About the procedure
This method of instrumental diagnostics, such as biopsy, is rightfully spoken of as one of the most informative and, most importantly, valuable in terms of the accuracy of the diagnosis or its refutation.
Often, a biopsy is resorted to after other diagnostic studies - ultrasound, CT, etc.
As medical practice shows, a biopsy has the smallest error in making a diagnosis. The method is used in a number of cases.
The main ones:
- Confirmation/refutation of preliminary diagnosis;
- Differential diagnosis of tumors in the organ of interest to the doctor;
- Early detection of cancer;
- Evaluation of previously prescribed treatment and its possible adjustment.
We can say that a biopsy has no limitations, in the sense that using it, a doctor can examine any organ of the human body and take a biopsy sample for further laboratory study.
Can be divided into two stages:
- The procedure for taking a biopsy sample;
- Laboratory study of the removed biopsy specimen.
This procedure in oncology is a mandatory research method; without it, it is impossible to use traditional treatment methods, for example, chemotherapy.
Recommendations after biopsy
After the biopsy is completed, the doctor may insert a gauze pad containing an anesthetic gel into the rectum, which will release on its own during bowel movements. It is advisable that when traveling home there are accompanying persons who will take you by car. The next day after the procedure, you can return to your normal life and continue taking the medications prescribed earlier.
After receiving the report, it is important to contact the doctor to discuss the need for treatment depending on the results. If you experience an increase in body temperature over time or problems with spontaneous urination, you should immediately call your doctor.
The price of a prostate biopsy depends on the method chosen. Fusion is considered expensive, but it gives more accurate results without requiring repeated studies. Fusion biopsy is performed in just a few Moscow clinics by an experienced urologist using modern equipment.
Procedure accuracy
When talking about the accuracy of biopsy results, you need to keep in mind the following factors:
- Experience of the physician and researcher studying the biopsy;
- Amount of biopsy sample taken.
Sometimes, for a more accurate conclusion, material is taken from a number of areas of the organ.
As noted above, a biopsy is a diagnostic procedure that allows us to find out with the highest degree of certainty the essence of neoplasms and distinguish the nature of the tumors: where is benign, where is malignant.
Patients do not have to be afraid of the procedure: it is completely safe and can be of great benefit in the early diagnosis of cancer and other diseases.
Why is a prostate biopsy done?
The prostate gland is an important organ of the male reproductive system, which produces a secretion that ensures the viability of sperm. Prostate cancer is the third most common cancer among men.
In the early stages of cancer, there are no obvious symptoms of pathology. Patients turn to a urologist with complaints that resemble an adenoma or inflammation of the prostate gland. The doctor performs a digital rectal examination to look for pathological nodes, lumps or swelling of the organ. The patient is referred for PSA (prostate-specific antigen), TRUS or MRI.
The results of a prostate biopsy help diagnose other diseases of the male reproductive system: fibrosis, adenosis, PIN, acute prostatitis, granulomatous inflammation.
What can you see
With the help of a biopsy we can solve a very wide range of problems:
- Obtain complete information about the characteristics of the pathology;
- Determine the nature of the tumor;
- Confirmation or refutation of a diagnosis made earlier;
- Diagnostics for the purpose of differentiation;
- Determine the stage of pathology;
- Eliminate the source of pathology;
- Evaluation of treatment effectiveness, etc.
Prostate biopsy
Contraindications for biopsy
Performing a biopsy or other manipulations in the prostate gland is not always safe. If there is a risk of bleeding, severe inflammation or other pathologies, the urologist will refuse to conduct a diagnosis.
Contraindications for biopsy:
- Infections in the genitourinary system: inflammation of the urethra, pyelonephritis, acute prostatitis.
- A depressed state of the male body, which appeared due to an infectious process or others.
- Deviations in blood clotting parameters: a puncture with a biopsy gun leads to disruption of the integrity of blood vessels; if the blood does not clot well, complications will arise.
- High blood pressure that cannot be controlled with medication.
Diagnosis in case of contraindications is postponed until they are eliminated. The exception is that the threat to life due to cancer is higher than the risk of complications.
Goals
After the procedure, the collected biopsy is examined - cytology or immunohistochemistry.
The study of pyoptate is carried out using a microscope.
