Epidemiology
- In terms of prevalence in the world, malignant neoplasms of the neck and head occupy 6th place.
- The main localizations of the organs of the neck and head are the larynx and hypopharynx.
- In Russia, laryngeal cancer ranks 5th in terms of incidence.
- The highest incidence is in Thailand, Poland, Ohio (USA), Italy, France, and Spain.
- Men are more susceptible to the disease – 1 in 10.
- Most often - in 95% of cases - among malignant lesions of the larynx, squamous cell carcinoma is diagnosed.
- Among all malignant neoplasms of the neck and head, this disease is in 1st place.
- In the general structure of cancer pathologies – 2.6%.
- The incidence rate per 100,000 people is 4-6.
- Low incidence (that is, less than 2 per 100,000 people) is observed in Japan, Norway, and Sweden.
We invite you to familiarize yourself with visualized statistics for the United States for 1992-2015. The graph shows deaths and the number of newly diagnosed cases.
Definition
The larynx is the area of the throat that is located between the trachea and the root of the tongue. Its structure contains vocal cords, the vibration of which produces the human voice.
To determine the prevalence of the process, it is necessary to take into account the anatomy of the larynx. It is divided into 3 sections according to a number of features: differences between the mucous and submucosal layers, lymph and blood circulation, etc. Let's consider the main sections of the organ:
- Upper, or vestibular. It includes the following structures: aryepiglottic ligaments on the laryngeal side, Morganian ventricles, false vocal cords, epiglottis.
- Average. This is the area where the true vocal cords are located.
- Lower, or subglottic.

This gradation largely determines the differences in the course of the disease. Most often, the fold and supraglottic sections are affected (50-70%), while the incidence in the fold section is 30-40% of cases, and in the subglottic section – 3-5%. The most malignant course is if the tumor affects the vestibular region. In this case, metastases develop with a frequency of 40-60%. The most favorable prognosis is if the fold section is affected. Metastases are diagnosed in 5-12% of cases. If the subglottic region is affected by a neoplasm, the indicators are approximately the same.
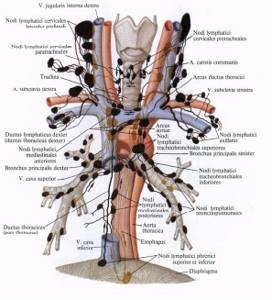
Features of the development of metastases, depending on the location of the oncology
Supraglottic section
There is a well-developed lymphatic network here, which helps the tumor quickly spread throughout the local and regional localization. Metastases mainly affect the upper and middle group of lymph nodes located in the deep jugular chain - 50-60% of cases. Metastases are localized:
- in 57% of cases on the side of the tumor;
- in 9% - on both sides of the larynx;
- in 6.3% - contralaterally, that is, on the side opposite to the tumor.
Vocal folds
Due to the low lymph circulation, metastases are rarely observed here. In 5-12% of cases they are found in the middle deep jugular lymph nodes.
Subglottic department
Regional metastases occur in 5-12% of cases. Moreover, in 20% of cases they develop in the pretracheal and prelaryngeal lymph nodes. Lymph moves towards the lower deep jugular lymph nodes, where metastasis is also diagnosed.
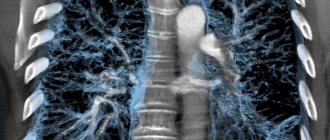
Distant metastases are most often diagnosed in the ribs, lungs, and mediastinum.
Precancerous diseases
Let's consider the pathologies that precede laryngeal cancer:
- laryngitis, which a person suffers from in a chronic form for many years;
- a special role in the appearance of this pathology is played by: most often - papilloma, which has existed for a long time, and leukoplakia of the mucous membrane lining the larynx;
- pachydermia;
- dyskeratoses;
- cystic formations on the laryngeal ventricles;
- broad-based fibroma;
- chronic inflammation that cannot be treated and is caused by smoking, alcoholism, and syphilis.
