There are many methods for imaging brain pathologies. These include:
- MRI (including functional MR spectroscopy, MR angiography and diffusion tensor imaging);
- CT (computed tomography);
- EEG (electroencephalography);
- PET (positron emission tomography);
- MEG (magnetoencephalography);
- Echo-EG (echoencephalography);
- Rheo-EG (rheoencephalography);
- Electrical impedance tomography;
- Thermoencephaloscopy;
- Luminescent neuroimaging.
Magnetic resonance imaging and electroencephalography are most often used in diagnosing brain diseases.
Work principles
To see the difference between magnetic resonance imaging and electroencephalography, consider the principle of operation. During MRI, hydrogen atoms found in the human body are exposed to electromagnetic waves. The vibrations of atoms affected by a magnetic field make it possible to assess the condition of the organ under study. The procedure is absolutely painless and there is no radiation exposure. During the procedure, the patient must lie still.
EEG of the brain is the latest research method that uses an electroencephalograph. This device records neuron impulses, allowing the diagnosis of tumors and injuries. This type of research is carried out in a sitting or lying position in a separate room without light. Brain activity is recorded by a helmet with electrodes that are placed on the patient's head. The procedure has no contraindications and is completely painless.
How these studies are carried out - a comparison of operating principles
The algorithms for MRI and EEG procedures of the brain differ significantly.
When performing a tomography, the patient is placed on the tomograph conveyor table, and his head is fixed to ensure complete immobility. Being in this position, the patient on the couch enters the tunnel of the device, where the “reading” will take place. The scan takes about 30 minutes, but if the diagnosis is carried out with contrast, it takes about one hour. The procedure is painless, but requires special psychological preparation, since lying motionless in a cramped, enclosed space is morally very difficult. As a result, the doctor receives images showing an organ with pathological changes. Since the image can be represented in three dimensions, specialists can obtain the most detailed information about the object being studied.
To conduct an EEG, a cap with suction cups that are sensitive to electrical impulses is placed on the head. The diagnosis takes place in a regular office, and the patient does not have to sit absolutely still. The main thing is to try to remain calm, since the manifestation of emotions negatively affects the reliability of the result. An EEG can determine the functional state of the brain in 10-15 minutes; the procedure is completely painless. The result of the study is a graph printed on paper that can only be read by a specialist.
Diagnostic cost comparison
The described forms of research are paid services, but despite the fairly high price, they are very popular due to their exceptional information content.
The cost of an MRI in a private clinic will be approximately 5,000 rubles; the price may increase if a contrast agent is administered during the study. If a sedative is additionally used, the price increases by about 2,000 rubles.
The price of an EEG will be approximately 1500-3500 rubles, which depends on the level of the clinic and the quality of the equipment.
What MRI Can't Visualize
Magnetic resonance is based on the interaction of hydrogen molecules that are contained in any tissues or vessels. Therefore, brain images show structures and a clear pattern of tumors and hematomas. The main feature of the method is that the scanner captures the image in real time, but does not show changes in dynamics. Therefore, MRI does not show:
- presence of mental illness;
- level of functionality of different centers responsible for speech, thinking, memory;
- does not prove the patient is feigning illness;
- does not give clear reactions to certain stimuli.
MRI of the brain shows inflammation or damage to nerve fibers, but does not provide information about nervous disorders in schizophrenia and epilepsy.
How does MRI differ from EEG?
The EEG method is based on recording the total electrical activity of brain neurons removed from the surface of the scalp. As a result of alternating excitatory and inhibitory potentials, waves appear in cortical neurons, which are recorded through special electrodes. The main types of waves recorded when recording an EEG: alpha waves (rhythm in a state of quiet wakefulness, best expressed in the occipital regions), beta waves (rhythm in a state of active wakefulness, expressed in the frontal lobes), gamma waves (rhythm of the most concentrated attention), delta waves (deep sleep rhythm).
The principle of studying the brain using magnetic resonance is, in turn, based on the ability of the electromagnetic field of the tomograph to set in motion hydrogen atoms in tissues. Different tissues have different amounts of hydrogen, and the device detects this difference using special quantitative sensors. The brain is 90% water (and therefore hydrogen), making it an ideal subject for MRI scanning.
What does EEG reveal?
