Increased values (lactic acidosis)
- Pathologies of the cardiovascular system: heart failure, cardiogenic shock (acute left ventricular failure), Raynaud's syndrome (severe vascular disease, spasm of small blood vessels);
- Blood flow disorders and diseases of the circulatory system;
- Non-insulin-dependent diabetes mellitus;
- Increased physical activity (usually among professional athletes);
- Tetany (convulsions due to calcium metabolism disorders);
- Tetanus (a bacterial disease affecting the nervous system);
- Epilepsy (pathology of the nervous system, manifested by convulsive seizures with loss of consciousness);
- Hepatitis (viral inflammation of the liver) in acute form;
- Cirrhosis of the liver (an abnormal change in the structure of the organ tissue);
- Oncological processes: lymphoma (cancer of the lymphatic system), leukemia (blood cancer), etc.;
- Poliomyelitis (highly contagious disease of the nervous system, spinal paralysis);
- Tissue hypoxia (oxygen starvation);
- Hypotension (low blood pressure);
- Heavy bleeding;
- Pulmonary insufficiency, hyperventilation (impaired frequency or depth of breathing).
A temporary increase in lactic acid concentration is possible as a result of:
- deficiency of vitamin B1 in the body;
- long-term regular use of alcohol;
- poisoning with chemical elements: ethanol, salicylates, toxins, methanol, etc.;
- dehydration (dehydration of the body);
- pregnancy (in the 3rd trimester the level of lactic acid may increase slightly);
- taking medications: sodium drug, nitroprusside, adrenaline, metformin, fructose or glucose, propylene glycol, methylprednisolone, phenformin, etc.
POLYTRAUMA / POLYTRAUMA
Ustyantseva I.M.1,2, Khokhlova O.I.1, Agadzhanyan V.V.1,2
1 State Autonomous Institution "Regional Clinical Center for Miners' Health", Leninsk-Kuznetsky, Russia, 2 Federal State Budgetary Institution "Novosibirsk Research Institute of Traumatology and Orthopedics named after. Ya.L. Tsivyana" of the Ministry of Health of Russia, Novosibirsk, Russia
BLOOD LACTATE LEVEL AS A PREDICTIVE FACTOR OF MORTALITY IN PATIENTS WITH POLYTRAUMA
Purpose of the study -
to evaluate the clinical and prognostic significance of blood lactate level as a predictor of mortality in polytrauma.
Material and methods.
The study is based on a retrospective analysis of medical records of 475 patients with polytrauma.
We analyzed demographic data (age, gender), mechanism of injury, information on vital signs during hospitalization (heart rate (HR), systolic blood pressure (SBP)) and rating scales (Glasgow Coma Scale (GCS), Injury Severity Score ISS (Injury Severity Score), Abbreviated Injury Scale (AIS)). Discharge status (whether the patient survived or not) was also taken into account. The group of survivors consisted of 439 victims, 36 who died. The lactate content in whole venous blood was determined in the first three hours after admission to the hospital using a Roche Omni S critical care analyzer (Germany). Results.
As a result of multiple logistic regression analysis, it was found that the most significant prognostic factors for mortality in patients with polytrauma were the level of lactate in the blood, hypertension and hypotension, and severity of injury according to the ISS scale.
After adjusting for SBP, HR, and ISS, baseline lactate remained independently associated with increased mortality (adjusted odds ratio 1.0 (95% CI 0.1–1.1), 1.5 (95% CI 1.1–2. 0) and 3.8 (95% CI 2.8–5.3) for lactate levels <2.5, 2.5–3.9, and ≥4 mmol/L, respectively). It was also revealed that in victims with hypotension (SBP < 90 mmHg), mortality increased as the severity of hypotension progressed and the level of lactate in the blood increased. Conclusion.
The level of lactate in whole blood in the first three hours after injury is an independent predictor of mortality in polytrauma. Victims with lactatemia levels above 2.5 mmol/l require careful examination and monitoring.
Keywords:
polytrauma; mortality; lactate
Lactate is a metabolite, the level of which in the blood depends on the balance of the intensity of the processes of its formation and utilization, and, accordingly, an increase in its content in the blood can be associated with both increased production and reduced consumption [1]. The main reason for the excessive formation of lactate is increased anaerobic processes in tissues with insufficient oxygen supply. Therefore, determination of lactate in the blood is useful in the diagnosis and prediction of tissue hypoxia, for example, in shock [2]. Assessment of the level of lactatemia is recommended as one of the most proven indicators for assessing the degree of blood loss [3]. Elevated blood lactate levels have been shown to be associated with increased mortality in trauma patients and predict the need for massive blood transfusions [4–6]. Blood lactate testing in combination with systolic blood pressure (SBP) may improve the ability to predict adverse outcomes in severe injuries [7, 8]. In the international criteria for sepsis SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference revision 2001 [9], Surviving Sepsis Campaign (SSC12) 2012 [10] and “Sepsis-3” 2016 [11] increased lactate levels ( above the laboratory norm > 1 mmol/L) is proposed as an indicator of tissue hypoperfusion. Lactate clearance is associated with favorable outcomes in critically ill patients, including those with septic shock [12, 13]. At the same time, small groups of trauma patients have shown that a long-term increase in blood lactate levels is accompanied by an increased risk of infection and complications [14, 15]. We have previously shown the possibility of using blood lactate in patients with polytrauma to assess the severity of the systemic inflammatory response syndrome and predict septic complications [16-18]. Despite the fact that a large number of studies have been devoted to the study of blood lactate, and its monitoring is widely used in clinical practice, the diagnostic value of this metabolite in critically ill patients has not been fully determined [10, 13, 15]. The significance of blood lactate level as a prognostic factor for mortality in a cohort of patients with polytrauma has also been insufficiently assessed.
