MRI procedure If cancer is suspected, doctors often prescribe magnetic resonance imaging. This method is highly accurate and eliminates the risk of damage, discomfort and negative effects on organs.
One of the most common cancers in men in adulthood is prostate cancer. The following symptoms are considered a reason to contact a medical institution for help:
- problems with urination (blood impurities, pain, burning, feeling of incomplete emptying, incontinence, etc.);
- frequent urge to go to the toilet at night;
- erectile dysfunction, change in the appearance of ejaculate, etc.
First of all, the specialist will conduct a digital rectal examination and prescribe a blood test for PSA (prostate specific antigen). An increased level of this biochemical marker indicates a possible cancer or benign neoplasm (adenoma), inflammatory process (prostatitis) in the prostate gland. Early diagnosis plays an important role in effective treatment. MRI for prostate cancer helps differentiate pathology from other disorders. The procedure can confirm or refute the preliminary diagnosis made by the doctor.
Can MRI detect prostate cancer?
During magnetic resonance imaging, layer-by-layer images of the pelvic organ are taken. The result is an image of the area of interest in different planes. MRI for prostate cancer helps in a timely manner:
- determine the presence of tumors and metastases;
- assess the severity of the lesion;
- trace the involvement of the urethra, seminal vesicles, bladder, lymph nodes, rectal wall and surrounding tissues in the pathological process.
The procedure is performed with a contrast agent, which improves the accuracy of visualization of the organ. Thanks to the use of the indicator, cancer is differentiated from other pathologies of the pelvic organs of men. If the tumor is located in the anterior part of the peripheral zone of the gland, then it can only be examined with magnetic resonance imaging.
Stages of BPH
BPH 1 – compensation stage – prostate gland 30 cm3 or more in volume, bladder symptoms are absent or minimally expressed. Due to slight compression of the urethra, the detrusor muscle in the wall of the bladder is hypertrophied, but completely copes with its emptying.
BPH 2 - stage of subcompensation - the prostate enlarges, compression of the urethra increases, the muscular wall of the bladder ceases to cope with the complete expulsion of urine, its hypertrophy is replaced by hypotrophy and thinning. Incomplete urination - >80 ml of residual urine remains in the bladder. Difficulty in drainage of urine causes stagnation and expansion of the higher sections - the ureters, calyces and renal pelvis. Kidney failure gradually develops.
BPH 3 – stage of decompensation – inability to empty a full bladder, since its stretched detrusor muscle is no longer capable of contracting. At the same time, urine leakage occurs. It is spontaneously squeezed out drop by drop from the bladder into the urethra due to constant intake from the kidneys. There is a real threat of acute urinary retention - the inability to empty the bladder due to an irresistible desire to urinate. This situation requires emergency surgery.
What does an MRI show for prostate cancer?
High-quality MRI images are important for diagnosing prostate cancer. Based on the examination results, a decision is made on treatment tactics, the advisability of surgical intervention, and the direction of conservative therapy. Thanks to the accuracy of imaging, it is possible to reliably determine the location of neoplasia and the spread of the tumor relative to the prostate capsule. The doctor makes the final diagnosis based on the histological report obtained after a tissue biopsy. All other instrumental diagnostic methods are probabilistic in nature.
During the examination, the following pathological conditions of the prostate are observed:
- symmetrical growth of the organ, in which the contours of the gland are evenly expanded (signs of benign hyperplasia);
- enlarged prostate with unclear boundaries (prostatitis);
- single or multiple neoplasms with point localization (tumor process).
The normal state of the male genitourinary system is characterized by a smooth capsule of the prostate gland and testes, and the absence of obvious signs of proliferation of surrounding tissues.
MRI of the prostate gland (prostate): how it is done, what is visible in the images
WHAT IS A PROSTATE MRI
The prostate gland, or prostate, is a male organ located under the bladder and surrounding the urethra (urethra).