The procedure is necessarily prescribed for the following brain pathologies and patient complaints:
- frequent dizziness;
- loss of consciousness with stable blood pressure;
- speech disorder;
- pain after a stroke;
- hormonal disorders affecting brain function;
- panic attacks;
- comprehensive examination for cerebral palsy or autism;
- chronic insomnia.
Using an EEG, the doctor determines which areas of the brain are affected by injury or infection. This facilitates further diagnosis and becomes the basis for CT or magnetic resonance imaging.

MRI differs from EEG of the brain in the clarity of the image for tumors. While the electroencephalograph is operating, the device receives signals indicating the possible presence of formations. But they do not show the structure, the place of formation. But the procedure helps to understand how the pathology affected the functioning of the brain: often with oncology, patients do not feel pain, but complain of insomnia, irritability, and changes in behavior.
Advantages and disadvantages of methods
Both methods are safe and are carried out repeatedly to make an accurate diagnosis.
But each option has positive aspects and disadvantages - let's talk about them in more detail.
MRI
We list the advantages and disadvantages of magnetic tomography:
- Advantages - a powerful device provides a detailed image of the scanned area. This helps to identify the pathological area and assess the condition of surrounding tissues and blood vessels.
- Disadvantage - the study is carried out only in the diagnostic room, time is limited. The tomograph does not show foci of excitation, procedures are prohibited for pregnant women, the presence of braces, metal crowns, a pacemaker, and an insulin pump.
EEG
Pros and cons of EEG:
- Advantages include bedside testing. The procedures can be carried out over a long period of time and a sluggish pathology can be recognized. The device shows neural activity.
- Disadvantages - the doctor does not see tissue structures, there is an error in determining the lesion. Minor pathological changes go unnoticed.
Differences between methods
To compare which is better for the patient - MRI or EEG, a review of the differences between each of the recommended methods helps:
- With MRI, the doctor determines the physical structure of the brain, the exact location of the tumor and its boundaries. EEG evaluates the quantity and quality of biopotential, areas with increased excitability or spasms.
- An MRI scanner makes layer-by-layer sections showing the location of blood vessels, blood supply, and inflammatory foci. EEG records the activity of certain centers when the psyche is exposed to stimuli: a bright flash of light, a loud sound or a certain melody.
Both methods are safe for the patient and are used in diagnosing the same diseases. But they give different results and data that show the problem from the emotional and physical side. An electroencephalogram is better than an MRI in determining the degree of brain development. Therefore, it is recommended for children with cerebral palsy, autism, and speech delay.
WHAT DOES RESEARCH DETERMINE?
The difference between brain EEG and MRI can be understood by analyzing their diagnostic capabilities. MRI is used for suspected multiple sclerosis, vascular pathologies, tumors, brain inflammation, and congenital abnormalities. The following is revealed:
- inflammation in membranes and tissues;
- microscopic foci of multiple sclerosis;
- clarified boundaries and location of tumors, hematomas, cysts and other space-occupying processes;
- affected areas of the medulla, vascular malformations;
- spectral power of brain activity rhythms;
- features of blood circulation, stenosis, blood clots, areas with atherosclerosis, aneurysms;
- epileptogenic focus;
- areas with acute disruption of blood supply;
- the state of the white matter pathways.
Using an encephalogram, mental disorders, epilepsy, brain tumors, and central nervous system disorders are diagnosed. Using this method you can install:
- non-elliptical or epileptic seizure with specification of its type;
- dynamics of drug action;
- epileptogenic focus;
- changes in waves when the tumor is on the surface;
- brain functionality, stage of dysfunction (in Alzheimer's disease, schizophrenia, dementia);
- development of ischemic stroke;
- lesions of deep brain structures.
MRI cannot detect disorders of the psyche and brain functions. An EEG establishes the presence of organic lesions, including tumors with their localization, but does not make it possible to assess their nature and precise size.

Another diagnostic method is ECHO EG, echoencephalography. This is an ultrasound examination to identify pathologies of the central nervous system and blood vessels, in which the ultrasound wave is reflected from the cranial bone, brain and membranes. The main indication is a suspicion of displacement of intracranial structures; the following is revealed:
- hematomas inside the skull;
- abscesses;
- neoplasms;
- strokes.
ECHO EG does not allow one to accurately establish the pathology; it only indirectly indicates it. In parallel, an EEG or MRI should be performed.
