Fluorography (one projection) is a screening (mass) method for diagnosing primary pathologies of the chest organs, and is a type of x-ray examination.
X-rays can adversely affect human health, provoking pathological processes at the cellular level. Large doses can even lead to the development of cancer. Today, doctors use digital fluorography - a safe type of examination . To determine radiation exposure, use the Dosimeter.
Film fluorography: features and differences from x-rays
Film apparatus (There is a cassette on the left side of the CCD matrix)
Film fluorographic examination is not a safe procedure. Like X-rays, it uses rays passing through the human body. They provide a film image of the heart and lungs, from which the doctor makes a diagnosis.
With film fluorography, the image is small in size, and is shown by whole reels of film used per shift. That is why the results of fluorography must wait 1-1.5 days. Since the film size is small, the image quality is unsatisfactory - signs of tuberculosis, pneumonia or oncology can be seen in the image, but a more detailed picture can be seen on an x-ray of the lungs (two projections).
Radiography (lung x-ray) is rarely used. If fluorography is done annually, then radiography is performed only if the signs of pathology described above are confirmed in the primary image.
An X-ray image is a kind of clarifying image, specifying the patient’s condition. How often you can do this will be determined by your doctor based on the permitted annual radiation load. The data can be viewed on large format film, i.e. life-size. Therefore, the doctor prescribes an x-ray only for pre-existing reasons.
It’s quite difficult to find a film machine these days, but such clinics exist!
The specialist explained why the world abandoned fluorography
— Sergey Anatolyevich, how do you assess the need to undergo fluorography?
— It all depends on how we apply this or that method, in the required volumes and places. If we answer these questions “yes, this is so,” then it is undoubtedly useful. Fluorography at a certain period of time was an absolutely irreplaceable, necessary research method that saved many lives. But the epidemic situation is changing, other methods have appeared, and currently fluorography is not a method recommended by international organizations, with the exception of the Russian Federation and the countries of the former CIS. Leading powers do not use this technique.

- Why? Expensive?
— Any screening method is expensive, even if its effectiveness is confirmed, and the issue of confirming the effectiveness of fluorography is very controversial. If we talk about the economy, then in the Russian Federation in 2010, 67 million fluorographs were performed, in 2014 74 million, in 2021 about 81.5 million procedures. At the same time, the proportion of identified patients with tuberculosis from the number of fluorographs was only 0.052%. And this figure is decreasing all the time. In 2021, it was 0.036%, or 29,653 patients. That is, for one identified case, 2,745 fluorographic examinations need to be carried out. The question is that when a doctor conducts almost 3 thousand fluorograms and everything is normal, he stops looking at the fluorograms so carefully, especially when he needs to describe 100–150 studies every day. This is a difficult psychological task.
Each study in Moscow costs from 22 to 84 rubles, depending on the tariff. Quite a lot of money is spent in Russia, in my estimation, around 3 billion rubles, or, in other words, to identify one case - about 100 thousand rubles. This amount does not take into account capital investments associated with the purchase of equipment. There are about 6 thousand fluorographers working in the Russian Federation; They need to be changed every 10 years, or even more often. This also requires funding. You can argue with the numbers, but these are official data. Therefore, the conclusion is: in those places where there is a lot of tuberculosis, fluorography needs to be carried out, and in order to carry it out to everyone, you need to understand how effective it will be, how necessary it is. Although, undoubtedly, identifying such a socially significant disease as tuberculosis is an important element of ensuring public health, and this must be done, but done wisely.
— By necessary places, do you mean the FSIN system?
— Yes, the technique is necessary in the penal system, as well as in controlling migration flows, in decreed groups of the population (doctors, teachers, catering workers, etc.) and in regions with an unfavorable epidemiological situation. In these cases, the use of fluorography is logical, but for everyone it is an excessive measure. It seems that it will not be possible to abandon the current system immediately, but fluorography can gradually be replaced by other, more informative methods. And if, for example, we are not talking about tuberculosis, but about detecting lung cancer, then with a computed tomograph with a slightly higher radiation dose than with fluorography, we get an image whose diagnostic value is significantly higher. This study also should not be performed by everyone. Low-dose computed tomography is performed in a risk group - these are people who smoke (20 cigarettes per day or more) from 50 to 75 years old. The criteria for any screening method must be very clearly defined.
— When fluorography is performed, is the early stage of tuberculosis or lung cancer visible in the image?