There are many, many indications for the procedure:
- Suspicion of cancer;
- Carrying out distinctive diagnostics;
- Performing cytology or immunohistochemistry of tissues and organ cells;
- Determining the nature of infertility;
- Determining the risk of pathogenization of moles;
- Determining the source of metastasis;
- Characterization of cancer;
- Removal of the tumor during surgery;
- Assessing the optimality of therapy already prescribed, etc.
The procedure can be repeated if the seized material turned out to be insufficient, as well as to detect concomitant diseases that require additional diagnostics. But in any case, a biopsy is the final diagnostic method.
Indications for prostate biopsy
The manipulation is carried out initially and repeatedly. A primary biopsy is prescribed by a urologist if there is a suspicion of cancer. Indications for the study:
- Elevated level of prostate specific antigen (PSA) in a blood test - from 4 ng/ml and above.
- A digital examination of the prostate reveals lumps, tumors or nodes.
- Ultrasound of the peripheral part identified heterogeneous, hypoechoic zones.
The urologist prescribes a repeat prostate biopsy in the following cases:
- The initial analysis showed a negative result, but the suspicion of cancer remained.
- The PSA level remains high or increases, the free antigen decreases in relation to the total.
- The primary survey material was insufficient.
During the primary and repeated procedures, biomaterial is taken from the peripheral and transitory zone of the prostate gland. This allows you to obtain the required number of biopsies (tissues) for examination.
Razor
This is taking material by scrapings, smears, fingerprints.
When a small amount of biopsy is needed for research, this type is used.
So, to diagnose a cervical tumor at the initial stage of the disease, an impression smear is made. A biopsy obtained in this way is quite sufficient for research.
Performing the procedure, the doctor removes a layer from the surface of the skin. The resulting bleeding surface is treated and covered with a bandage.
Cost of biopsy at various sites:
| Name of service: | Cost, rub. |
| Skin biopsy | 3200 |
| Percutaneous breast biopsy | 8000 |
| Gastric biopsy using endoscopy (without the cost of histological examination) | 3000 |
| Large intestine biopsy (without the cost of histological examination) | 2200 |
| Biopsy of nodules, tophi | 1500 |
| Lymph node biopsy | 8000 |
| Biopsy of the oral mucosa | 6000 |
| Tongue biopsy | 2800 |
| Biopsy of lip tissue | 3000 |
| Thyroid biopsy (without the cost of ultrasound support) | 3000 |
| Biopsy of the laryngopharynx mucosa | 6000 |
| Tissue biopsy of the pyriform recess | 6000 |
| Ovarian biopsy (without the cost of ultrasound support) | 20000 |
How important is a correct diagnosis?
The patient, a young woman, 32 years old, virgin, suffered from periodic breakthrough bleeding, resulting in anemia. They did a pipette biopsy; there was little material for research; they diagnosed uterine cancer and suggested removing the uterus. The patient decided to remove the hymen to make a correct diagnosis. They took tests and revealed hyperplasia due to lack of sexual activity. Treatment was carried out, after 2 years the patient got married and gave birth to a child.
A 50-year-old female patient complains of stomach pain. In November, the clinic performed a gastroscopy, an ulcer was in doubt, and a diagnosis of ulcerative gastritis was made. Appropriate treatment was started. Due to diet and stomach pain, the patient began to rapidly lose weight, losing 10 kg. I had a repeat gastroscopy in another clinic. The diagnosis of ulcer was confirmed. Treatment did not bring improvement. The patient contacted the Center for Integrated Medicine. A gastroscopy with an extended biopsy was performed and cancer was detected, but time was lost. At this stage of cancer, only palliative treatment was possible; chemotherapy sessions were performed, but the prognosis was unfavorable.
puncture
This method, by its name, refers us to Latin, where “punctio” means “injection”. There are 3 types of this procedure:
- Fine needle;
- Thick needle;
- Aspiration.
Fine needle
Used when it is necessary to obtain a small number of cells. The doctor inserts a needle into the suspicious area and removes a sufficient amount of biopsy material.
thick needle
Used to obtain large quantities of material. This type is considered optimal: it allows you to collect a lot of material for subsequent study without making a cut.
The doctor immerses a hollow cylinder, the edges of which are sharp, into the area of interest, and columns of tissue fill it.