MRI of the prostate is a diagnostic method performed using a magnetic resonance imaging scanner and allows you to obtain detailed images of the prostate gland. MRI is used primarily to evaluate changes in the prostate cancer and determine the extent of the tumor, as well as to diagnose infections, benign prostatic hyperplasia, cysts and congenital anomalies. The study can be performed with an endorectal coil placed in the rectum, as well as with contrast enhancement, when a special drug is injected into the patient's vein. There is no radiation exposure during prostate MRI. Tell your doctor about any health problems, previous interventions, or allergies. The magnetic field is harmless, but may interfere with the functioning of the implants; Medical personnel must be alerted to the presence of any implanted metal bodies.
Get an MRI of the prostate gland (prostate) in St. Petersburg
WHY DO A PROSTATE MRI?
What are the indications for MRI of the prostate gland?
- Prostate cancer. In most cases, MRI allows not only to see a cancerous tumor, but also to assess its size, extent, and involvement of neighboring organs. Currently, radiologists use the description of prostate MRI according to PI-RADS - this is a standardized system for analyzing images and generating a medical report. It must be borne in mind that the final diagnosis of prostate cancer is made only on the basis of a biopsy, when the gland is punctured with a needle for subsequent microscopic analysis of the tissue.
- Infections (prostatitis/abscess) MRI reveals acute or chronic prostatitis, helps to detect purulent complications at an early stage - prostate abscess, as well as concomitant vesiculitis
- Benign prostatic hyperplasia (BPH) itself is not a direct indication for MRI, but this study clearly visualizes glandular and stromal hyperplasia nodes, urethral compression, size and shape of the prostate, and also helps exclude malignant transformation (cancer).
- Congenital anomalies of the prostate gland
- Complications after pelvic surgery
PREPARATION FOR PROSTATE MRI
- The study is carried out on an empty stomach, with a full bladder.
- On the eve of the examination, you need to drink espumizan to reduce the amount of gas in the intestines, half an hour before the examination - 2 tablets of no-shpa
- Remove all jewelry, metal and electronic items from pockets, watches, etc.
- Warn staff about the presence of metal prostheses or electronic implants in the body
HOW IS A PROSTATE MRI DONE?
Examination of the prostate gland is done only on a high-field tomograph (field strength 1.5-3 Tesla). A conventional MRI scanner consists of a cylindrical tube located inside a large magnet. You will need to lie down on a table, which will place you in the center of the device, where you will need to be during the examination.
Before the test, a special radiofrequency coil will be placed on your body to read the structure of your body's tissues. Sometimes a special thin coil is placed inside the rectum, although such coils are rarely used in Russia.
Most often, the study is done with intravenous contrast; for this, a thin catheter is installed in a vein, through which a special drug containing gadolinium is injected during the study.
The scan is performed within 30-60 minutes. All this time you need to remain motionless.
After this, the data is processed by a radiologist, and you receive a conclusion with recommendations.
DESCRIPTION OF PROSTATE MRI BY PI-RADS
Currently, it is not enough to do an MRI of the prostate gland on a good tomograph. The modern standard of examination involves the formation of a radiologist’s conclusion made according to a special standard - this is the so-called report according to the PI-RADS v2.0 system. This report is necessary for a qualified urologist and serves to correctly determine further treatment tactics. Depending on the PI-RADS scores, the urologist decides whether to do a biopsy or not, choose a wait-and-see approach, or prescribe surgery.
Often, even after having an MRI of the prostate done on a high-quality MRI scanner, the patient does not receive a high-quality description using the PI-RADS system. But even in this case, you can get a description of PI-RADS from the National Teleradiological Network service, just send an MRI from a disk via the Internet for review, and get a high-quality conclusion made according to modern standards. Having received such a description, the urologist will choose a more reasonable treatment tactic.
WHAT DOES IT FEEL TO DO WITH A PROSTATE MRI?
During the examination, the device makes a loud noise, this is normal. You may also feel a slight warming of the body, this is not harmful to the body. Injection of the drug into a vein is usually not accompanied by any unpleasant sensations.
WHAT DOES MRI OF THE PROSTATE SHOW?
What does prostate cancer look like on an MRI?
