Ultrasound examination of the shoulder is a fast, relatively cheap and dynamic way to examine the shoulder joint, which is especially informative in diagnosing the condition of soft tissue structures (muscles, ligaments), the cartilaginous component and assessing the degree of impairment of motor function.
No preliminary preparation is required for ultrasound scanning of the shoulder joint and surrounding areas.
The examination requires attention to technique and appropriate positioning of the patient. A polypositional dynamic study of the joint is performed in four projections. Moreover, in each projection, the joint and all its structures are examined in two mutually perpendicular section planes (longitudinal and transverse). In case of limited joint mobility (trauma, pain), the shoulder joint can be successfully comprehensively assessed by moving the ultrasound probe.
To provide sufficient anatomical resolution, a high-frequency linear transducer (5.5-12 MHz) is required.
Shoulder joint
The shoulder joint is the most mobile joint in the body. This mobility provides the upper limb with a huge range of motion: around the sagittal axis - abduction to the horizontal level (further movement is prevented by the coracoacromial ligament, called the humeral vault) and adduction; around the frontal axis - flexion and extension; around the vertical axis - rotation of the shoulder inward and outward. When moving from one axis to another, a circular motion (circumductio) is possible in the joint.
This wide range of motion also makes the shoulder joint unstable. This instability is compensated by the rotator cuff muscles, tendons, ligaments and labrum glenoidale.
The muscles and ligaments surrounding and strengthening the shoulder joint are subject to the greatest load. The muscular, tendon-ligamentous apparatus holds the humerus in the correct position in accordance with the glenoid cavity of the scapula and allows the entire complex range of movements of the upper limb to be performed.
Content:
- Shoulder joint
- The essence of the method
- Research technique
- Indications for ultrasound of the shoulder joint
- What can be determined using an ultrasound of the shoulder joint?
- Limitations of using the method
- What happens during the study?
- Advantages of the ultrasound diagnostic method of the shoulder joint
Indications
The list of diseases for which it would be useful to do this type of ultrasound is very extensive, although diseases of the veins and arteries of the upper extremities are much less common than vascular lesions of the coronary arteries, cerebral vessels and lower extremities. The main indications for the examination will be:
- Pain or tenderness in the shoulder or forearm and hardening of the veins.
- The appearance of swelling in the hands and soreness in the muscles.
- Convulsive movements (convulsions), numbness, decreased sensitivity of the fingers.
- Cold hands.
- Diabetes.
- Trophic ulcers.
- Increased cholesterol.
- Blood failure.
- Operations of the upper extremities.
The essence of the method
The ultrasound technique is based on sound waves emitted from a transducer, which are then returned back from underlying structures based on the density of that structure. The computer interprets the returning sound waves and creates images that reflect the quality and density of the tissue from which the waves return. When the sound waves are bounced back quickly and with great force, like hitting a bone, an intensely white image (“hyperechoic”) appears on the screen. When sound waves encounter a substance that transmits the waves easily and they do not return like air or liquid, a dark image (“hypoechoic”) is displayed on the screen.
Research technique
Of course, there are an endless variety of potential techniques, but there are basic shoulder ultrasound techniques that all physicians should adhere to. In most cases, for the most complete assessment of the condition of the shoulder joint, patients are examined in several positions: lying on their back (the examined arm is located along the body), sitting with the arm bent at the elbow joint, sitting with the arm hanging freely, sitting with the arm brought to the body with an additional inner or external rotation.
During ultrasound examination, tendons cause an optical phenomenon known as “anisotropy” (i.e., the visualization of the tendon structure is directly dependent on the angle of incidence of the ultrasound beam). Therefore, each tendon must be scanned in several projections and each has its own technique.
To make a correct diagnosis, visualization of the various sections and structures of the shoulder along its length and diameter is important. Ultrasounds of the left and right shoulder joints are performed similarly to each other.
The use of a high resolution transducer (7-15MHZ) is essential when assessing the superficial structures of the shoulder joint.
Biceps tendon

Patient position: arm in neutral position, elbow flexed 90 degrees, forearm supported (palm up). The long head of the biceps tendon is visible in the intertubercular groove. It passes under the transverse humeral ligament and is visible in both transverse and longitudinal sections.
Normal findings: The tendon should be located in the bony groove with minimal fluid around it (the tendon sheath communicates with the shoulder joint), and the tendon fibers should be seen without tears, irregularities, or thickening.
