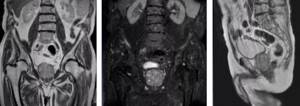
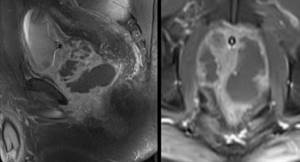
MRI: prostate cancer T2a and T3a (arrows indicate involvement of the capsule in the tumor process) MRI remains the leading method of medical imaging, allowing us to clarify the nature of diseases in the most complex cases. Magnetic resonance scanning is an absolutely safe study for people without metal in the body: for patients with installed implants (pacemaker, drug pump, hearing aid, etc.) the diagnostic procedure is contraindicated.
If brachytherapy, which involves implanting permanent radioactive seeds into the organ, was performed during treatment for prostate cancer, the images may be distorted. In such a situation, the tumor is monitored using ultrasonography (including TRUS - transrectal ultrasound) and computed tomography (CT).
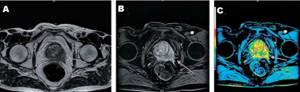
A - magnetic resonance imaging demonstrates uneven contour of the capsule of the left lobe of the prostate with the spread of the soft tissue component beyond its limits (arrow), T2 VI. B — image after dynamic administration of gadolinium. C - after processing by a computer program - a clear increase in the intensity of the MR signal in the pathology area, typical of neoplastic degeneration
The greatest diagnostic value is obtained from images obtained using multiparametric MRI, which combines dynamic contrast and diffusion-weighted studies.
Comprehensive magnetic resonance imaging is prescribed to patients with suspected malignant tumor process, which makes it possible to evaluate pathological foci in the prostate with minimal risk of error and avoid biopsy.
Do they do MRI of the prostate?
The prostate is a glandular-muscular organ of the male reproductive system, resembling a chestnut in shape, weighs 25 g. Vertical size is about 3 cm, horizontal - 4 cm, depending The normal parameters vary depending on age. The main function is the production of secretion to maintain the vital functions and normal motor activity of sperm. Features of the anatomy (girth of the initial part of the urethra, adherence to the bladder and rectum) determine the clinical manifestations of pathologies: discomfort in the perineum, dysuric disorders. With a significant enlargement of the prostate and impaired urodynamics, acute urinary retention, etc., develops as a complication.
Magnetic resonance imaging of the prostate gland is mainly prescribed by urological oncologists to obtain the most accurate picture of a space-occupying formation. Patient management tactics are based on:
- process stage;
- assessing potential tumor progression;
- timely diagnosis of relapse;
- identifying suspicious areas before planning a biopsy, etc.
Blood flow disorders, vascular malformations, and the size of the pathological focus less than 0.5 cm imply contrast. Intravenous administration of an amplifier with paramagnetic properties improves visualization.
Why are additional instruments used during tomography?
Some radiology practices use an endorectal (inside the rectum) coil as part of the scan. An endorectal coil is a latex (rubber) balloon with a central tube. It is lubricated and then inserted into the rectum and inflated to secure the position of the coil, which is then removed.
This helps provide high-quality images of the prostate and surrounding area by reducing the influence of intestinal motility. When using an endorectal coil, the cost of the examination increases. To make the procedure more comfortable, the patient may be given an injection of an anesthetic.
Prostate diseases
According to the images obtained using MRI, there are:
- malignant neoplasms (final verification occurs exclusively after a morphological study, which makes it possible to judge the degree of cell differentiation);
- benign prostatic hyperplasia;
- prostatitis (acute, chronic, granulomatous);
- complications of pathologies (abscess, fistula);
- fibrous transformation of tissues;
- cysts;
- prostatolithiasis (formation of stones, foci of calcification);
- prostate infarction;
- tuberculosis, etc.
In addition to examining the prostate gland, MRI is performed to diagnose an inflammatory, tumor process in the vesicles (seminal vesicles), stricture of the urethra, testicular tumor screenings, etc.
What does the procedure show?
Tomography of the prostate allows you to diagnose various pathologies of the gland and surrounding tissues:
- congenital anomalies;
- inflammatory processes;
- cysts;
- abscesses;
- prostatitis;
- complications after operations or injuries of the pelvic organs;
- hyperplasia;
- tumors.
During the study, layer-by-layer images are created, which display even minimal structural abnormalities and changes in the prostate, as well as the tissues surrounding this gland, nerve endings, blood vessels and bone structures.
If the development of an oncological process is suspected, tomography with a contrast agent may be required. A special marker drug accumulates in the tumor, making it possible to make its contours clearer in the images and determine its exact size and location. In many cases, tomography can avoid a biopsy. Tissue sampling is not required if the images do not reveal tumor formations.
MRI of the prostate: preparation for the study