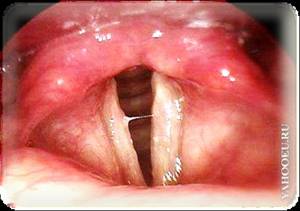
Laryngitis
Laryngitis

Papilloma

Papilloma

Leukoplakia
Leukoplakia
Risk factors
It is important to understand that the presence of these factors does not mean that you will definitely encounter cancer, however, their absence does not guarantee that you do not have cancer.
The main factors that increase the risk of developing laryngeal cancer:
- Alcohol. Those who regularly drink strong alcoholic drinks are 6 times more likely to develop oral cancer. The combination of smoking and alcohol is very dangerous.
- Smoking. The more experience a smoker has and the more cigarettes he smokes, the higher the risk of getting sick. Passive smoking also increases the risk of cancer.
- Working conditions. Risk factors include: working in conditions of high dust (especially if the dust contains harmful chemicals, radioactive substances, metals), in contact with isotopes and at high temperatures.
- Human papillomavirus (HPV). Neoplasms with the HPV18 and HPV16 virus subtypes were considered HPV-positive.
- Wrong diet.

Confirmation that alcohol and smoking increase the risk of developing the disease was found in studies that examined how the p53 tumor suppressor gene behaves. According to these studies, among all patients with laryngeal cancer, a mutation of this gene was detected in 42%. In those who drink and smoke at the same time, the mutation was observed in 58% of cases. For those who smoke but do not drink – 33%. In non-drinkers and non-smokers, the mutation occurred in only 17% of cases. In addition, in non-smokers and non-drinkers, the p53 mutation was observed in a DNA region that is more typical for endogenous mutations.
Decoding the results
The result is deciphered by a radiologist who records what he saw in the conclusion. With radiography, the conclusion is supplemented with photographs; fluoroscopy gives an idea of what the doctor saw in real time on the monitor. A narrowed tracheal lumen may indicate congenital cartilage hypoplasia, tracheostenosis. Tumors on X-rays are visible as enlargements of parts of the organ and deformations of the lumen in their locations. When the trachea is displaced, it is necessary to find the cause, which usually lies in a nearby organ. On a contrast X-ray of the trachea, tumors and inflamed nodes can be seen.
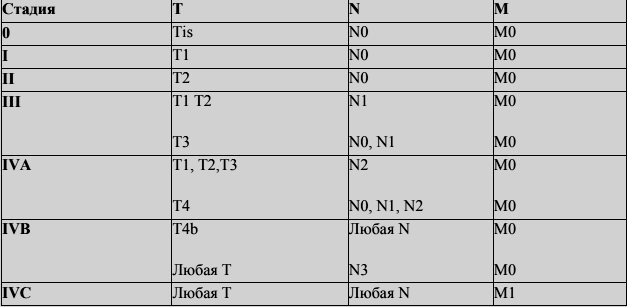
Stages of the disease
Let's consider the TNM clinical classification. In accordance with it, the symbol N indicates whether there are metastases in the regional lymph nodes (L/N):
- NX – there is not enough data to evaluate regional hospitals;
- N0 – there are no signs of metastasis in regional lymph nodes;
- N1 – metastases are noted in one lymph node located on the affected side, measuring up to 3 cm in the greatest dimension;
- N2 – on the affected side there are metastases in one lymph node up to 6 cm in the greatest dimension, or metastases up to 6 cm in the greatest dimension are present in several lymph nodes on the side of the tumor, or metastases up to 6 cm in the greatest dimension are located in the lymph node at both sides;
- N2a – on the affected side in one lymph node there are metastases up to 6 cm in greatest dimension;
- N2b – on the affected side in several lymph nodes there are metastases up to 6 cm in greatest dimension;
- N2c – metastases up to 6 cm in greatest dimension are located on both sides or opposite the tumor in the lymph node;
- N3 – metastases more than 6 cm in greatest dimension are detected in the lymph node. The left midline is referred to as the nodes on the affected side.
The M symbol indicates whether there are distant metastases:
- MC – there is no data to evaluate distant metastases;
- M0 – no signs of distant metastases were found;
- M1 – distant metastasis is noted.