Review of contraindications
Each research method has contraindications. For EEG this is:
- Damage to the scalp (absolute contraindication);
- Violent patients. This is a relative contraindication: an EEG can be done if a sedative is administered.
For MRI this is:
- Pregnancy in the first trimester;
- The patient's body weight is above 130 kg;
- Metal structures in the study area. We are talking only about steel; titanium and other metals that are not ferromagnetic are not contraindicated;
- Gadolinium intolerance (with contrast-enhanced MRI);
- Claustrophobia and other mental disorders in which the subject cannot lie without moving (in this case, the patient can be given a sedative);
- Having a pacemaker or device installed in the middle ear (the only absolute contraindication of all).
It can be seen that in case of a traumatic brain injury, one can only undergo examination with a tomograph, while in the presence of a pacemaker, only an EEG can be done. Electroencephalography also does not cause attacks of claustrophobia. Another advantage of the method is the absence of weight restrictions, since the patient will not be on a table, but on a regular chair or couch.

Both methods do not require preparation for the study, but with the caveat that the patient must come to the EEG in a good mood and well-rested. Otherwise, the diagnosis may give incorrect results.
Pregnancy is not a contraindication for MRI and EEG, since human organs do not receive radiation during diagnostic procedures. Both methods are safe for both mother and baby.
Limitations to the study
First, we note general contraindications for EEG or MRI of the brain:
- Severe head injury - if soft tissues are damaged and there is bleeding.
- Mental disorders and intoxication - in this case there is a risk of inappropriate behavior of the patient, interruption of the procedure or damage to equipment.
EEG no longer has any contraindications, the method is safe and is carried out according to the protocol.
MRI has a wider list of restrictions - the study is prohibited in the following conditions:
- first and third trimesters of pregnancy, lactation;
- braces, metal crowns;
- a pacemaker in the body or an insulin pump;
- contrast intolerance;
- severe obesity;
- claustrophobia.

The last contraindication is considered relative; with minor claustrophobia, the study is carried out if the patient is able to overcome fear.
Diagnostic cost comparison
EEG and MRI are paid diagnostic procedures, as they are carried out using innovative, expensive equipment. Let's look at the prices offered by clinics for brain research:
- EEG – from 1600 to 5700 rubles, depending on the newness of the equipment and the reputation of the clinic.
- An MRI costs an average of 5,000 rubles, and when examining the blood vessels of a person’s brain or detecting tumors, MR diagnostics can cost 7,000-8,000 rubles, depending on the amount of contrast agent administered.
- An EEG and MRI with the administration of a sedative will cost 2000-6000 rubles more.
- The cost of the procedures will increase by another 500-1000 rubles if the results of the study are recorded on electronic media (disk, flash drive).
The legislation provides for some cases for free EEG and MRI under the compulsory medical insurance policy. In other situations, the patient pays for the procedures.
There are many methods for diagnosing brain diseases, so the question is which is more effective: MRI and EEG. This is a case where there is no clear answer, because these studies are designed to study the organ from two different “sides”. Electroencephalography will accurately identify functional capabilities and only suggest the presence of pathologies in different brain structures. And magnetic tomography accurately diagnoses the localization of brain tissue damage: the presence of a tumor, necrosis, inflammation. But tomography only suggests the presence of mental and cognitive disorders. Thus, these are two procedures that do not replace, but complement each other.
SOURCES: https://diagme.ru/mrt/golova-i-sheya/eeg-ili-mrt https://proskopiyu.ru/metody/mrt-ili-eeg-golovnogo-mozga.html https://mrtdom. ru/diagnostika-mrt/mrt-golovy/eeg-ili-mrt-golovnogo-mozga https://mrtcentre.ru/article/chto-vybrat-dly-obsledovaniy-golovnogo-mozga-mrt-ili-eeg
Computer electroencephalogram
: Reading time:
EEG is the main type of instrumental diagnostics in modern psychiatry
In 1929, Hans Berger was the first to record electrical potentials of the brain from the surface of the human head non-invasively, i.e. bloodless electrodes - this is how a new scientific and practical diagnostic direction appeared - electroencephalography.
