MRI of the liver (or “cholangiography”) is an instrumental high-precision diagnostic method aimed at visualizing the liver and biliary organs. MRI of the liver and gallbladder allows you to determine and evaluate their condition and identify existing pathologies. Along with its high precision, the procedure is absolutely safe and painless.
If you need to perform an MRI of the liver with contrast, contact the CELT clinic! We employ leading specialists, doctors of the highest category, capable of conducting diagnostics at a decent professional level.
MR tomography of the liver with intravenous administration of a hepatotropic contrast agent (Primovist) - RUB 17,000.
15-45 minutes
(duration of procedure)
Indications
- Painful sensations localized in the area of the right hypochondrium;
- Preoperative preparation/postoperative monitoring;
- Pain sensations localized in the upper abdomen;
- Previously performed surgery on the abdominal organs, during which the bile ducts were damaged;
- Clinical signs of impaired production of bile and pancreatic juice;
- The presence of obstacles in the ducts of a mechanical nature, their differential diagnosis.
Contraindications
- Allergic reactions to contrast agent;
- Pregnancy and lactation;
- Implants in the patient's body made of metal.
Is it possible to do an MRI of the liver?
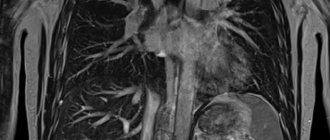
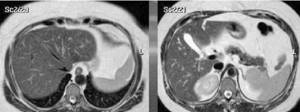
Signs of cirrhosis: yellowness of the skin, enlarged abdomen due to ascites, visualization of convoluted dilated veins on the anterior abdominal wall - “jellyfish head”, multiple dilated vessels are visible on the MRI scan
The doctor can select the parameters of magnetic resonance scanning, which makes it possible to diagnose diffuse and focal diseases of the biliary system. Initially, with characteristic clinical manifestations and an increase in liver tests (bilirubin, AST and ALT), an ultrasound examination is performed. The danger of liver cancer and cirrhosis lies in the absence of symptoms in the early stages. The doctor will refer you for an MRI if the patient has:
- yellowing of the skin;
- pain in the abdomen, right hypochondrium;
- unexplained nausea, vomiting, stool disorders (stools are light, soft, oily with a foul odor), bleeding (nasal, gingival, gastrointestinal due to portal hypertension and disruption of the coagulation system);
- weight loss with normal diet, weakness, decreased concentration;
- spider veins, “liver” (crimson) palms and tongue, itchy skin, dark urine, swelling of the lower extremities;
- signs of ascites, etc.
MRI of the liver is an expert diagnostic method. Scanning is performed when ultrasonography results are questionable and there is a need to gain a more complete understanding of the genesis of the pathological process. Use as a screening (mass) study is limited by the relatively high cost of the procedure.
Is liver MRI done for children? Young patients can be tested after reaching one month of age. The diagnostic procedure will not affect health or further development: no biochemical reactions occur in the cells, and there is no ionizing radiation exposure.
What does an MRI of the liver show?
Liver cysts on magnetic resonance scan
The tomograms show:
- shape, contours, structure and size of the organ;
- narrowing of the bile ducts, stone formation;
- increase in the diameter of the portal vein, portosystemic collaterals, varicose veins of the abdominal cavity, esophagus;
- ascites (visualized better on MRI than on CT);
- focal nodular hyperplasia;
- lymphadenopathy and severity of changes;
- benign and malignant formations, the relationship of tumors with nearby tissues;
- stage of fibrosis;
- fatty infiltration;
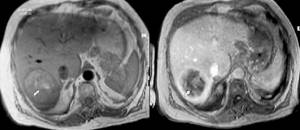
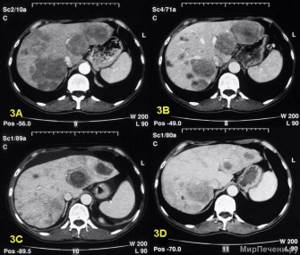
MRI of the liver without contrast and after gadolinium administration, T1 VI, abscess (arrow)
- congenital and acquired cysts, including parasitic ones, hemangiomas, hamartomas;
- abnormalities of the biliary system organs;
- liver sarcoidosis;
- abscesses;
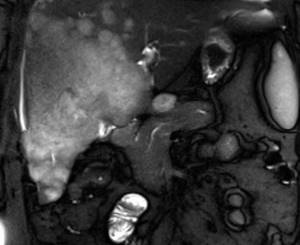
- hyper- and hypovascular metastatic lesions, including those of a secondary nature (screenings of tumors from other organs - intestines, stomach, breast, ovaries, kidneys, lungs), etc.