Classification of tumors according to the T symbol, taking into account localization in the larynx
| Supraglottic region | T1 | The tumor is located only in the supraglottic part, the vocal cords are mobile |
| T2 | The mucosa of several anatomical areas of the ligamentous or supraglottic part or the area outside the supraglottic part (medial wall of the pyriform sinus, mucous membrane of the tongue root, etc.) is affected without fixation of the larynx | |
| T3 | The neoplasm is limited to the larynx with fixation of the vocal cords and/or extended to the posterior part of the laryngeal cartilage, tissue in the preepiglottic region; erosion of the thyroid cartilage is minimal | |
| T4a | The tumor affects the thyroid cartilage and/or has spread to the soft tissues around the larynx: esophagus, neck (external and deep muscles), thyroid gland, ribbon muscles, tongue | |
| Т4b | The neoplasm affects the mediastinum or the lining of the carotid artery, as well as the prevertebral region | |
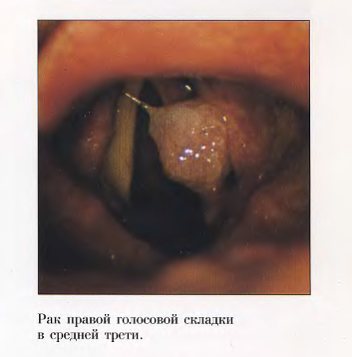
| Ligamentous department | T1 | The neoplasm is limited to the vocal cords and does not impair their mobility; the posterior and anterior commissures may be involved in the process |
| T1a | The tumor is limited to one vocal cord | |
| Т1b | Both vocal cords are affected | |
| T2 | The pathology affects the sub- and/or supraglottic zones, impairs the mobility of the vocal cords | |
| T3 | Only the larynx is affected with fixation of the vocal cords and/or the tumor grows into the supraglottic region and/or provokes erosion of the thyroid cartilage | |
| T4a | The tumor involves the tissues around the larynx (ribbon muscles, trachea, deep/external muscles of the tongue, neck, esophagus, ribbon muscles) or thyroid cartilage | |
| Т4b | The neoplasm has grown into the mediastinum, prevertebral space or carotid artery sheath | |
| Subglottic region | T1 | The tumor is limited to the subglottic region |
| T2 | The tumor affects one or two vocal cords, mobility is free or limited | |
| T3 | The tumor does not extend beyond the larynx with fixation of the vocal cords | |
| T4a | The neoplasm grows into the thyroid or cricoid cartilage and/or affects the tissues located around the larynx (thyroid gland, neck, including the external/deep muscles of the tongue, trachea, ribbon muscles) | |
| Т4b | The tumor spreads to the prevertebral space, the carotid artery sheath, or the mediastinum |
Table of general grouping of the disease by stages
Symptoms and clinical picture
The clinical picture of the disease varies depending on the area affected by the tumor. Let's look at each of them.
Vestibular cancer (seen in 60-65% of cases)
During the first few months, patients experience:
- sore throat;
- dryness;
- sensation of the presence of a foreign body.
Later the following symptoms appear:
- swallowing disorder;
- fatigue;
- dull voice;
- pain when swallowing;
- morning pain when swallowing, and later - constant.
It is worth noting that such symptoms may also indicate the presence of laryngitis and pharyngitis.
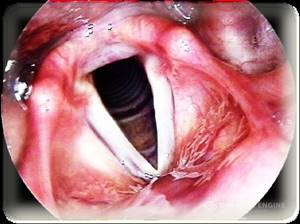
When the vocal tract is affected (occurs in 30-35% of cases)
The clinical picture of damage to this area is as follows:
- weakness and hoarseness of voice;
- rapid fatigue during vocal stress;
- later – difficulty breathing, aphonia.

Subvocal department
The following symptoms are characteristic of damage to this area:
- frequent coughing attacks accompanied by difficulty breathing.
The tumor is characterized by an endophytic type of growth, as well as a tendency to grow down and to the cartilaginous structures of the trachea.
In what cases is an x-ray of the larynx prescribed?