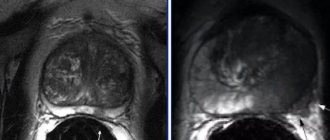
Prostate cancer looks like a lesion in its structure, with unclear contours, hypointense in T2-VI mode. If it is in the peripheral zone, it is characterized by limited diffusion on ADC maps. When contrast is administered, cancer is characterized by its early accumulation. Is it possible to miss prostate cancer on an MRI? MRI detects tumors of at least 5 mm in size; diagnosis of smaller tumors is unreliable.
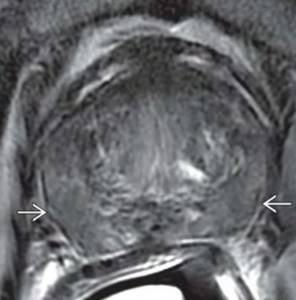
MRI of prostate cancer. Axial and sagittal tomograms reveal a volumetric formation of the prostate gland with low signal intensity, irregular shape, with tuberous edges, causing obstruction of the right ureter (hyperintense signal on the tomogram on the left) - carcinoma. https://radiopaedia.org/cases/locally-progressive-prostate-cancer
Prostatitis on MRI
The diagnosis of prostatitis is usually made clinically and by laboratory tests, and MRI is often performed to detect abscesses. There are focal and diffuse forms of prostatitis. Focal prostatitis appears as a linear or triangular hypointense area with poorly defined edges. Diffuse form: hypodense signal in the peripheral zone, decreased ADC values on diffusion-weighted tomograms. Prostate abscess: a mass formation containing pus, with a rim that accumulates contrast.
On an axial T2 VI tomogram in a patient with prostatitis, a diffuse decrease in the intensity of the peripheral zone is determined (from the book DI: Genitourinary, 2021).
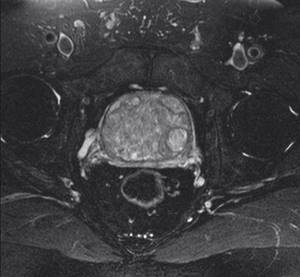
MRI for BPH
Benign hyperplasia: enlargement of the prostate due to stromal and glandular hyperplasia. MRI signs: prostate enlargement, expansion of the transition zone, multiple nodes, hyperintense signal (glandular hyperplasia), hypointense signal (stromal hyperplasia) with the presence of round or elongated nodules.
MRI (T2 VI) reveals a pronounced diffuse enlargement of the prostate with the presence of numerous nodes in the structure with different signal intensities (from the book DI: Genitourinary, 2021).
Prostate cysts on MRI
Degenerative (against the background of hyperplasia), cysts of the Müllerian duct, prostatic uterus, ejaculatory duct, retention cysts. On T1 WI, most cysts are hypointense (the signal intensity increases with infection/hemorrhage); on T2 WI, they are hyperintense. You can read more about prostate cysts here.
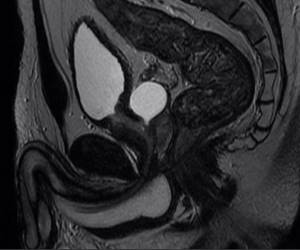
Sagittal MRI (T2 WI) visualizes a hyperintense cystic formation behind the bladder (ejaculatory duct cyst). https://radiopaedia.org/cases/ejaculatory-duct-cyst
Get an MRI of the prostate gland (prostate) in St. Petersburg
Vasily Vishnyakov, radiologist
Read more about Second Opinion
Read more about telemedicine
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists
How is an MRI done for prostate cancer?
To exclude the influence of intestinal peristalsis on MRI results, you need to prepare before the upcoming procedure: it is recommended to remove from the diet for a couple of days foods that cause increased gas formation (legumes, brown bread, carbonated drinks, etc.). On the morning of your scan, you should not eat for at least 4 hours before the scan. MRI of the prostate gland is performed with a full bladder, so you need to drink water 1 hour before the procedure and not go to the toilet.
It is necessary to arrive at the medical center in advance and undergo a preliminary consultation. Before starting the diagnosis, it is recommended to remove all jewelry, watches, and change into clothes without metal objects. The above may distort the operation of the tomograph.