MRI image of the liver: hepatocellular cancer
An MRI study is carried out to assess the effectiveness of therapy, as part of preoperative preparation to study anatomical features. Magnetic resonance scanning has found application in transplantology to examine the donor’s liver for the detection of hepatocellular carcinoma.
One of the main tasks when prescribing MRI of the biliary system is to determine whether the lesion is benign or malignant, on the basis of which to choose patient management tactics. MRI scanning allows you to avoid invasive diagnostic procedures - laparotomy and puncture biopsy.
Indications for the study
A referral for a liver scan using MRI is usually given by a hepatologist or gastroenterologist. The reasons for referral for tomography may be symptoms of organ pathology: complaints of pain in the right hypochondrium, loss of appetite, yellowing of the whites of the eyes, darkening of urine, etc.
Also, a study may be prescribed in the following cases:
- if a malignant neoplasm is suspected in the tissues of the liver or organs closest to it;
- hepatomegaly (an increase in the size of an organ) is diagnosed, the cause of which is illness or if the cause is unknown;
- to clarify data from other diagnostic methods;
- there is reason to suspect that stones or salt deposits have formed in the organ, interfering with the flow of normal processes;
- to clarify the etiology of hepatitis and the consequences of this disease for the organ;
- liver cancer has been previously diagnosed and there is a threat of metastatic damage to nearby organs;
- assessing the effectiveness of treatment, for example, after chemotherapy or surgery;
- assessment of the condition of the liver in cirrhosis, etc.
MRI not only diagnoses diseases, but also monitors the progress of treatment.
Is liver cirrhosis visible on MRI?

Changes in tissue architecture due to the destruction of hepatocytes and the formation of regenerative nodules, due to which the surface of the organ becomes wavy
Cirrhosis is the terminal stage of a number of chronic liver diseases, accompanied by hepatocellular necrosis (death of functioning cells). Pathology is diagnosed using ultrasound, CT and MRI. These imaging modalities can be used to detect possible complications such as portal hypertension or hepatocellular carcinoma.
There are many causes of liver cirrhosis. Sometimes the pathogenetic factor cannot be determined, in which case they speak of an idiopathic form of the disease.
The death of hepatocytes and the degeneration of normal parenchyma into fibrous tissue occurs when:
- viruses that cause modification of organ tissue (mainly chronic hepatitis C);
- abuse of alcohol, chemical substances;
- sclerosing or biliary cholangitis;
- a number of pathologies - hemochromatosis, Wilson-Konovalov disease, alpha-1-antitrypsin deficiency, cystic fibrosis, etc.;
- autoimmune liver damage;
- constrictive pericarditis, veno-occlusion, heart failure, etc.
Regardless of the cause, the clinical manifestations of liver cirrhosis are determined by the stage of the disease: initially there are no symptoms.
MRI confirms cirrhosis:
- uneven contour of the organ;
- detection of specific nodules;
- diffuse hepato- and splenomegaly, liver enlargement occurs against the background of dilatation of the bile ducts, as the disease progresses, the organ may thicken and shrink;
- expansion of the diameter of the portal, splenic, superior mesenteric veins - increased signal intensity on T2 VI;
- formation of portosystemic collaterals;
- thickening of the gallbladder wall - signal intensity is reduced on T1 and T2 VI;
- expansion of the lobar and common hepatic ducts;
- accumulation of free fluid in the abdominal cavity;
- lymphadenopathy, etc.