- As a rule, cancer is visible quite late, when it is already very difficult to treat, this is what does not allow the use of fluorography to assess lung cancer. It is much easier to suspect tuberculosis, but also not always, since they usually take one photo. In some cases, it is more effective to replace fluorography with a survey image of the lungs.
We have a problem when a patient prescribes a test for himself. He comes to the doctor and says: “Let’s do me a tomography/X-ray/MRI/PET scan.” Of course, the doctor refuses, since the insurance company will not pay for such a study in the clinic, but if the patient comes to do it for a fee, then, unfortunately, he is not refused. At the same time, the persistent desire of some patients to “get examined” can be so obsessive that sometimes it is easier for the doctor to agree with this desire than to explain that the examination is not necessary. In my practice, there was a case when a patient was undergoing a computed tomography scan in different institutions, something seemed to be there, and she decided that she needed to do a CT scan at a certain frequency. By the time she accidentally contacted us, her total accumulated dose was approaching 200 mSv, and the research itself was absolutely useless.

In Russia, 45% of X-ray equipment has a service life of more than 10 years. Photo: ru.net
— What is the maximum load?
— In medicine there is no maximum load, everything is determined by benefit or harm. If the harm of carrying out the procedure exceeds the harm of “not performing it,” then it is not carried out. For example, if a patient is in critical condition and it is necessary to determine the tactics of further action, none of the doctors will even think about the fact that the patient had previously undergone any tests, even if he has radiation sickness. If research is needed to save a life here and now, nothing else matters. If we calculate the doses for all studies and divide their sum by all residents of the Russian Federation, then on average each of us receives a dose of 0.5–0.6 mSv per year from medical exposure. In the USA, for example, medicine accounts for more than 3 mSv; in Germany, medical exposure is about 2.5 mSv. Radiation doses from medicine in these countries exceed the natural background radiation, and this forces the authorities to seriously think about controlling this type of radiation.
— Is there data on the number of unnecessary prescriptions and the reasons?
— Yes, about 30% of research is the average in the world. In Russia there are mandatory procedures for the provision of medical care. And if the doctor doesn’t prescribe something, then insurance organizations can punish him, and the patient himself can say that the doctor didn’t do something to me, and has the right to complain. And, as our American colleagues say, 30% of research is done not for the patient, but for the lawyer. But I think that we also have our own peculiarity: in Russia, a large number of useless studies are also associated with the “spirit of collectivism,” so to speak: the clinician orders a study “just in case” in order to share his responsibility for the patient with the radiologist .
— How many studies are carried out with errors?
— If we are talking about all x-ray studies, then, according to international studies, about 10–15% of studies have incorrect, or missed, or delayed diagnoses, that is, insignificant errors. An interesting situation: up to 30% of initial descriptions of X-ray images do not coincide with repeated diagnoses. Several years ago, a large American hospital conducted a study in which doctors were given a description of a study they had previously described, and the number of discrepancies was almost 25%. An acceptable level of discrepancy is considered to be 4–5%. In this case, there should be no clinically significant discrepancies that affect the tactics of further treatment of the patient. In the USA, a fairly large part of the claims are against radiologists. But most of the claims are purely emotional claims, and no more than 5% of decisions are in favor of the defendants.
— What complications can you get from low-quality equipment?
— If we talk about complex studies that can create a large radiation dose in one area of study (angiography, multiphase computed tomography), then if the equipment breaks down and the personnel act incorrectly, the radiation dose can be very large. But this happens extremely rarely; over the entire period of observation (since 1895), about 300 such cases have been described worldwide. Medical overexposure, as a rule, occurs in countries with well-developed radiation diagnostics, where the number of studies is huge, but with fluorography this, in principle, cannot happen. This does not happen in low-dose computed tomography either.
- And if you fly somewhere, passing a metal detector...
— Inspection installations for passengers at airports, as a rule, operate without sources of ionizing radiation; there are, however, also with X-ray tubes, but the dose there is very small. To get something meaningful, you have to walk all day. To inspect luggage and goods at airports or the metro, on the contrary, they mainly use X-ray machines, but they are absolutely safe for people, as well as for your things. I find it very funny to hear stories from my Customs colleagues about how some passengers throw away food after it has passed through the X-ray machine conveyor. These fears are in vain: nothing will happen to your food and other things, they will not become radioactive or harmful - this is due to physical laws. The frames of metal detectors have nothing to do with radiation exposure at all; this is electromagnetic radiation of a completely different spectrum. Regarding airplane travel, all you need to know is that the dose for pilots is limited to 5 mSv per year. It's unlikely that you fly more than pilots.