The procedure takes place in a separate room. The patient is placed on the table of the device, the health worker helps the patient to take the correct position. During the examination, the laboratory assistant is in the next room, observing the process through the glass. On the monitor, the program displays section-by-section images of the prostate gland, reconstructed as a result of recording the responses of the patient’s cells to the action of the magnetic field.
The duration of the scan does not exceed 30 minutes, including intravenous contrast.
Upon completion of the study, the patient waits about an hour for the result and expert’s opinion.
Treatment of BPH
Conservative
- improvement of urine outflow due to relaxation of the bladder neck, urethra,
- reduction in gland size,
- improvement of the detrusor muscle of the bladder.
Combination pharmacotherapy is used, which is selected individually and adjusted during treatment by the urologist observing the patient.
Surgical
If conservative therapy is ineffective, BPH progresses, severe urinary disorders, an increase in the volume of residual urine, or the development of complications (stone formation, hematuria - red blood cells in the urine, renal failure, etc.), surgery is necessary.
The Clinical Hospital on Yauza practices a modern method of surgical treatment of prostate adenoma - endoscopic laser vaporization, in which access to the prostate gland is through the urethra, and excess gland tissue is evaporated by a laser.
MRI-guided robotic biopsy allows for more accurate diagnosis
In order to make a diagnosis of cancer and determine the malignancy of the formation, a biopsy is always necessary.
In a routine, traditional biopsy, samples are taken randomly from 12 different areas of the prostate gland. As a rule, after such a biopsy, the patient experiences complications: inflammation, pain and bleeding. The Docrates Clinic has begun to conduct a new biopsy method - robotic biopsy under MRI guidance. This method allows you to take material precisely from the formation under MRI control. And for such a biopsy, only 2-3 samples are enough (instead of 12). This method is more accurate than Fusion biopsy. MRI-guided robotic biopsy is performed under local anesthesia and is painless for the patient.
There is also a classification of prostate cancer by stages:
| Stage | T | N | M | G |
| I | T1a | N0 | M0 | G1 |
| II | T1a | N0 | M0 | G2-3 |
| T1b | N0 | M0 | Any G | |
| T1c | N0 | M0 | Any G | |
| T2 | N0 | M0 | Any G | |
| III | T3 | N0 | M0 | Any G |
| IV | T3 | N0 | M0 | Any G |
Preparation for magnetic tomography of the prostate gland
Before an MRI of the prostate is performed, the patient is prescribed a certain diet consisting of foods that do not cause gas formation. The fact is that a number of foods and drinks can cause distortion of the survey results. It is necessary to exclude from the diet:
- soda;
- alcohol;
- fatty foods;
- sweets.
Preparation for an MRI is accompanied by a cleansing enema. It is mandatory if the specialist prescribes diagnostics to the patient using a rectal coil, which is inserted into the rectum. At the same time, filling the bladder with fluid is mandatory for everyone.
Treatment
Dynamic observation (delayed treatment)
indications for dynamic observation:
- Localized prostate cancer (T1a - T2b N0M0)
The patient's life expectancy is less than 10 years
- Well differentiated tumor
- Severe concomitant diseases
Surgery
Surgery (radical prostatectomy) is the most radical treatment method and is considered the method of choice in the treatment of localized prostate cancer.
Radiation therapy
Cryotherapy
Brachytherapy (intrastitial radiation therapy)
Hormone therapy
The goal of hormonal therapy for prostate cancer is to increase survival rates and improve the quality of life of patients. Hormonal therapy as an independent option is carried out for palliative purposes, but it can be used in combination with radical surgical or radiation treatment as a combination antitumor therapy.
Methods of hormonal therapy:
- Bilateral orchidectomy.
- Therapy with LH releasing hormone agonists
- Therapy with LH-releasing hormone antagonists
- Estrogen therapy
- Maximum (combined) androgen blockade
- Monotherapy with antiandrogens
Bilateral orchidectomy
Bilateral orchidectomy (surgical castration) is the main method (gold standard) of hormonal therapy for prostate cancer.