In addition to demonstrating morphologic changes in cirrhosis, MRI is used to evaluate vascular structures for patency or tumor invasion. T1 WIs are valuable for studying anatomical details, while T2 WIs are more sensitive for detecting diffuse lesions, cysts and hemangiomas.
In difficult cases, it is possible to perform a biopsy followed by morphological examination.
Indications and contraindications for CT scan of the liver
An unpleasant feature of the development of liver diseases is the fact that it contains a small number of nerve endings, so a person cannot always feel that something abnormal is happening to the organ. However, if the patient often complains of pain and heaviness in the liver area, bloating, metallic taste, nausea and bitterness in the mouth, such symptoms are an indication for an ultrasound, based on the results of which the doctor may prescribe a referral for a computed tomography scan.

Other indications for liver CT include:
- detection of organ enlargement for unknown reasons;
- the need to clarify the preliminary diagnosis, for example, cirrhosis or hepatitis;
- identification of pathological formations, the need to clarify their size and extent of distribution;
- suspicion of tumor diseases, the appearance of metastases;
- presence of disturbances in the functioning of liver vessels;
- conducting surgical interventions: surgeons prescribe CT scans before surgery, in preparation for it, and after it to assess its effectiveness;
- impaired blood flow and thrombosis in this part of the body;
- infectious and inflammatory processes, polycystic liver disease;
- chronic alcoholism, which, as is known, often provokes irreversible processes in the liver;
- previous abdominal injuries.
There are also situations where the potential risks of tomography are higher than the likely value of the data obtained in the process, or when, due to the nature of the human body, the information content of the study will be too low. In the presence of certain diseases and conditions, CT scanning can generally harm a person. Tomographic scanning of the liver is prohibited:
- for pregnant women and nursing mothers, due to the risk of exposure to the fetus;
- for children under 3 years of age, so as not to expose a very young body to x-rays;
- for diabetes mellitus, acute forms of bronchial asthma;
- in the presence of iodine intolerance, kidney or liver failure, if we are talking about computed tomography with contrast;
- in case of severe general condition of the patient, for example, if he is connected to life support devices;
- in diseases and pathologies associated with the manifestation of hyperkinesis: in such cases, the patient will not be able to ensure complete immobility during the scan, which is why the value of the resulting images will be almost zero.
For obese patients, liver CT remains questionable. On the one hand, it is known that ultrasound is practically uninformative for them, since it poorly visualizes the organ due to the presence of a pronounced subcutaneous fat layer. On the other hand, computer tomographs, in general, are simply not designed to weigh more than 140-180 kilograms. In such cases, the doctor decides at his own discretion how exactly the patient will be examined.
Preparing for an MRI of the liver

Tell your doctor about your ongoing medication use, allergic reactions, diagnosed kidney failure, or implanted metal parts in your body.
It is difficult for the patient to choose the type of examination on his own; it is necessary to consult a doctor for a referral. Symptoms of early-stage liver disease are nonspecific, so the abdominal and retroperitoneal organs are often evaluated in one diagnostic procedure.
Excessive accumulation of gas in the abdomen, increased peristalsis, and overstretching of the intestinal walls with feces interfere with obtaining high-quality images and accurate interpretation of the results. It is recommended to follow a diet low in carbohydrates and fiber 2-3 days before the magnetic resonance scan. Exclude from the diet:
- fresh (without heat treatment) vegetables and fruits, herbs;
- marinades, spices;
- smoked meats;
- fatty meats and fish;
- confectionery;
- black bread;
- mushrooms;
- seeds and nuts;
- milk and derivatives of high fat content - cream, sour cream, yogurt;
- alcohol, kvass, strong tea and coffee, jelly, lemonade, sparkling water.