This procedure is applicable for tumors of the liver, prostate, etc.
Aspiration
When carrying out this procedure, a vacuum aspirator is used, which is a cylinder where negative pressure is created. A needle is connected to the cylinder, with the help of which the desired material is obtained. You can pick up several pieces of fabric at once.
Most often, this procedure is applicable in gynecology.
Biopsy analysis results
Laboratory analysis is carried out within 10-14 days, after which the patient receives a report indicating the number of tissues taken, the nature of the samples and the presence of cancer.
A negative biopsy shows no signs of changes in suspicious cells in the area examined.
The result may indicate the presence of benign changes:
- Atrophy: focal or diffuse. Occurs in men who have undergone hormonal therapy.
- Inflammation: chronic or acute prostatitis.
- Adenosis: atypical adenomatous hyperplasia.
Histological examination readings can detect cells that fall between normal and cancer. Reasons for a suspicious biopsy:
- PIN (prostatic intraepithelial neoplasia).
- Atypical proliferation of acinar cells.
- Proliferative inflammatory atrophy.
Under Scan
When suspicious tumors cannot be detected by palpation due to their tiny size, radiography, ultrasound, and MRI come to the aid of the doctor. The procedure in these cases is controlled by an image, such as an x-ray, which helps the doctor control the tip of the needle.
The image is used in several planes. This helps to understand how the tumor is localized more clearly.
This procedure can be fine-needle, thick-needle, or aspiration.
Types of prostate biopsy
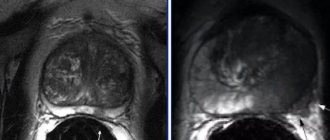
There are several methods of prostate biopsy - transrectal, saturation and fusion. Transrectal is considered the gold standard. But to accurately detect suspicious areas, an MRI of the pelvic organs with contrast is performed. Based on the results obtained, more modern and informative techniques are used. Only a few clinics in Moscow perform fusion biopsy of the prostate, which gives comprehensive results.
Transrectal prostate biopsy (TRUS) is the gold standard and a common test technique for elevated PSA levels. For diagnosis, a biopsy manipulator and thin needles with cutting edges are used. Biomaterial is collected from 12 points to obtain a complete description of the histological structure.
The procedure is performed through the rectum under local anesthesia under the control of an ultrasound scanner. This allows the urologist to accurately determine the location of the area of the prostate suspicious for tumor. After receiving the materials, the tissues are preserved in solution and sent to the laboratory for examination.
Saturation technique
Saturation prostate biopsy is an advanced research method. It is carried out to verify the diagnosis when, after a biopsy, histology shows no evidence of cancer, but PSA continues to grow. Material is collected from 24 points or more, depending on the volume of the prostate.
The method reduces the need for a repeat biopsy and does not lead to an increase in complications. Diagnostics is used for secondary research, but is also prescribed for primary testing if the patient’s age is less than 65 years, PSA is below 10 ng/ml.
Fusion
Fusion prostate biopsy is a diagnostic method that is performed using combined MRI-ultrasound control and provides a complete picture due to a three-dimensional image of the gland. The resulting images are superimposed on each other - this helps the urologist to examine the exact localization of the site where the material was taken. This is important because it becomes possible (if cancer is detected) to carry out a local treatment method: cryo and brachytherapy.
With fusion, 3-4 targeted punctures are performed in the suspicious area, taking into account MRI data. The technique is complemented by the saturation method to obtain a more accurate result.
If cancer is suspected, an MRI of the prostate with contrast is performed. If the diagnosis shows pronounced suspicious areas, a fusion technique is prescribed. The method is especially relevant when several transrectal studies have shown a negative result.
Suspicious areas are classified according to the Pirads scale:
- 2 points – low probability of cancer. If PSA levels are elevated or there are palpable masses, a repeat biopsy may be ordered.
- 3-4 points – signs of altered cells. To exclude a negative result, a saturation or fusion biopsy is performed.
- 5 points – high probability of prostate cancer.
Biopsy and endoscopy
A biopsy during endoscopy is called targeted; it is used, for example, in diagnosing the gastrointestinal tract.
For the procedure, an endoscope is used, through which forceps or a needle are passed through a tube to collect tissue, for example, from the stomach
If the sample is taken from the colon, the endoscope is inserted through the anus.