Luteinizing hormone releasing hormone agonists
LH releasing hormone agonists are synthetic analogues of native hypothalamic LH releasing hormone. after the administration of these drugs, there is a short-term increase in testosterone concentration on days 3-5 (flare syndrome), followed by a decrease to the post-castration level on days 21-28. To prevent flare syndrome in patients with metastatic prostate cancer, antiandrogens are prescribed before the administration of an LH-releasing hormone agonist and during the 1st week of therapy.
Currently, the following LH-releasing hormone agonists are used for the treatment of prostate cancer:
- Goserelin
- Triptorelin
- Buserelin
Treatment with LH releasing hormone agonists is long-term.
Estrogens
Historically, estrogens were the first group of hormonal drugs that were used to treat prostate cancer; however, due to severe side effects, they are now rarely used in clinical practice.
Antiandrogens
- Steroidal antiandrogens:
- Cyproterone
- Megestrol
- Chlormadinone
- Nonsteroidal antiandrogens:
- Flutamide
- Nilutamide
- Bicalutamide
Drugs of other classes
- Ketoconazole is an antifungal drug that inhibits the synthesis of androgens by the adrenal glands. Ketokenazole is a second-line drug.
- Aminoglutethimide - also inhibits the production of androgens by the adrenal glands by blocking cytochrome P-450.
Treatment of hormone-refractory prostate cancer
Hormone-refractory is considered to be the stage of the tumor process at which progression occurs (two consecutive increases in PSA levels by 50% above the minimum value) against the background of post-castration testosterone levels.
For the treatment of hormone-refractory prostate cancer, mono- and polychemotherapy is used in various regimens. The drug Estramustine is used.
Further management
- Determination of PSA level, DRE and routine clinical examination every 3 months. for 1 year, every 6 months during the 2nd and 3rd years, then annually.
- An increase in PSA levels after radical prostaectomy >0.2 ngml indicates relapse of the disease.
- A palpable tumor node and an increase in PSA level after the minimum value achieved after radiation therapy are defined as disease recurrence.
- Biopsy of a recurrent tumor under transrectal ultrasound guidance is indicated when planning the second line of radical treatment.
- For bone pain, skeletal scintigraphy is indicated (regardless of PSA level).
Contraindications for prostate MRI
- the presence of ferromagnetic implants in the human body;
- presence of IVR in the body;
- endoprosthetics (the study is carried out only if there is a certificate for the endoprosthesis, which clearly indicates the composition of the foreign body and states that its presence does not prohibit MRI).
The cost of diagnostics, as well as MRI of other organs and tissues, depends on the size of the anatomical area being studied and the required thickness of sections. MRI of the prostate with contrast costs twice as much, because... 2 studies are carried out one after another. Before the second, a contrast agent is injected into the vein.
Morphological classification according to the Gleason scale
According to the Gleason classification, the degree of tumor differentiation is assessed on a 5-point scale:
- 1 point - the most highly differentiated tumor;
- 5 points - poorly differentiated tumor.
For a tumor with a heterogeneous morphological structure, it is customary to distinguish the most common histological gradation (primary score) and the next most common gradation of differentiation (secondary score). When adding the primary and secondary scores, the Gleason score is obtained (from 2 to 10 points).
The Gleason classification is currently the most common and has important prognostic significance for predicting the pathomorphological stage of the process and assessing the results of treatment of prostate cancer.
Indications for the procedure
Basically, MRI of the prostate is performed to diagnose a serious disease such as cancer. After a biopsy (histological examination), if the test result is positive, the patient is sent for a procedure such as MRI diagnostics of the prostate gland in order to determine the boundaries of the spread of cancer cells and whether they extend beyond this area of the body. In addition, MRI is prescribed if there are signs of prostatitis (inflammation of the prostate), as well as benign prostatic hyperplasia (prostate adenoma).
If the disease is suspected of spreading, doctors may order an MRI scan to detect:
- damage by cancer cells to the lymph nodes;
- the presence of tumor cells in the pelvic organs and bones;
- metastatic lesion of the bladder.
MRI of the prostate gland is recommended for every man, regardless of the disease that doctors suspect. Using the procedure, you can identify not only complex diseases that require immediate treatment, but also congenital pathologies that do not manifest symptoms.