Prepare dishes by boiling or baking in the oven. Preferably, minced meat products, water-based porridges, dry biscuits, clear broths, unsweetened compotes, mousses, diluted juices, still water, etc.
Unless otherwise agreed, you must arrive for the procedure on an empty stomach: the last meal is allowed 4-6 hours before diagnosis. Even a light snack causes contraction of the gallbladder; in a full state, the contours of the organ and internal changes are better visualized.
To prevent autonomic reactions - nausea, dizziness, drooling - a light breakfast is acceptable before an MRI of the liver with contrast. Nursing mothers should prepare a supply of milk for 2-3 times, and express and dispose of the excess. An increased drinking regime promotes faster removal of the dye from the body.

Drugs prescribed for long-term treatment are taken as usual
The attending physician will tell you specific preparation measures for MRI of the liver, taking into account the clinical situation. You may be assigned:
- antispasmodics;
- sorbents;
- enzymes;
- laxatives;
- sedatives;
- drugs to reduce flatulence, etc.
Colon cleansing with an enema may be required for patients suffering from chronic constipation (do not use without the recommendation of the attending physician).
Take with you your passport, compulsory medical insurance/voluntary medical insurance policy (subject to payment for scanning by the insurance company), hospital discharge notes, results of previously performed CT, MRI, PET, ultrasound, etc. - everything that can help in determining the diagnosis and assessing changes in dynamics.
Contraindications for MRI examination
MRI of the liver and biliary tract has a number of contraindications, including: the presence of neurostimulators and pacemakers; built-in large metal implants; hemostatic clips built into the brain; the presence of ferromagnetic and electronic implants of the middle and inner ear.
Among the relative indications it is worth noting: the presence of claustrophobia; pregnancy, especially in the first three months; the presence of severe pain that prevents you from lying still for one hour; the need for physiological constant monitoring; presence of prosthetic heart valves.
Titanium, which is often used in medicine recently, is completely safe for the procedure. Also, the study will not be hindered by the period of breastfeeding, menstruation, or the presence of intrauterine devices. A large percentage of devices and equipment introduced into the body for medical reasons interact well with an MRI machine.
It is important, before starting the procedure, to tell the doctor about the presence of foreign bodies in the body, because only he can say with certainty whether it is possible to undergo the study, or whether it is recommended to choose another alternative method.
How to do an MRI of the liver

For the diagnostic procedure, wear loose clothing without metal components: this measure will prevent artifacts in the images and allow you to feel comfortable
The stages of magnetic resonance imaging are standard:
- The patient arrives at the clinic in advance; time is needed to fill out documentation, questionnaires to identify contraindications, and deposit items containing metal for storage.
- The X-ray technician escorts the patient to the diagnostic room and, after instructions, places him on the tomograph table. To avoid accidental movements, the limbs are fixed with soft belts and bolsters. A special grid is installed over the abdomen to enhance the magnetic field in the area of interest.
- When contrast is planned, a vein is catheterized, and the drug is supplied automatically during certain phases of the study. After a series of native scans, there is a break; waiting is necessary for the chelated gadolinium to flow through the bloodstream to the abdominal organs.
- After completing the study, the catheter is removed from the vein and an aseptic dressing is applied.
The operation of a magnetic resonance imaging scanner is accompanied by technical noise; unpleasant sounds can be neutralized using earbuds or headphones. Medical staff monitors the progress of the diagnosis through a window from an adjacent room. In the event of extraordinary situations (sudden attack of claustrophobia, allergy to contrast, fainting, etc.), the patient has a special button at hand for communication. The result of an MRI of the liver can be collected within an hour. The patient receives a disc with a recording in the international dicom format and a form with a conclusion.
Order of conduct
The patient, upon entering the office, removes all metal objects and lies down on the tomography table, which is placed inside the device.