Preparing for an MRI of the prostate is an important step that should not be neglected. In emergency situations, the study can be done at the time of application. But preparatory measures allow you to fully obtain information when performing a diagnostic procedure.
To ensure better visualization of the prostate, it is necessary to give up gas-forming and constipating foods and drinks for 2-3 days:
- herbs (parsley, dill, onion, garlic, celery, etc.);
- vegetables (sauerkraut, salted and raw cabbage, peas, chickpeas, beans, soybeans, potatoes, tomatoes);
- raw fruits (apples, melons, grapes, mangoes, apricots, peaches, etc.);
- fatty meat and poultry;
- berries, watermelon;
- pastries, black bread;
- confectionery products (cakes, cakes, sweets, etc.);
- milk and derivatives (cream, sour cream, curdled milk, fermented baked milk);
- seeds, nuts;
- dried fruits;
- mushrooms;
- beer, sparkling wines and other alcohol;
- sparkling water, lemonade, strong tea and coffee, freshly squeezed juices with pulp, jelly.
You can cook dishes in the oven, by boiling, or steaming. The diet includes:
- rice, buckwheat;
- chicken and turkey breasts, veal;
- “yesterday’s” dried bread;
- eggs (omelet or soft-boiled);
- fish;
- zucchini, carrots, onions after heat treatment, etc.
Preparing for an MRI of the prostate does not imply reducing your caloric intake. On the day before the test, it is better to eat light broths; steamed cutlets and other minced meat products cooked with a minimum amount of oil, vegetable casseroles, unsweetened compotes and herbal teas are acceptable.
Colon cleansing is necessary for patients suffering from chronic constipation, if dietary nutrition has not led to independent, complete bowel movements (after discussion with the treating doctor). You should consult your doctor about taking medications that relieve flatulence: antispasmodics, sorbents, and antiperistaltic agents have a number of contraindications.
You must come for the test on an empty stomach with a full bladder. The last meal is allowed 4-6 hours before the diagnostic procedure.
Clothing is preferable to a loose fit, without metal zippers, buttons or decorations. Do not forget to take with you your passport, an extract from your medical history, a doctor’s referral, and the results of previous diagnostics (MR and CT scans, TRUS).
During MRI of the prostate with contrast, 10% of patients experience autonomic reactions: dizziness, drooling, nausea. You can reduce the severity of the side effects of gadolinium administration by having a light snack before leaving the house.
Indications and contraindications for MRI of the prostate

Magnetic resonance scanning of the prostate gland is prescribed for repeated increases in the level of prostate-specific antigen in the blood, TRUS results suspicious for a mass formation, to clarify the cause of chronic pelvic pain, determine the severity of the inflammatory process, and exclude complications , as part of dynamic monitoring of the disease, to assess anatomical features, differentiate pathologies, etc.
Acute uncomplicated bacterial prostatitis, hyperplasia of glandular tissue with normal levels of prostate-specific antigen do not require MRI or CT, the diagnosis is established by symptoms, digital rectal examination, laboratory tests, and ultrasound.
Complaints, the causes of which will be reliably demonstrated by an MRI scan of the prostate:
- difficulty at the beginning of urination, sluggish stream, need to strain, nocturia (frequent release of urine in small portions at night), sexual dysfunction. With the malignant nature of the process at an advanced stage, weakness, weight loss, sweating, increased temperature in the evening, etc. are added;
- severe discomfort in the perineum, lower abdomen, sensation of a foreign body in the rectum during bowel movements, ribbon-like stools (with significant enlargement of the prostate), episodes of urinary retention;
- fever with chills, acute pain, blood, pus in urine, semen;
- urinary incontinence after surgery (prostatectomy or transurethral resection) to identify damage to the sphincter, nerve bundles, etc.
Contraindications for prostate MRI:
- implanted devices containing metal;
- history of low-dose brachytherapy with the introduction of radioactive grains into the gland tissue;
- acute conditions requiring resuscitation;
- patient weight over 120 kg (for closed-circuit tomographs);
- inability to lie on your back during the diagnostic procedure;
- claustrophobia (if sedation is unavailable);
- mental and neurological diseases accompanied by uncontrolled motor activity, etc.
MRI of the prostate is preferably performed before biopsy, which increases diagnostic accuracy. If it is necessary to undergo examination after invasive interventions, you need to wait 3 weeks, during which time the areas of hemorrhage will level out and the tissue will heal.
Advantages

It is possible to ensure high quality diagnostics with modern equipment. At the MART clinic, MRI of the prostate is performed on a high-field German expert-class tomograph Siemens Espree. Unlike older models, this device has unique technical characteristics and provides maximum comfort for patients.
The ultra-short length and wide diameter of the magnet allow patients suffering from claustrophobia to undergo MRI. The weight limit is 160 kg, and on older models patients weighing no more than 120 kg can be examined.
MRI of the prostate, how is it done?

The diagnostic procedure includes a number of stages:
- clarification of contraindications during a preliminary conversation;
- signing a voluntary consent to conduct an MRI of the prostate;
- depositing items containing metal (cell phone, payment cards, keys, coins, watches, etc.);
- placing the patient on the tomograph table, fixing the limbs with belts to prevent motor activity, placing magnetic amplifier coils over the pelvic area;
- immersing the patient in the tomograph tunnel, scanning the area of interest; injection of a contrast agent into a vein is carried out after a series of native images (if an enhanced study is planned);
- description of images and delivery of results.
The medical staff watches the scanning progress through glass from the next room, and uses a microphone and headphones to communicate. In case of an emergency, the patient has a panic button at hand. The diagnostic procedure without contrast lasts 15 minutes, with an amplifier - 30, preparation of the report takes about half an hour. Multiparametric MRI of the prostate takes longer to complete than conventional MRI.