— Recently in Taiwan, scientists after studying 22 thousand case histories concluded that computed tomography, in which the patient receives radiation, increases the risk of developing thyroid cancer and leukemia, especially women and people under 45 years of age. Other scientists say that reducing the load dose during CT scans reduces the effectiveness of the study. Can you comment on such contradictions?
— My opinion is that the truth lies somewhere in the middle, everything is good in moderation. There are risks, but they should not be exaggerated or demonized. The Russian Federation, as well as the IAEA, has adopted the most conservative and safe for citizens no-threshold model. If someone objects, then “just” it is necessary to prove the inconsistency of this theory, while none of the scientists has been able to do this, and the position “prove that it is harmful” is not suitable here.
— How to choose a place, on what equipment to carry out fluorography, what is the situation with equipment in Moscow?
— In Moscow, in my opinion, there are no film fluorographs left, but in Russia there are 700 film fluorographs and 5108 digital ones. Digital fluorographs are an order of magnitude safer than film fluorographs.
— What part of the equipment requires replacement?
— In radiology, the service life of equipment is usually about 10 years. The actual need to replace a particular device, of course, depends on its operating conditions. The higher the load, the higher the wear and tear and the more often the equipment needs to be replaced. According to reported data, currently in Russia approximately 45% of X-ray equipment has a service life of more than 10 years. For CT and MRI machines this figure is slightly lower.
HELP "MK"
Fluorography is a study that involves photographing a visible image on a fluorescent screen, which is formed as a result of the passage of X-rays through the body (of a person) and their uneven absorption by organs and tissues of the body.
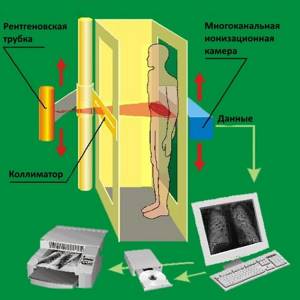
What are the differences between digital fluorography?
Digital fluorography is a progressive technique for diagnosing the chest organs. The main feature of such research is the transfer of images into digital format. At the same time, the quality of the image does not deteriorate and becomes better, and the radiation dose to the patient is less.
The image during digital fluorography becomes comfortable primarily for the doctor. If a film image could be unclear, for example, due to development errors, and the doctor needed to carefully peer into the picture and look for pathology, then there are no such problems with a digital image.
Digital scanning fluorograph (the safest and most modern diagnostic method)
The image is of the highest quality; using the program you can enlarge individual areas, add or decrease brightness, and adjust contrast. This provides new opportunities for research.
The procedure time is minimal, it takes about one minute. The rest of the time is spent on paperwork and dressing the patient. The image is ready 5-10 minutes after the examination, and after another couple of minutes it is saved on any storage medium - disk, external memory.
The undeniable privilege of digital images is that the data is stored in DICOM or HL7 format. If necessary, an image of the lungs is printed on a DICOM printer or sent by e-mail.
The fluorography room sees up to one and a half hundred patients per day. These features make digital fluorography in demand.

X-ray and fluorography of the lungs are a reliable way to diagnose organ pathologies. Based on the results of the study, it is possible to make a timely diagnosis and begin treatment of the patient.
Fluorography or “digital”? Analyzing diagnostic methods
Fluorography or “digital”? Analyzing diagnostic methods
The result of a medical examination or diagnosis of the lungs should be the most accurate diagnosis with minimal harm from the procedure itself. To choose the most appropriate research methods, it is worth understanding their pros and cons.
What equipment is used to study the lungs?
Today, in radiological diagnostics of the lungs, digital technologies have proven an undeniable advantage, and X-ray diagnostic studies using film are becoming a thing of the past. Digital fluorograph, digital X-ray diagnostic machine and computed tomograph are the most modern and safe examination tools.
Pros and cons of digital lung examination methods
The quality of the image directly affects the results of the study. Due to low image resolution, a radiologist may miss pathological changes in organs and tissues or mistake interference for signs of a disease. The key role here is played not only by the type of equipment, but also by the specific model of the device, its complete set and characteristics (type of digital receiver, etc.). In most cases, the image quality of digital fluorographs is inferior to digital X-ray diagnostic devices and is significantly inferior to the diagnostic capabilities of computed tomographs.
