEG is called flat, and EEG with an oscillation amplitude that does not exceed 20 μV is called low-amplitude.
Japanese equipment of expert level

The equipment is intended for conducting EEG studies in private clinics, epilepsy research centers, sleep institutes and scientific laboratories. To conduct research, an EEG cap is used (for children, newborns and adults) or individually glued electrodes.
We will conduct video-EEG monitoring at your home or at any other department of the medical hospital.
Diseases for which a doctor may prescribe electroencephalography
Focal brain injury
With mild traumatic brain injury, changes in the EEG may be absent or only minor disturbances in brain potential indicators are recorded in the form of increased frequent oscillations and uneven α-rhythm. In this case, there may be interhemispheric asymmetry, as well as electrographic signs of damage to the brain stem.
Juvenile absence epilepsy
Using an EEG for epilepsy, you can identify areas of the brain that are involved in the generation of epileptic attacks and monitor the effect of antiepileptic drugs. In 90% of patients with epilepsy, EEG changes can be detected.
Tumor of the temporal lobe of the brain
For tumors of temporal localization, EEG diagnostics indicating the focus of pathological electrical activity in the temporal region is most accurate (up to 90%). As a rule, focal beta activity is observed.
Comfortable conditions for patients
The clinic has 2 spacious rooms with good sound insulation, equipped with everything necessary for a comfortable long stay:
- a patient bed with the ability to transform into a chair, equipped with a table for eating;
- bed and chair-bed for accompanying persons;
- air conditioner;
- heater;
- TV;
- Internet Wi-Fi;
- fridge;
- microwave;
- kettle;
- sink;
- utensils for eating.
How is video-EEG monitoring performed?
Patients come to the clinic by appointment. You will be met by the administrator and taken to a separate soundproofed room, where video-EEG monitoring will be carried out. The specialist will conduct a consultation, ask questions about the medications you are taking, complaints, how the disease is progressing, then put an electrode cap on your head or apply collodion electrodes. EEG recording is carried out according to the following scheme - data is recorded in wakefulness before sleep, during sleep and after sleep. Also, before and after sleep, functional tests are carried out (hyperventilation - deep breathing test and rhythmic photostimulation).
Depending on the condition and needs of children, the sequence of video-EEG monitoring may vary slightly. The examination can be performed without sleep or only while asleep. During monitoring, the patient can feel free - play, watch TV, read books. Follow the recommendations and instructions of medical personnel. The child's parents or accompanying persons are obliged to monitor the behavior of the subject. It is necessary to ensure that the patient is within the field of view of the video camera and does not fall into the video recording zone during an attack. If an attack occurs, you must click on the button that will mark the event on the record and inform the doctor that the patient is having an attack; it will also be necessary to describe the attack on a special sheet issued at the beginning of the study for marking paroxysmal states and indicate the approximate time. After video-EEG monitoring is completed, the cap or electrodes are removed. You can go home.