What is interesting is that G. Berger and his followers immediately tried to use EEG of the brain to search for the causes of various mental disorders - for this they recorded EEGs from mentally ill people and tried to find this or that mental illness in the features of the EEG “pattern”. The search for EEG signatures of schizophrenia, depression and many other diseases continues at the present time, however, back in 2013, the US National Institute of Mental Health (NIMH), the main grant holder of scientific research in psychiatry in the world, recognized such a “frontal” approach as scientifically inadequate vision and announced the cessation of funding for this type of research.
In 2021, depression was recognized as a major factor in mental ill health and disability—according to WHO estimates, up to 500 million people worldwide suffer from this disorder. Statistical reports show colossal losses associated with disability due to depression. However, the problems with diagnosing and treating depression are not only not improving, but in general are becoming more complex and confusing. These difficulties begin already in the diagnostic manuals and textbooks themselves (DSM-5, ICD-10), in which depression is present both as an independent disorder and as “other, unspecified, comorbid, etc.” types of depression. One of the reasons for this state of affairs is the lack of clear objective diagnostic criteria. And this applies not only to depression, but to almost any mental disorder.
Despite the emergence of increasingly new powerful diagnostic methods, such as positron emission tomography (PET), nuclear magnetic tomography (MRI), functional MRI, torsion tomography, etc., interest in traditional electroencephalography (EEG) not only does not fade, but is increasingly increasing, and thanks to such properties as non-invasiveness, relative cheapness, high temporal resolution and “hybridization” with computer technologies, as a result of which the modern computer modification of EEG arose, it has become a leader in widespread everyday practice. This was also facilitated by numerous scientific fundamental studies, which resulted in the formation of a modern understanding of abnormal patterns of electrical activity of the brain in various mental diseases - endophenotypes or EEG phenotypes.
What is the computer EEG technique, what procedures does it include and how does it differ from the traditional paper EEG with which it all began?
In a fundamental sense, EEG is a recording of electrical potential fluctuations from the surface of the head, which are generated by a huge number of nerve cells in the brain during their work. These potentials are very weak, so special equipment is required to register them. We are talking about special amplifiers of electrical signals, which are the main element of the so-called electroencephalographs. Electrodes that are installed on the scalp are connected to the inputs of these amplifiers - they are the ones who pick up weak electrical signals that generate cortical neurons.
From the electrodes, the neural signal enters the amplifier, is amplified, and then its fate varies depending on the generation of encephalographs. In the pre-computer era, this signal was simply recorded on paper in the form of a regular EEG, and that was practically the end of it - the clinician simply looked through kilometers of such paper tapes with the recorded EEG and, based on his knowledge, made conclusions and formulated clinical conclusions.
With the advent of computers, the fate of the neural EEG signal has changed greatly - in order to be entered into a computer, it is first converted from analog to digital form (ADC or analog-to-digital converter), and then, in the form of a sequence of zeros and ones, it is entered into the computer for subsequent processing. Types of subsequent computer processing of digitized EEG are constantly developing and improving, and today among them there are several types of hierarchically built on top of each other techniques that ensure completeness and depth of analysis.
First of all, these are the most basic computer techniques that essentially duplicate some important functions of analog electroencephalographs - for example, outputting and drawing an EEG curve on a computer monitor screen. But even in this case, the use of a computer significantly enhanced the capabilities of this stage - it became possible to measure various EEG parameters (amplitude, latency, etc.) almost instantly using any set of channels.
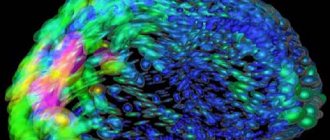
Further, due to the fact that, in essence, a digital EEG recording is, in a mathematical sense, a time series, it has become possible to apply a large number of different mathematical analysis algorithms to the processing of this series. Firstly, this is an interpolation procedure, the use of which made it possible to obtain a more compact representation of the information contained in the EEG - these are the so-called topographic maps. Its essence is as follows - the program, using a moving cursor, measures potential amplitudes synchronously across all EEG channels at a certain point in time, enters the measured values into the “nodes” of the map corresponding to the points where the electrodes are applied, then, using interpolation algorithms, calculates the theoretical values of the potential amplitude for all others map points, then applies black-and-white or color coding to the resulting array of values, and we obtain topographic maps of the distribution of the amplitude of the electrical potential over the surface of the head - view from above, side, bottom, whatever.