According to the World Health Organization, among the main non-communicable diseases leading to death in people under 70 years of age, cancer and lung dysfunction occupy second and third place. The mortality rate from lung cancer is greater than from breast, prostate and colorectal cancer combined. In 2015 alone, 2,907 cases of lung cancer were discovered in Moscow, the majority of them were smoking people of working age. In 75%, stages III and IV of the disease are stated. Detection of the disease at these stages significantly reduces the chances of saving the patient’s life. Low-dose computed tomography (LDCT) allows for timely and successful detection of lung cancer in the early ( I and II ) stages (studies show a 20% reduction in mortality), which is impossible with fluorography.
How harmful is radiation exposure during lung diagnostics?
Radiation exposure to a patient is usually assessed by the effective dose - it shows the risk of consequences for human health. The average effective dose when performing radiography on a digital device in organizations of the Moscow Department of Health is from 0.05 to 0.30 mSv. When conducting fluorographic studies, the average effective dose is determined in the range from 0.01 to 0.10 mSv. Effective doses in both cases satisfy the requirements of paragraph 2.2.1 of SanPiN 2.6.1.1192-03 “Hygienic requirements for the design and operation of X-ray rooms, devices and X-ray examinations,” according to which for healthy people the annual effective dose should not exceed 1 mSv. When performing LDCT, the load also does not exceed this standard. This means that the correct use of all three methods (fluorography, digital radiography, LDCT) for diagnosing the lungs is quite safe, and the benefits of using more accurate methods - digital radiography and LDCT - often significantly outweigh the possible health risks.
Is it possible to undergo a digital chest x-ray instead of fluorography when undergoing a preventive medical examination?
According to Order of the Ministry of Health of the Russian Federation dated March 21, 2017 N 124n “On approval of the procedure and timing of preventive medical examinations of citizens in order to detect tuberculosis,” fluorography of the lungs or radiography of the chest organs (lungs) is performed to diagnose an adult. You may have a digital chest x-ray instead of a fluorogram during your physical exam.
Eventually…
In other words, when diagnosing lung diseases, the most accurate method is computed tomography, and when conducting preventive medical examinations, X-ray studies using digital radiography instead of a fluorograph. This will allow the radiologist to analyze high-quality images and make more accurate diagnoses, and the patient will receive minimal radiation exposure. Be healthy!
What will an x-ray show?
An X-ray of the lungs helps visualize the organs located in the chest. In the image you can visualize both soft structures and dense ones, but the rays will give different shades. Diagnostics makes it possible to look at the heart, bronchi, lungs, lymph nodes and trachea. The description of these organs is enough to suspect abnormalities in one of them.

Tuberculosis
As for lung pathologies diagnosed by x-ray, these include:
- sarcoidosis;
- pneumonia;
- pleurisy;
- emphysema;
- oncology;
- swelling of the lungs;
- asthma;
- pulmonary tuberculosis.
X-ray copes with many diagnostic tasks successfully. Therefore, when sending for an x-ray, you should not worry about radiation exposure - it is much more important to see damage to organs.
Digital diagnostics of pulmonary diseases
Digital diagnostics has great capabilities, and therefore the image is more informative. For example, with a digital X-ray you can even find out who the picture belongs to - a man or a woman, since the results show shadows of the mammary glands in the form of contours.
Doctors receive information about the correctness of the study - how deep the breath was and whether the patient was motionless at the time of filming.

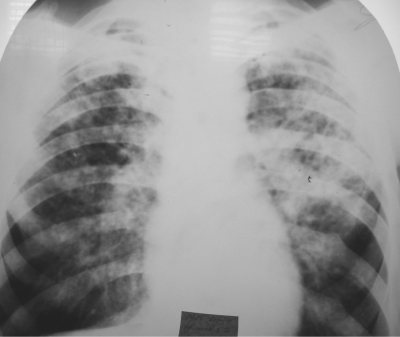
Photo of healthy lungs
When assessing the results of digital fluorography, doctors consider the following positions using x-ray irradiation:
- soft tissues;
- integrity of bone elements;
- location of the trachea;
- the presence of calcifications;
- contours of the heart;
- pulmonary fields.
The study is carried out in an anteroposterior projection. The images are informative and make it possible to assess or identify the presence of pathology in the lungs.
X-ray and fluorography for pneumonia - application features
Pneumonia, or pneumonia, is a dangerous disease with vivid symptoms. It needs to be diagnosed as early as possible, since the pathology has a high mortality rate with late diagnosis. In this case, doctors are faced with a choice - which is better, fluorography or x-ray for diagnosing the disease.
Pneumonia can also be detected by fluorography. The x-ray will show lesions larger than five millimeters in diameter, which can be seen on healthy lungs. At the same time, such spots are not detected during fluorography.