During the study, a person does not experience any discomfort while lying quietly in the device for half an hour. In some cases, an attack of claustrophobia may occur, but you can combat it by talking to a doctor using a special microphone built into the device.
Sometimes the study is extended to 1-1.5 hours if it is necessary to obtain more accurate information. It is important to remain still during this entire time so that the pictures are of high quality.
If MRI is performed with contrast, then before the procedure a contrast agent is injected into the patient’s vein, which is one of the stages of preparation for the study.
Interpretation of MRI photographs of the liver
Magnetic resonance scan of the abdominal organs, normal, with T2 VI the liver has a low signal intensity
The interpretation of the study results is carried out by a radiation diagnostics doctor (radiologist), focusing on the generally accepted norms of the anatomical atlas. Independent interpretation of MRI of the liver is not available to an untrained person.
The organ has a double blood supply system. 25% comes from the branches of the hepatic artery, 75% from the portal vein. The organ has eight segments, the zones are limited by the main vessels. Sizes vary and are related to gender, age, and individual characteristics of a person.
In the absence of pathology, the liver is located usually, not enlarged, and the structure is homogeneous. The diameter of the portal vein is normal, the ducts are not dilated, without filling defects.
What pathologies can a computed tomography scan of the liver detect?

The results of a CT scan of the liver are pictures and images, analyzing and studying which, a radiologist can identify the following diffuse changes in the liver:
- various neoplasms: cancer, hemangioma, adenoma, other types of tumors;
- liver abscess is a purulent inflammation that affects the tissues of the organ and leads to the formation of a purulent cavity in it;
- signs of liver cysts, the appearance of which may be associated with trauma (hematomas, seromas and liver bruises) of other types of cysts;
- presence and extent of spread of metastases;
- echinococcosis is a parasitic lesion of an organ caused by the proliferation of a parasitic infection in it;
- signs of liver cirrhosis;
- signs of infectious or viral lesions, such as hepatitis.
In addition to pathologies and disorders, CT scan of the liver also shows the functional characteristics of the organ, as well as the changes found in it - tissue density, size, location of tumors or metastases, their depth.
CT diagnostics
During X-ray scanning, a computer tomograph creates a series of images (cross sections) of the liver and collects from them a three-dimensional image with a good degree of detail. The procedure can be performed either with or without contrast. But for liver cancer, CT with contrast (iodhexol, ultravist) is much more informative and gives more accurate results.
During the procedure, a helical scan is usually performed first and only then contrast is injected and a second helical scan is performed, with another repetition after 30-40 seconds.
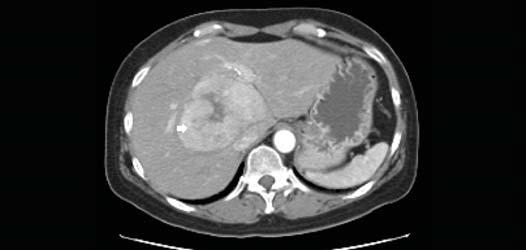
Liver cancer can look different on a CT scan. This can be a single or multiple lesion, having the same low density in relation to parenchymal tissue. The lesions may contain areas of necrotic and fatty tissue, calcifications, fibrous formations and choroid plexuses.
HCC is characterized by expansion of surrounding tissues or penetration (germination) into them and the formation of secondary foci. Large tumors are quite visible and have a distinct specific structure.
Causes of cirrhosis
In 100% of cases, the formation of cirrhosis is preceded by hepatitis, which can be asymptomatic for years or even decades. Long-term hepatitis leads to the formation of fibrosis (replacement of liver cells with connective tissue). At a certain point, the destruction becomes irreversible, and the organ stops working. The most common cause of this disease is hepatitis, caused by the following factors:
- taking drugs and toxic medications;
- viral hepatitis;
- diabetes mellitus and some other diseases;
- metabolic disorders;
- violation of the outflow of bile;
- storage diseases;
- autoimmune processes, etc.