The need for a diagnostic procedure will be determined by an otolaryngologist. Direct indications for the study are the following conditions:
- trauma to the neck area;
- possible presence of a foreign object;
- suspected injury during tracheal intubation;
- assessment of the condition of the organ after a chemical or thermal burn;
- visualization of the state of the vocal folds during their paresis;
- the likelihood of having cystic and other types of neoplasms;
- whooping cough, laryngitis and other types of infectious processes localized in the larynx.
Regarding contraindications, diagnosis has no absolute restrictions. It is not recommended for use during pregnancy, in particular in the early stages. If necessary, it is carried out during lactation. After the procedure, it is recommended to express breast milk.
Diagnostic methods
First, let's present the differential diagnosis table
| Form of the disease | Clinical picture |
| Papilloma in the larynx | Usually occurs on the vocal cords, less commonly affects the epiglottis, finely lumpy, pale gray, the patient experiences hoarseness |
| Leukoplakia | A white spot with an uneven surface is found on the vocal cords; most often it is located behind the arytenoid cartilaginous structures, characterized by impaired phonation and coughing. |
| Contact form vocal process fibroids | Located in the back parts of the vocal folds, on one of them it resembles a hammer, on the other - an anvil, the patient’s voice changes |
| Laryngeal fibroids | Located in the anterior third of the vocal cords, sometimes have a wide base and arise from the laryngeal ventricle or vestibular ligament |
Diagnosis of this disease includes physical and instrumental examination methods.
Physical:
- collection of anamnesis of life and illness;
- examination and palpation (palpation) of the lymph nodes and larynx.
Instrumental:
- laryngoscopy (indirect);
- fibrolaryngoscopy, during which a targeted biopsy is performed;
- Ultrasound (performing puncture of lymph nodes under ultrasound control);
- Trepan biopsy of lymph nodes followed by histological examination of the biomaterial, which is crucial for making a diagnosis in oncology.
Let us consider diagnostic methods in detail and describe their features.
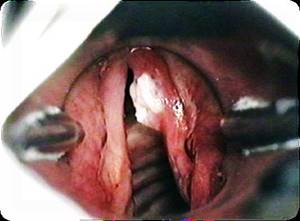
Laryngoscopy
- Indirect. It is used to determine the location and boundaries of the neoplasm, its growth patterns, the color of the mucosa, its integrity, the size of the lumen of the glottis, the level of mobility of the vocal folds, as well as the presence of inflammation of the cartilage and perichondrium of the larynx (chondroperichondritis).
- Fibrolaryngoscopy. Allows you to examine parts of the larynx that are not visible during direct laryngoscopy (epiglottis, laryngeal ventricles, anterior commissure, lining). During this procedure, a targeted biopsy is performed.

Laryngoscopy
X-ray techniques
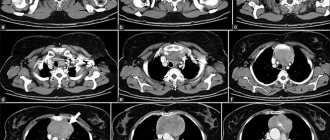
The patient undergoes the following examinations:
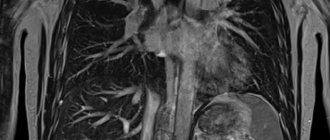
- MRI/CT of the soft tissues of the neck using intravenous contrast - provides data on the spread of the pathological process throughout the parts of the larynx, and also provides information on the regional lymphatic collector;
- X-ray of the chest organs or CT scan of the chest and abdominal cavities using contrast.
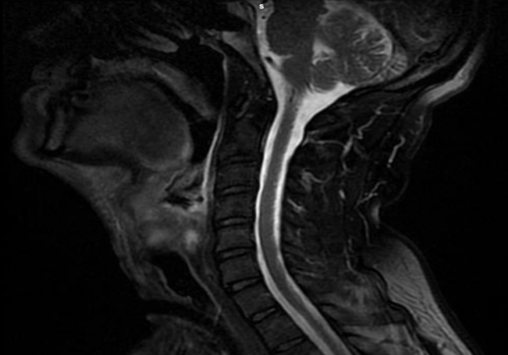
X-ray research methods
X-ray research methods
Histological examination
In accordance with the histological structure, in 98% of cases, laryngeal cancer is represented by non-keratinizing or keratinizing squamous cell epithelium. Adenocarcinoma is less commonly diagnosed. In extremely rare cases (0.4%) – sarcoma.