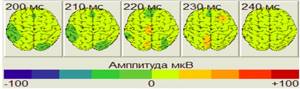
Topographic maps of EEG amplitude 200 ms and further after the cursor placed in the editing window.
The next improvement in computer analysis of EEG is associated with the use of the so-called. spectral analysis using fast Fourier transform - the EEG time series is fed to the input of this algorithm, and at the output we obtain the spectral density function for all frequencies of the EEG spectrum - usually from 1 to 100 Hz. Having summed up the spectral density values in standard EEG rhythm ranges (1-4 Hz - delta, 4-8 Hz - theta, 8-12 Hz - alpha, 12-36 Hz - beta, 38-42 Hz - gamma) or in any individual ones, we can imagine the severity of various EEG rhythms in the form of the same topographic map as in the case described above with potential amplitude.
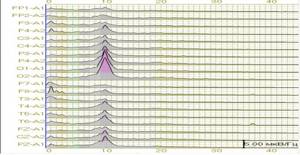
Power spectra for each of the 19 EEG leads from 0 to 50 Hz.
In addition to spectral analysis, we can apply a large number of other algorithms to the original EEG time series and obtain, for example, a topographic map of coherence or synchrony of potential oscillations in different areas of the cerebral cortex for different EEG rhythms - based on this indicator, it has become possible to talk about the functional connections of different brain structures and cortical areas. In general, the types of processing of the original time series are constantly being improved in both qualitative and quantitative aspects.
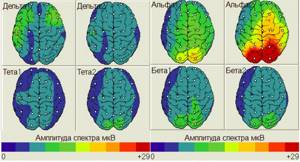
Topographic maps of the distribution of the spectrum amplitude indicator over the surface of the head for delta, theta, alpha and beta rhythms. The dots on the maps show the locations of EEG electrodes.
The next stage in the development of computer analysis of EEG is associated with the creation of computer EEG databases for both normal and various forms of mental pathology. The key names in this area are Bob Thatcher, who developed one of the few currently recognized regulatory frameworks, i.e. an EEG database for almost all ages, and Roy John, who developed the neurometrics method and a number of clinical EEG databases.
The essence of this stage is that in carefully selected healthy individuals in the age range from 3 months to 83 years without a history of mental and neurological diseases, whose relatives also do not have such a history of diseases, an EEG is recorded according to a standardized protocol (leads, rhythms, parameters, functional tests, etc.), individual EEGs are “run” through all processing algorithms, the resulting individual parameters are summed up, averaged and a huge array of various statistical metrics are obtained, which make it possible to statistically compare the EEG of an individual person with this base norm and obtain for this person topographic map of a statistical indicator of the reliability of deviations from the norm of any EEG rhythm and any of its parameters. We can say that this is one of the most recent achievements in computer analysis of EEG and reliable programs in this area have been developed relatively recently.
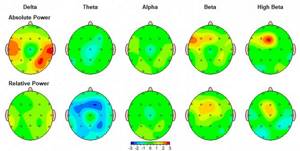
Topographic maps of Z-scores for absolute and relative power of delta, theta, alpha, beta, and high-frequency beta EEG of a patient with generalized anxiety disorder. The color shows the degree of statistical deviation from the norm (red – above the norm, blue – below the norm).
Currently, we are witnessing an even more complex stage in the development of computer analysis of EEG, associated with the development of expert systems using artificial intelligence algorithms to automate the process of describing and diagnosing clinical EEGs. However, this stage is still far from complete and requires joint actions of a large number of scientific and clinical teams. One of the tasks of this stage is to identify stable abnormal patterns of electrical activity of the brain in various mental diseases - endophenotypes or EEG phenotypes.
It is the provision on endophenotypes and biomarkers that forms the basis for the future objective classification of mental disorders, the foundations of which are being actively developed at the present time. To date, 14 different EEG patterns-phenotypes have been described in the literature, occurring in various mental illnesses and reflecting disorders of certain brain systems. It is endophenotypes, according to modern concepts, that are an indirect link between the genotype and a specific mental illness. However, we will postpone a more detailed consideration of this issue until a future publication on the website of our Center.
Author of the article: Ivashchenko Oleg Ivanovich
Ivashchenko Oleg Ivanovich, Neurophysiologist, biofeedback therapist, candidate of biological sciences
If you need help from an experienced specialist, make an appointment with Oleg Ivanovich.
Make an appointment