Purpose of the study
– to evaluate the clinical and prognostic significance of blood lactate level as a predictor of mortality in polytrauma.
MATERIAL AND METHODS
The retrospective analysis covered the period from January 1, 2003 to January 1, 2013 and included 475 patients with polytrauma delivered to the Regional Clinical Center for Miners' Health within 2 hours from the moment of injury. Of these, 29.7% are women, 70.3% are men. The average age of the victims was 42.2 ± 2.23 years. Inclusion criteria: age 18 years or older, presence of severe multiple or combined injuries. To conduct the study, permission was obtained from the Ethics Committee of the State Autonomous Institution of Healthcare of the Okrug. We analyzed demographic data (age, gender), mechanism of injury, information on vital signs during hospitalization (heart rate (HR), systolic blood pressure (SBP)) and rating scales (Glasgow Coma Scale (GCS), Injury Severity Score ISS (Injury Severity Score), Abbreviated Injury Scale (AIS)). Discharge status (whether the patient survived or not) was also taken into account. The group of survivors included 439 victims, 36 died. Early death was considered to be within 48 hours after hospitalization, late death was considered to be after 48 hours. The causes of deaths have been determined. The most common cause of death in victims in the early period after injury was bleeding (noted in 66% of cases). Among the causes of late death, head trauma (39.1%) and multiple organ failure (47.1%) predominated. The lactate content in whole venous blood was determined in the first three hours after admission to the hospital using a Roche Omni S critical care analyzer (Germany); the results were obtained electronically from the hospital laboratory information system. Lactate levels < 2.5 mmol/L were considered low, 2.5–3.9 mmol/L moderately high, and ≥ 4 mmol/L significantly high. Statistical processing of the results obtained
was carried out using the IBM SPSS Statistics 20 program. To check the nature of the distribution of the obtained quantitative indicators, the Kolmogorov-Smirnov test was used. Since the distribution of most of the data corresponded to the law of normal distribution, quantitative variables are presented as M (SD) (M is the arithmetic mean, SD is the standard deviation). Categorical data were described as absolute values (n) with proportions (%). Differences between groups in quantitative variables were identified using the parametric Student's t test. Between-group comparisons of categorical data were made based on sample size using the χ2 test of proportions or Fisher's exact test. Differences were considered statistically significant at p < 0.05. To identify prognostic factors for mortality in patients with polytrauma and to assess the independent relationship between lactate and mortality, multiple logistic regression analysis was performed. A stepwise forward search procedure was used. Results are presented as odds ratios (OR) and 95% confidence intervals (95% CI).
RESULTS
The characteristics of the groups of patients with polytrauma upon admission to the hospital are presented in Table 1. The groups, on average, did not differ in the mechanism of injury. Thus, the most common cause of injury in both groups of victims was a road traffic accident. However, statistically significant differences were noted in the nature and severity of injuries. Almost twice as often (p < 0.0001), the severity of injury in patients with a fatal outcome, compared with the group of survivors, was assessed as severe and extremely severe (ISS score exceeded 15 points) (Table 1). At the same time, the differences were due mainly to the severity of injuries to the head, chest and abdomen, while there were no differences between the groups in the nature of superficial injuries and injuries to the extremities. The level of consciousness assessed on the Glasgow Coma Scale in deceased patients was almost 1.7 times lower than in surviving patients (p < 0.001).