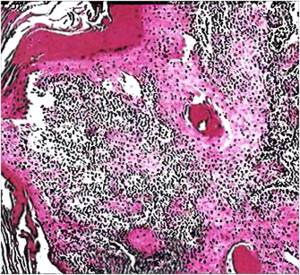
Squamous cell well-differentiated cancer
Contraindications for
An absolute contraindication to the study is pregnancy at any stage, since the dose of radiation received from an X-ray of the human trachea is significant. This type of diagnosis is not recommended for children under 15 years of age, as well as for patients in serious condition. X-ray of the trachea with contrast is contraindicated in those who have an allergic reaction to iodine or other contrast agent.
Advantages and disadvantages of the procedure
Fluoroscopy allows you to see the functioning of an organ in real time, but in this case you have to rely entirely on the qualifications of the doctor performing the procedure. The radiation dose during fluoroscopy is higher due to the fact that the patient has to remain under the sight of the x-ray machine for a long time. The main advantage of tracheal radiography is its low cost compared to other research methods, as well as its efficiency: in fact, the trachea is photographed, and it only takes a few seconds.
However, we should not forget that an X-ray of the trachea does not show so much that it should be done without a doctor’s recommendation. This is one of the diagnostic methods with a relatively high level of radiation exposure. For these reasons, it is not applicable to pregnant women and children. The low information content of the standard examination makes it less and less popular compared to CT. Therefore, if problems are detected, the doctor usually prescribes an additional examination of the trachea using a more modern diagnostic method.
Treatment methods
The treatment method is selected taking into account many factors: stage, location of the tumor, form of its growth, extent of the process, degree of malignancy. The most important preliminary study is a biopsy followed by histology, which determines the type of malignant tissue. CT and fibrolaryngoscopy have demonstrated high effectiveness in diagnosing lesions of the cartilage of the larynx and periglottic spaces. So, if these structures are affected, surgical intervention is necessarily included in the complex of therapy.
Basic techniques:
- operation;
- radiation therapy;
- chemotherapy;
- a combination of the above methods.
Surgical intervention
The following types of operations are carried out:
- CO2 laser resections;
- Laryngectomy;
- Partial resection of the larynx
- Cervical lymph node dissection
- Reconstructive plastic surgery
The scope of the surgeon's work is determined by the location of the tumor, its extent and radiosensitivity.

Types of surgical interventions:
- Chordectomy. Represents the removal of one vocal cord. Indications for it: damage to only one vocal cord without spreading the process to the vocal process of the arytenoid cartilage and commissure, no immobilization of the vocal fold.
- Hemilaryngectomy – resection of half the larynx.
- Anterolateral (or diagonal) resection of the larynx – 2/3 of half of the larynx remains. Indications: tumor damage to half of the larynx and passage through the anterior commissure.
- Anterior (or frontal) resection of the larynx. Excision of the anterior commissure and areas of the vocal cords located in close proximity is performed.
- Horizontal resection of the larynx. The affected part is excised and the vocal folds can be preserved. It is carried out when the tumor is located in the vestibule.
- Krail's operation. The internal jugular vein is removed along with tissue and lymph nodes.
- Fascial-sheath excision of lymph nodes and tissue of the neck
- Laryngectomy along with the root of the tongue and hyoid bone.
The Krail operation and FFI of lymph nodes and neck tissue (fascial-case excision of lymphatic and neck tissue) according to indications is carried out if there is insufficient regression of enlarged lymph nodes and the possibility of their operation after irradiation of 40 Gy, as well as during the first stage of treatment
The presence of N1 and N2a mobile lymph nodes in the absence of involvement of the sternocleidomastoid muscle and jugular vein in the pathological process serves as an indication for fascial-case lymph node dissection.
If there are N1, N2a, b, c impacted, immobile lymph nodes, and the sternocleidomastoid muscle and internal jugular vein are also involved in the process, a Crail operation is performed.
If a regional metastasis in the neck is fused with vessels, the patient is additionally prescribed angiography and CT scan of the neck, because in this case it is possible to perform a Crail operation with removal of the artery and its plastic replacement.