Visualized pathology of the biceps tendon: biceps tendon dislocation, or subluxation, tendinopathy, shoulder effusion, partial or complete biceps rupture.
Muscles that make up the rotator cuff
The rotator cuff is a layer of muscle that surrounds the head of the humerus and includes the subscapularis, supraspinatus, infraspinatus, and teres minor muscles.
Subscapularis tendon
Patient position: The arm is held in the same position as above and rotated outward. The subscapularis tendon is stretched. Image planes: tendon m. subscapularis should be traced both longitudinally and transversely. After the longitudinal study, the transducer is placed in a transverse position (medially) over the head of the humerus with the transducer marker pointing away from the patient's torso. The probe is then moved from top to bottom to access the three parts of the tendon, that is, the upper, middle and lower fibers. Dynamic examination: During internal and external rotation of the arm, while the transducer remains stationary, possible damage to the tendon as it passes under the cocooid process can be assessed. Transverse images: By rotating the transducer 90 degrees (now in the craniocaudal direction) toward the patient's head, the short axis of the three parts of the tendon can be assessed.
The transducer is slowly raised medially toward the lesser tuberosity of the humerus.
Visualized pathology: supraspinal tendinopathy, dynamic subluxation of the long head of the biceps tendon, damage to the transverse ligament.
Supraspinatus tendon
Patient position: internal rotation and extension of the shoulder. The supraspinatus tendons should be traced both longitudinally and transversely. Most ruptures occur in the most distal portion and therefore this area should be explored with caution.
Normal Findings: The tendon parallels the curved contour of the humeral head and flattens as it contacts the greater tuberosity of the humerus. The tendon has a fibrillar pattern. The subacromial bursa should be considered as one thin hyperechoic line parallel to the tendon; the presence of fluid (bleeding of the hyperechoic line by hypoechoic fluid) is abnormal, as is thickening of the bursa.
Visualized pathology: supraspinal tendinopathy, subacromial bursitis.
Infraspinatus tendon
Image Planes: The infraspinatus tendon should be traced both longitudinally and transversely. Normal results: The separation of the infraspinatus tendon from the supraspinatus tendon is so difficult that a random cut is used at a distance of 1.5 cm from the anterior edge of the supraspinatus tendon; i.e., the first 1.5 cm of the rotator cuff is designated the supraspinatus tendon and the next 1.5 cm is the infraspinatus tendon. The thickness of the posterior rotator cuff is significantly less than the anterior rotator cuff (3.6 vs. 6 mm), and therefore thinning should not be interpreted as partial tears.
Visualized pathology: tendinopathy, complete or partial tears.
What will an ultrasound of the vessels of the upper extremities show?
The use of color Doppler ultrasound technology makes it possible to detect blood clots and dissection of vessel walls, and to determine the formation of atherosclerotic plaques. Stenosis . Carrying out an ultrasound scan of the arteries and veins of the upper extremities gives doctors the opportunity to diagnose narrowing of the lumen of blood vessels in the early stages. The presence of compactions and irregularities on the walls is a symptom of stenosis. But establishing only the fact of narrowing is not enough. The main thing is to determine the degree of criticality of the disease. Ultrasound screening data allows you to measure the level of the vessel lumen and stage the stenosis. This information is fundamental in deciding whether surgical intervention is necessary. A level of stenosis of 70% or higher is considered critical. Often, if a sufficiently strong narrowing in the upper extremities is detected, it is recommended to undergo an MRI of the main arteries of the head, especially if the patient suffers from headaches. Thrombosis . The presence of a blood clot in the lumen of a vein or artery is the main cause of blockage of blood vessels, which leads to impaired blood flow. Ultrasound examination techniques allow not only to find the exact location of the blood clot, but also to determine its structure and size and even determine the causes of blood clots. Problems with blood flow speed. Vascular ultrasound is one of the most effective methods for diagnosing blood flow speed. When scanning an area where blood flow is blocked, a sharp, high-pitched sound is produced and a sharp drop in the speed of blood flow is observed. Normal blood flow is characterized by a decrease in linear velocity in the direction from the proximal to the distal segments of the upper extremities and high peripheral vascular resistance. During an ultrasound scan, the doctor makes a comparative analysis of blood flow readings that were obtained at rest and under load. In the absence of pathologies, they should differ by at least 10-40%. If significant anomalies are detected, additional examinations may be ordered. Most likely, the patient will be offered to undergo an ultrasound of the lower extremities so that the diagnosis of the vascular system is complete.