It is impossible to judge the presence of pneumonia by the spots - the fluorography data were obtained at low resolution, and therefore are an assumption. X-ray gives a clear picture and the results will be decisive in making a diagnosis. This is a basic test for suspected pneumonia. With its help it is good to control pathology.
What is fluorography and why is it called that?
There are two possible hypotheses here.
First: the author of the discovery, Wilhelm Conrad Roentgen, was a modest man who believed that these rays should not be named after him. And today in some languages of the world - in particular English - they are called “X-rays,” as the scientist asked.
And the second hypothesis is that the inventors of fluorography are good psychologists who understood that you are less afraid of X-rays, even knowing that they are there, if they are not mentioned in the name.
Perhaps both factors also contributed to the choice of such a medical term, but the main reason is different.
Have you noticed how big X-rays usually are? They are huge, life-size and even larger, since the rays from a point source after the object diverge even more. And all because X-ray focusing optics, which would make it possible to reduce the image, although it exists, is too complex and expensive to use in serial equipment. And without such optics, X-ray images are technically obtained not as photographs, but as so-called photograms - shadow images recorded on photographic material.
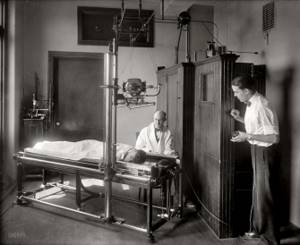
X-ray machine. 20th century Photo: forumimage.ru
But if radiography of most organs is done only when necessary, then the lungs are periodically scanned for almost everyone in order to detect tuberculosis in time. If you take these pictures full-size, you will need a lot of film. But a way out was found. Even two.
- The first is the use of electroradiographic devices (ERGA). Instead of photographic material, they use a layer that is pre-charged and then loses its electrostatic charge when exposed to radiation. Just like in a photocopier or laser printer. ERGA also prints on inexpensive plain paper.
- The old cartoon “Leopold the Cat’s Clinic” will tell you what the second way out is. It shows fluoroscopy - a method of x-ray diagnostics in which the image is obtained not on film, but in real time on a screen with a phosphor.
Of course, the filmmakers were joking, just like with the huge syringes in “Prisoner of the Caucasus.” Who doesn't love medical jokes? Fluoroscopy is not used during medical examinations, because the tube would have to be kept on the entire time while the specialist looks at all the details of the image on the screen. This would expose the patient, and the doctor, to a significant dose of radiation. Therefore, the scope of fluoroscopy is quite specific - emergency situations, when it is necessary to find out what happened after an injury immediately, and timely assistance justifies the danger of radiation.
When trying to understand the meaning of the word “fluoroscopy,” English speakers will remember the words flu, fluoride and flux - respectively, flu, fluorine and gumboil. But they have nothing to do with it, unlike the word fluorescence - fluorescence. This is a special case of luminescence, in which there is no afterglow. And if it is present, then such a special case of luminescence is called phosphorescence.
Now let’s see what happens during fluoroscopy in the eyes of a specialist looking at the screen.
The X-ray image, previously converted into a visible image by a phosphor, is reduced by the lens to such a size that it fits on the retina. After all, ordinary light rays, unlike X-rays, are very easy to focus. This means that after the screen with the phosphor, you can put a camera that reduces the image in the same way as the eye, and the problem is solved: the picture will be reduced. At the same time, the duration of switching on the tube can be minimized, making the procedure completely safe.
So you and I have reinvented fluorography - the successor of fluoroscopy, where the doctor’s eye is replaced by a camera.

Digital fluorograph Photo: Andshel, ru.wikipedia.org
Fluorography already allows you to save a lot of film, but what prevented you from making it even more economical? First the absence, and then the unprofitability of digital photography in the past. Well, as soon as this became profitable, digital cameras replaced film cameras and fluorographic technology, thereby reducing the need for photographic film to zero.
Another shooting method was also invented, in which the image is divided into lines vertically by moving a tube, the radiation of which passes through a narrow horizontal slit, and the lines themselves are divided into pixels horizontally by a multi-cathode ionization chamber. Everything together works similarly to a flatbed scanner. And although this method does not use fluorescence, it is also called fluorography by inertia.
The health hazard of modern fluorography methods, if performed no more than once a year, is so small that it can be neglected, which cannot be said about the danger that it allows to identify and prevent in time.