If a patient has single metastases in the liver and lungs, further examination is necessary to decide on further tactics for managing this patient
Radiation therapy
Indications are neoplasms in the middle and vestibular parts of the larynx.
Irradiation can be carried out as preparation for surgery (40-45 Gy mode), as well as radically in a therapeutic mode (70 Gy).
According to foreign and domestic authors, with stage I-II laryngeal cancer, 70-80% of patients can be cured using a 70 Gy regimen, as well as 45-52% of patients with stage III.
Contraindications to irradiation at the first stage:
- chondroperichondritis of the larynx;
- laryngeal stenosis (severe);
- tumor damage to surrounding organs (trachea, esophagus), as well as its disintegration;
- distant metastases;
- immobile conglomerates of metastases with ingrowth into great vessels;
- damage to the subglottic region;
- general serious condition of the patient due to diabetes, progressive tuberculosis, and cardiovascular diseases.

If after irradiation of 40 Gy the effect is insufficient and the patient categorically refuses surgery, radiation therapy is continued until the therapeutic dose (70 Gy).
When the tumor has spread to the anterior commissure, preepiglottic space, or lateral pharyngeal wall, radiation is ineffective as the only treatment. It is supplemented with chemotherapy, microwave hyperthermia and/or surgery.
Often, before treatment, if necessary, the patient is given a tracheostomy due to the high risk of suffocation during treatment. During radiation therapy or chemotherapy due to edema, an irreversible condition may occur that can lead to the death of the patient, without prior tracheostomy. There is also a need to install a gastrostomy tube, which can be performed under endoscopic control and in the classical open way.
If the patient has a tracheostomy, nasogastric tube or gastrostomy tube, this is not an obstacle to radiation or chemotherapy. If the neoplasms are widespread, the tracheostomy may fall into the radiation field.
Chemotherapy
Options for using systemic chemotherapy:
- palliative treatment for metastases and recurrent disease;
- in combination with radiation – organ-preserving treatment of locally advanced tumors;
- neoadjuvant therapy – makes it possible to perform surgery and/or reduce the amount of intervention;
- if the patient refuses surgery or the impossibility of surgical intervention, for example, with intolerance to anesthesia, in old age, with somatic diseases.
Main drugs used: 5 Fluorouracil, Cisplatin, Carboplatin, Paclitaxel
Contraindications to chemotherapy:
- perichondritis;
- laryngeal stenosis 2-3 degrees;
- tumor damage to the arytenoid and thyroid cartilages;
- stomach and duodenal ulcers;
- diseases of the kidneys, liver, cardiovascular system in the stage of decompensation;
- decompensated diabetes mellitus;
- pregnancy;
- open form of pulmonary tuberculosis.
X-ray examination of tracheal diseases
X-ray of the trachea is an effective and affordable way to detect various diseases. X-ray examination of the trachea can be overview or targeted. Sighting differs from survey in that it uses special equipment for a detailed examination of a separate organ. For better visualization, x-rays are taken in frontal and lateral projections. At the moment, X-rays of the respiratory organs with contrast have almost been replaced by computed tomography, but due to their availability, contrast X-rays continue to be in demand.
Special instructions for treatment
According to research, if the supraglottic region is affected and the process extends to stage T1N0M0, it is better to give preference to irradiation (the cure rate reaches 95%, the function of the larynx is preserved). For T2N0M0 and similar localizations, organ-sparing surgery is indicated, because up to 80% of relapses after irradiation are associated with damage to these particular laryngeal structures.
If the folded area is affected and stage T1N0M0 is recorded, therapy begins with irradiation. With this method, the cure rate is 75-78%, taking into account which it is necessary to carry out an initial assessment of the effectiveness of therapy at a dose of 40 Gy. If regression of the tumor is less than 70%, then surgical intervention – chordectomy – is possible. When the tumor has spread to the anterior commissure and second vocal fold, laryngeal resection is performed, because in this case the long-term results are better than with radiation.
Chemotherapy does not improve treatment outcomes for stage T1-2N0M0.