| Service | price, rub. | Promotion Price |
| “Healthy Legs” program (duplex scanning of the veins of the lower extremities with assessment of valves and perforating veins and duplex scanning of the arteries of the lower extremities) | 3200 rub. | 3000 rub. |
| Ultrasound triplex scanning of N/C veins with assessment of valves and perforating veins | 2500 rub. | |
| Ultrasound triplex scanning of veins of the upper extremities | 2000 rub. | |
| Ultrasound triplex scanning of the arteries of the lower extremities with measurement of the brachiomalleolar index (BMI) | 2000 rub. | |
| Ultrasound triplex scanning of the arteries of the upper extremities | 2000 rub. | |
| Ultrasound duplex scanning of the arteries of the aorto-iliac segment | 1900 rub. | |
| Ultrasound duplex scanning of the abdominal aorta and visceral arteries | 1900 rub. | |
| Ultrasound duplex scanning of the inferior vena cava | 1700 rub. | |
| Ultrasound duplex scanning of the iliac vein | 1700 rub. | |
| Ultrasound duplex scanning of the renal arteries | 1700 rub. | |
| Intracranial duplex of cerebral vessels | 2500 rub. | |
| Ultrasound of neck veins | 2500 rub. | |
| Ultrasound of the brachiocerebral arteries (BCA) | 2500 rub. | |
| Heart ultrasound or echocardiography for adults | 2400 rub. | |
| Comprehensive neck diagnostics (MRI of the cervical spine, MRI of neck vessels, ultrasound examination of neck vessels, ultrasound of the thyroid gland and soft tissues of the neck, consultation with a neurologist) | 13200 rub. | 9500 rub. |
Indications for ultrasound of the shoulder joint

Ultrasound is a valuable diagnostic tool for evaluating the following indications:
- muscle, tendon and ligament damage (chronic and acute);
- bursitis;
- effusion;
- vascular pathology;
- hematomas;
- soft tissue formations such as lipomas;
- to assess the structure of the formation, for example: dense, cystic, mixed;
- postoperative complications, such as abscess;
- for monitoring during injection, aspiration or biopsy;
- some bone pathologies.
What can be determined using an ultrasound of the shoulder joint?
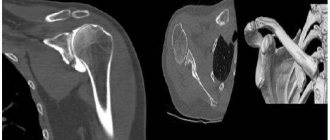
Using an ultrasound examination of the shoulder joint, the development of the following pathological processes can be determined:
- traumatic or degenerative damage to the muscle complex that ensures mobility of the shoulder joint - the rotator cuff;
- fractures or cracks of the humerus;
- tenosovinitis or bursitis - various inflammatory diseases of the joint;
- injuries or displacement of the humeral process of the scapula;
- rupture of the articular labrum - the cartilage tissue surrounding the socket of the joint;
- excess or insufficient amount of fluid in the joint cavity;
- connective tissue damage - arthritis;
- muscle atrophy - a decrease in the number of muscles and a decrease in their functionality;
- synovial cyst - a benign formation that on ultrasound looks like a small darkened area with uneven contours;
- osteoarthritis is a disease during which the cartilage tissue of the joint becomes thinner and loses functionality (usually accompanied by pain and limited mobility);
- inflammation of the synovial bursa.
What happens during the study?
Before the diagnosis begins, the patient is asked to sit or lie on a special couch. A small amount of a special gel is applied to the skin to improve contact between the sensor and tissue. During the diagnosis, the doctor evaluates the condition of the muscles, tendons and nearby tissues. To assess the dynamic state of the joint, the patient is asked to change the position of the arm as needed: lift, abduct, and unfold. Typically, the duration of the study is about half an hour, and upon completion, the patient is given a protocol with a transcript.
Ultrasound examination of the shoulder joint is comparable in accuracy to MRI. It can be used as a targeted examination, providing rapid, real-time diagnosis and treatment in required clinical situations.
Preparation for ultrasound of the upper extremities
Ultrasound of the arteries and veins of the upper extremities is a non-surgical method for examining the vascular system and does not require special training. It is not recommended to do it on an empty stomach; the patient needs to eat something light shortly before the procedure. The day before the examination, you should avoid strenuous physical activity. It's also important to get a good night's sleep. The day before the ultrasound procedure, it is advisable to avoid foods that can affect the condition of blood vessels, for example, energy drinks, caffeine (coffee, tea).