To obtain a biopsy from the stomach, an endoscope is inserted through the mouth.
A similar procedure can be performed to study other organs.
What is the basis for the research?
The features of the biopsy procedure itself depend on the location of the tissue and organ that needs to be examined.
In most cases, a biopsy can be performed using a needle, which is the most minimally invasive procedure and allows the patient to go home the same day. In this case, visual control allows you to select the best point for inserting the needle and bring the instrument to the site of pathological changes: fluoroscopy, ultrasound, CT or MRI.
If the focus of pathological changes is located in hard-to-reach places, then a surgical biopsy in the operating room may be required. In this case, the removal of a tissue sample requires the presence of a surgeon who performs a minor operation. To determine the location of the lesion and collect tissue, the doctor uses an instrument equipped with a small camera.
Image guidance allows the doctor to insert a needle through the skin and guide it to the suspicious area of tissue.
A sample of cells and tissues is collected using one of the following methods:
- A fine-needle aspiration biopsy uses a small-gauge needle and syringe to remove fluid or a small sample of cells.
- During a core needle biopsy, an automatic spring mechanism is activated, which “pushes” the needle deep into the tissue. After returning the needle, the hollow part of the instrument is filled with a tissue sample in the form of a column. The cutting element of the instrument immediately cuts off the tissue and holds it inside the syringe. The process is repeated several times.
- In a biopsy using a vacuum device, the needle is first placed into the area of pathological changes. After this, a vacuum device is activated, which “sucks” the tissue sample under pressure into the hollow part of the needle. The tissue is cut using a cutting element and passes through a needle into a special reservoir. The process is repeated several times.
Up
Accuracy and time
Taking into account the accuracy of the biopsy sample taken for research, we highlight:
- Classic methods. They are carried out if the exact location of the tumor is difficult to establish;
- Targeting methods. They are used during endoscopic examinations, as well as under ultrasound and x-ray control.
The procedure can also be urgent or planned:
- The procedure for taking a biopsy sample is performed during surgical interventions. Examination of the removed tissue takes up to half an hour. Further operational tactics depend on the results.
- A planned study is carried out by fixing the removed tissues in special solutions. Later, their samples are cut and stained. The study may last several weeks.
Histology: what kind of analysis is this?
The collection of biological material and its careful histological analysis are very important in many branches of medicine. In order to identify pathology, for example, histology of a mole, cervix, digestive tract, endocrine system, and so on can be prescribed. Our questions about histology were answered by Sergei Viktorovich Ezhov, an oncologist-mammologist at the Expert Clinic Voronezh.
- Sergey Viktorovich, tell us what kind of analysis this is - histology? What is its essence?
— Histological analysis is a highly accurate research method that allows you to determine pathological deviations in the structure of tissue. This method is used in many areas of medicine, but its main essence is that using this method it is possible to diagnose the presence of malignant tumors, determine their structure, as well as the stage of the pathological process.
— What can be a biomaterial for histological examination?
— The biomaterial can be one or another suspicious tissue (skin, mucous membrane, muscle, bone) taken through a biopsy, or a preparation obtained as a result of surgery.
— When is histology prescribed?
— As I already said, histological examination can be used in many areas of medicine, but its special value lies in determining the nature and nature of changes in tissue at the slightest suspicion of an oncological process. This study is also carried out before prescribing antitumor therapy to develop a treatment plan and during treatment to monitor its effectiveness.
— What does histology show?
— Histological analysis makes it possible to detect inflammatory processes in tissue, establish the nature of a particular neoplasm (i.e., whether it is benign or malignant), determine the level of malignancy, and also identify the localization of the primary tumor focus. You must understand that only a specialist should decipher the results of histological examination. I would not recommend that patients do this on their own.
Biopsy
— How to get tested for histology? Is special training needed?
— Before conducting a histological examination, it is necessary to perform a biopsy and send the resulting material (biopsy) for analysis. As such, the biopsy does not require any preparation; there are only a number of restrictions and recommendations that the patient must adhere to the day before and during the collection of the biopsy. It is important to inform your doctor about all medications you are taking. On the eve of the study, you must stop taking medications that affect blood clotting (in consultation with the doctor who prescribed them), and also inform the doctor who will perform the biopsy about the presence of allergies. It is undesirable to carry out this manipulation in women during menstruation. Alcohol consumption is contraindicated.