When treating locally advanced pathology at stage T3N0M0-T4N0M0, the greatest effectiveness was shown by the use of a combined technique with different sequences of irradiation and surgery, because in this case, 70-73% of patients achieve five-year survival. However, this involves performing a laryngectomy, which disables the patient.
If the patient has contraindications to surgery, therapy begins with radiation. If the cancer is advanced T3-T4, then the options for radiation therapy are limited. Moreover, even if operations are possible, they are crippling in nature. An option for organ-preserving treatment of locally advanced pathology or the hypopharynx may be a combination of induction chemotherapy according to the PF regimen (Cisplatin and 5-fluorouracil) with further irradiation if there is a response to therapy. If it is not observed, a laryngectomy is performed.
How is the examination carried out?

X-rays of the trachea are performed in x-ray diagnostic rooms. To examine your throat, you will need to lie on your side and apply a special film to your neck. This is usually done by a doctor, fixing the patient in a position that allows good pictures to be taken. During the examination, the patient is asked to hold his breath. After a few seconds, the patient can get up and, taking the developed image, go home.
X-ray of the trachea with contrast
In order to ensure better visibility of the organ in the image, a contrast agent is injected into its lumen, which blocks x-rays. For X-rays of the trachea, you will need to drink a contrast agent based on barium or iodine sulfate. After some time, you can begin the examination in the usual way.
X-ray of the trachea with functional tests
An X-ray of the trachea with functional tests takes a little longer than a regular one, since it is aimed at obtaining images from different angles, with different conditions of the organ. The patient ensures the necessary condition of the organ by following the doctor’s instructions. During fluoroscopy of the trachea with contrast of the esophagus, a radiologist
will ask the patient to breathe and hold his breath, comparing the state of the organ at rest and during functioning. X-ray of the trachea with functional tests allows you to determine the state of the organ when performing its direct functions, which greatly simplifies diagnosis.
Treatment of metastases in the lymph nodes of the neck
Regional metastases in laryngeal cancer do not interfere with conservative therapy, because neoplasms of this localization (N1-N2) are often amenable to chemotherapy and radiation. Therefore, the lymph nodes on both sides must be included in the irradiation zone of the larynx. If it is necessary to irradiate the lymph nodes of the lower parts of the neck, the use of a direct field with a block is indicated. The lower edge of this field extends 1 cm below the lower border of the clavicle. In case of damage to the supraclavicular lymph nodes, it is necessary to irradiate the lymph nodes of the upper mediastinum.
When non-displaceable or limited displacement metastases are present, it is advisable to begin treatment with neoadjuvant polychemotherapy followed by 40 Gy of radiation. Further, the tactics are determined by the effectiveness of the treatment. If significant or complete regression of metastases is observed, as well as their inoperability after a dose of 40 Gy, then irradiation is adjusted to 60-70 Gy.
It is worth especially noting that today, when the indicator of quality of life is as important as the reliability of oncological treatment, specialists are directing their efforts to the development and improvement of conservative therapy, including various types of chemotherapy and radiation, as well as to performing organ-saving operations that allow preserving or restoring the main functions of the larynx.
How much does a laryngeal x-ray cost?
The cost of the examination depends on the location - a private diagnostic center or a public clinic. The price is also affected by the equipment used for the study - classic X-ray or digital. On average, the cost varies from 1000 to 1900 rubles.
The attending physician, usually an otolaryngologist, can refer you for an X-ray examination. You should not decide on your own about the need for the procedure; after all, diagnosis requires a certain dose of radiation.
X-ray of the larynx is an accessible method for identifying pathology of the respiratory tract, however, it is not the most informative. In some cases, an additional CT or MRI may be necessary.
Survival prognosis
The prognosis depends on the stage of the disease, but in general it is unfavorable. This is largely due to the large proportion of patients with advanced forms of cancer.
According to clinical observations and literature data, advanced forms of laryngopharyngeal oncology account for more than 85% of all newly diagnosed cases of morbidity.
Using modern methods of complex therapy, 56% of patients achieve five-year survival.
The prognosis becomes worse in the presence of metastases: for cancer of the hypopharynx T3-4N0-1M0, the three-year survival rate is up to 80%, and for stage T3-4N2-3M0 – up to 40%.