Tags: fluorography, medical terms
X-ray signs of pneumonia
It is possible to detect pneumonia on an x-ray. It will look like a single darkening against the background of healthy lungs. However, differential diagnosis may also be required, since the same darkening is detected in the presence of metastases, tuberculoma, and cystic formations.
Therefore, with pneumonia, the difference is implicit and diagnosing a single focus of darkening does not indicate the disease. This can be either inflammation or a sign of tuberculosis or oncology. For a final diagnosis, it is recommended to do additional studies.
Doctors should not miss the possibility of the appearance of a cancerous tumor, so in parallel with the research they add diagnostics for tumor markers.
Is it possible to detect pneumonia?
It is quite simple to identify pneumonia in an image of the lungs. Doctors take into account the number of spots that appear, compactions in the lung segments, and the intensity of light and dark areas. The radiologist will definitely pay attention to the root of the lung and changes in it. They also indicate pneumonia.

If you have pneumonia, the following signs will be visible on the image:
- focal lesions;
- unclear outline of the infiltrate;
- strengthening of the pulmonary pattern;
- expansion or thickening of the root of the lung.
The spots are localized in the lower sections, the pattern around them is deformed, and shadows of the bronchi will be visualized nearby.
Home › Diagnostic methods › Instrumental diagnostics › What fluorography shows and why it is important to undergo it
Tuberculosis
Tuberculosis is a socially significant disease that requires early diagnosis and controlled treatment.
It is known that more than 70% of all cases of this specific infectious pathology are detected through preventive examination. What does fluorography diagnose for tuberculosis? Typical radiological syndromes are presented in the table below.
Table: X-ray symptoms of tuberculosis:
| Type of disease | X-ray picture (with photo) | Description |
| Focal tuberculosis | Focal darkening against the background of an enhanced pulmonary pattern | Accompanied by the appearance of small localized foci mainly in the upper segments of the lungs. They usually have a rounded, clear shape; later, foci of fibrosis may form. |
| Infiltrative tuberculosis | Zone of infiltrative darkening in the right lung | Associated with the appearance of widespread foci of infiltration (fuzzy whitish darkening) with uneven edges. Sometimes the pathological process can involve several segments or an entire lobe of the lung. |
| Disseminated tuberculosis | Presence of multiple foci of Mycobacterium tuberculosis screening | It is characterized by the presence of many small (1-2 mm) foci of darkening with clear contours, located throughout the pulmonary field. They tend to merge and form vast conglomerates. |
| Cavernous tuberculosis |
| Accompanied by the presence of a cavern - a center of darkening with clear contours and a decay cavity (clearance) in the central part. |
| Fibrous-cavernous tuberculosis | An old cavity, the walls of which are replaced by connective tissue | On a fluorogram it appears as old cavities with areas of fibrosis. |
| Caseous pneumonia |
| One of the most severe forms of tuberculosis. It manifests itself as intense darkening of most of the lung (one or several lobes). The X-ray picture is inhomogeneous, small areas with varying intensities are observed. |
Lungs' cancer
The third disease that can be successfully diagnosed with fluorographic examination is lung cancer.
This pathology is accompanied by the following radiological syndromes:
- Peripheral darkening with fuzzy bumpy contours - can be with squamous cell carcinoma, adenocarcinoma.
- A notch along the darkening contour indicates possible drainage into the bronchus.
- A characteristic “path” to the root of the lung is a manifestation of lymphangitis.
- Lightening against a background of intense darkening is a sign of tissue breakdown.
- Rising sun syndrome (the appearance of an additional high-intensity shadow in the projection of the root of the lungs) is a probable sign of central cancer.
Diagnostic procedure allows you to detect lung cancer at an early stage
Above, we tried to figure out what diseases fluorography shows. This simple and accessible diagnostic method should not be ignored: it allows you to identify such terrible diseases as cancer and tuberculosis at a very early stage, when properly selected treatment will be most effective. Spending a few minutes once a year cannot be compared to many years of healthy life.
Where are diagnostics done?
Fluorography and x-rays of the lungs are carried out in any medical institution. The test can also be done in a private diagnostic center, where the patient receives the result in hand and gives it to the doctor who sent it for an x-ray.
Digital fluorography for lung pathologies is a necessary study that identifies such dangerous diseases as tuberculosis, pneumonia and malignant neoplasms. X-rays are used not only for diagnostics. For example, they can treat retinoblastoma, a malignant pathology of the organs of vision. When conducting a digital examination, the radiation dose is minimal, which means that the diagnosis will not harm the patient’s health.