— How is histology performed?
— The material obtained from the biopsy is placed in formalin and sent for histological examination to the pathomorphological center. There the material is filled with paraffin (most often). After cooling and hardening, thin sections are made, onto which various reagents are applied for a detailed study of the tissue under a microscope by a pathologist.
— How long does it take to perform a histological analysis?
— If the result is obvious and beyond doubt, the conclusion is issued on average in 7-10 days. If doubts or suspicions arise about the accuracy of the diagnosis, the drug may be studied longer.
— Are there errors in histology results?
— Unfortunately, especially in small settlements, problems may arise with the quality of histological analysis. This is due to various reasons (lack of doctors, equipment, consumables). But if doubts arise about the correctness of the histological conclusion, a review of the finished preparations is usually prescribed in another pathomorphological center.
Want to learn more about other types of tests? Read articles in our section You can make an appointment with an oncologist here ATTENTION: the service is not available in all cities
Interviewed by Marina Volovik
The editors recommend:
Precancer: to be afraid or not to pay attention? Fear has big eyes. Is fibroids really that dangerous? Breast cancer is not a death sentence!
For reference:
Ezhov Sergey Viktorovich
In 2007 he graduated from the medical faculty of Kursk State Medical University.
2007 - 2009 - clinical residency in the specialty “Oncology” at the Medical Radiological Research Center of the Russian Academy of Medical Sciences in Obninsk (today - MRRC named after A.F. Tsyb - a branch of the Federal State Budgetary Institution "National Medical Research Center of Radiology" of the Ministry of Health of Russia).
Currently, he is a doctor-oncologist-mammologist at the Expert Clinic Voronezh.
Reception is conducted at the address: st. Pushkinskaya, 11.
Preparation
No special preparation is required for the procedure. A mandatory story from the doctor about its essence, risks, as well as the written consent of the patient is required.
In 2-3 weeks you need to forget about smoking and alcohol, adjust your diet, remove spicy, fatty, smoked foods. 12 hours before the procedure you should not take food, and 3 hours before the procedure you should not take liquid.
If necessary, anesthesia is used. If general anesthesia is used, the patient should not drink or eat for the period specified by the doctor.
The need to remain under medical supervision exists for 8-10 hours, after which the patient goes home and is required to take precautions:
- The first few days are semi-bed rest;
- No heavy physical activity;
- Healthy eating;
- Healthy lifestyle
How is a prostate biopsy performed?
When performing a prostate biopsy, several people are present: a urologist, a nurse and a radiologist in the case of fusion. Before the test, a urine test is performed to look for signs of infection. If there are inflammatory processes, the examination is postponed.
During a transrectal biopsy, the area around the rectum is treated with an antiseptic. Lidocaine is injected into the intestinal wall, after which an ultrasound probe (sensor) is placed into it to obtain an image of the gland.
Thin spring-loaded needles are inserted into the prostate to obtain biomaterial. After the procedure is completed, the ultrasonic probe (sensor) is removed and the samples are sent to the laboratory.
Fusion biopsy is performed under spinal anesthesia in the lithomic position (the lower part is immobilized). An ultrasound probe is inserted into the rectum. The resulting image is synchronized online with MRI data to accurately match contours on a special biopsy grid.
Complications
It all depends on the type of research. For example, the risks of a procedure during a surgical procedure are due to the procedure itself.
During the puncture procedure the following are possible:
- Damage to a vessel with a needle;
- Bleeding;
- Infection;
- Painful sensations for some time.
At the Integrative Oncology Clinic Onco.Rehab you can get the addresses of clinics - our reliable partners, where various types of biopsies are performed. The qualifications and experience of our friends, the use of high-tech modern equipment will make the risks of conducting research unlikely.
Features of the postoperative period for men
In most cases, patients tolerate the procedure well. After a transrectal biopsy, the person goes home independently (just not while driving).
Since saturation and fusion biopsies are performed under general anesthesia (spinal anesthesia), the patient remains in the clinic for a day for observation. The man is fitted with a urinary catheter, which is removed after a day - this is necessary to prevent disturbances in the outflow of urine and its normal excretion. After recovery, he is discharged.