If, as a result of chemotherapy and radiation, complete regression of the disease is achieved, you need to be regularly observed and examined so that in case of relapse, surgery can be performed in a timely manner.
Table of survival rates, depending on the form of pathology and its stage
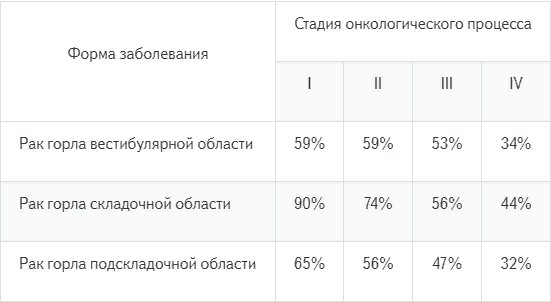
For patients with stages III-IVb, the five-year survival rate is 48.2%, for HPV+ and HPV- (RR=0.73, p<0.001) – 42.1%.
Rehabilitation
Speech therapy rehabilitation methods are widely used, aimed at restoring vocal function and achieving good voice quality. It is possible to achieve the set goals in 45-60% of cases.
After laryngectomy:
The voice is a socially important function that does not need proof, so it is quite reasonable for patients to strive to preserve or restore it. For those who have had a laryngectomy, vocal rehabilitation is carried out through training in the so-called esophageal voice, the use of voice devices, or the installation of a tracheoesophageal shunt of the Bloom-Singer type.
One of the methods for voice rehabilitation in patients who have undergone complete resection of the larynx is the use of voice-forming devices of various designs. These can be electric larynxes, sound generators.
According to many authors, the method of teaching esophageal speech is the most physiological and minimally invasive. In 62-91% of cases it is possible to form a pseudo-voice, which will be sufficient for communication.
Disadvantages of the method:
- patients find it difficult to master the method of swallowing air masses into the esophagus and pushing it out during phonation;
- the esophagus as a reservoir for air has a small volume - 180-200 ml;
- spasm and hypertonicity of the compressive elements of the pharynx.
Surgical technique for voice restoration after laryngectomy
The method is based on the formation of a shunt between the esophagus and trachea. Through it, air from the lungs enters the pharynx and esophagus, provoking vibration of the pharyngoesophageal element, which is the voice generator.
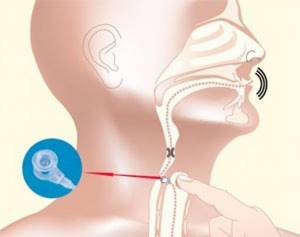
A voice prosthesis placed in the lumen of the shunt allows air from the lungs into the esophagus and prevents food and liquid from entering in the opposite direction.
Good voice quality, thanks to this technique, was achieved in 93.3% of patients. However, the authors of the method indicate that in 7-30% of cases complications are possible: fungal infection of the prosthesis, excessive growth of granulations, displacement of the prosthesis, leakage of the prosthesis, which can lead to aspiration pneumonia in patients.
Studies show that all patients after organ-preserving operations experience impaired swallowing function, because the entire mechanism is rebuilt in accordance with the type of intervention. Violations of the protective function are more significant after horizontal and sagittal resection of the larynx. To prevent aspiration of food and saliva in the postoperative period, various methods of obturation (blockage) of the larynx are used: starting with Mikulicz tamponade (indicated during sagittal surgery) and ending with the use of obturators and T-shaped silicone tubes with a closed upper end, inserted into the formed respiratory anastomosis . These measures are aimed at preventing food from entering the respiratory tract.
Chronic aspiration of saliva often leads to pneumonia, so corrective surgery is indicated in some cases. Solving this problem affects the patient's future life, because constant aspiration may cause the need for laryngectomy.
One of the most difficult tasks when performing organ-saving operations is restoring respiratory function, because all types of resection, with the exception of extirpation of the epiglottis, deform the larynx and reduce its size. V. O. Olshansky gives a relatively higher figure - he is able to decannulate 73.4% of patients. The author used a tube-shaped endoprosthesis consisting of biologically compatible polymer materials impregnated with an antiseptic composition to restore the lumen of the larynx.