Table 1. Characteristics of cohorts of patients with polytrauma
| Index | Survivors | Dead | p |
| n, abs. | 439 | 36 | |
| Age, avg. meaning (SD) | 48.2 (22.1) | 67.9 (21.1) | < 0.0001 |
| Men, n (%) | 297 (68) | 21 (62) | n/a |
| Mechanism of injury, n (%): | |||
| — Road accident | 210 (48) | 15 (42) | n/a |
| - falls | 87 (20.2) | 9 (25.8) | n/a |
| - injuries | 44 (10.2) | 2 (5.6) | n/a |
| - another | 98 (21.6) | 10 (26.6) | n/a |
| Glasgow Coma Scale Score, avg. meaning (SD) | 13.8 (3.2) | 7.8 (5.2) | < 0.001 |
| ISS indicators: | |||
| < 15, n (%) | 280 (63.8) | 11 (30.3) | < 0.001 |
| 15-25, n (%) | 104 (23.7) | 10 (28.0) | n/a |
| > 25, n (%) | 55 (12.5) | 15 (41.7) | < 0.001 |
| Nature of damage according to AIS* avg. value (SD): | |||
| - head | 3.4 (1.1) | 4.7 (0.75) | < 0.001 |
| - rib cage | 3.0 (1.03) | 3.6 (0.89) | < 0.001 |
| - belly | 2.7 (0.95) | 3.3 (1.1) | < 0.001 |
| - limbs | 2.7 (0.67) | 2.8 (0.8) | 0.06 |
| - superficial damage | 1.0 (0.26) | 1.1 (0.24) | 0.96 |
| Heart rate, beats/min., avg. meaning (SD) | 89.8 (18.9) | 85.6 (25.9) | < 0.001 |
| SBP mm. rt. Art., Wednesday meaning (SD) | 136.2 (27.3) | 130.3 (42.5) | < 0.001 |
| Lactate, mmol/l, avg. meaning (SD) | 2.5 (1.8) | 3.8 (3.0) | < 0.001 |
Note:
* AIS – Abbreviated Injury Scale; n/a – no reliability.
Statistically significant differences between the groups were also noted in age (patients who died were 1.4 times older than those who survived), heart rate, SBP, and mean blood lactate (which was 1.5 times higher in the cohort of deceased patients than in group of survivors (p < 0.001)). Further analysis showed a connection between the mortality rate of patients with polytrauma and the level of lactate in the blood. Thus, with a blood lactate concentration <2.5 mmol/l, mortality was 5.4% (95% CI 4.5–6.2%), with lactatemia values ranging from 2.5–3.9 mmol/l mortality was 6.4% (95% CI, 5.1–7.8%), and for levels ≥ 4 mmol/L it was 18.8% (95% CI, 15.7–19.9%) (Fig. 1).
Figure 1. Relationship between blood lactate levels and mortality in patients with polytrauma
As a result of multiple logistic regression analysis, it was found that the most significant prognostic factors for mortality in patients with polytrauma were the level of lactate in the blood, hypertension and hypotension, and severity of injury according to the ISS scale (Table 2). Moreover, elevated lactate levels predicted both early and late mortality. After adjusting for SBP, HR, and ISS, baseline lactate remained independently associated with increased mortality (adjusted odds ratio 1.0 (95% CI 0.1–1.1), 1.5 (95% CI 1.1–2. 0) and 3.8 (95% CI 2.8–5.3) for lactate levels < 2.5, 2.5–3.9 and ≥ 4 mmol/l, respectively) (Table 2). It was also found that there is a U-shaped relationship between mortality rates and SBP, and the likelihood of death in victims with the highest and lowest quartiles of blood pressure is significantly higher than with normal or moderately elevated SBP.
Table 2. Prognostic factors for mortality in patients with polytrauma (n = 475) in multiple logistic regression analysis
| Odds Ratio (95% CI) | |
| Lactate, (mmol/l) | |
| 0-2.5 | 1.0 (0.1-1.1) |
| 2.5-3.9 | 1.5 (1.1-2.0) |
| ≥ 4.0 | 3.8 (2.8-5.3) |
| SBP, (mm Hg) | |
| Quartile 1 (≤ 118) | 2.3 (1.5-3.4) |
| Quartile 2 (119-134) | 1.7 (1.1-2.6) |
| Quartile 3 (135-152) | 1.0 (0.1-1.1) |
| Quartile 4 (≥ 152) | 1.8 (1.2-2.7) |
| Heart rate, (beats / min ) | |
| < 70 | 1.6 (1.1-2.2) |
| 70-199 | 1.0 (0.1-1.1) |
| ≥ 120 | 1.7 (1.0-2.7) |
| ISS, (score) | |
| < 20 | 1.0 (0.1-1.1) |
| 20-29 | 3.2 (2.4-4.3) |
| 30-39 | 3.4 (2.1-5.5) |
| ≥ 40 | 6.6 (4.0-11.0) |
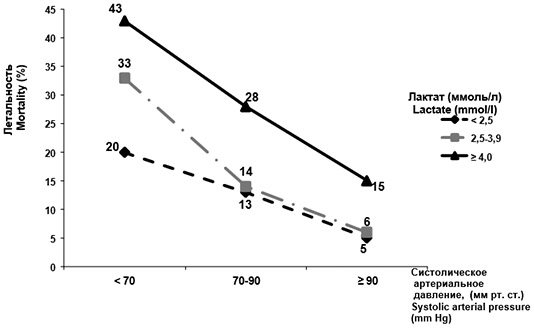
Subsequent analysis revealed an association between blood pressure, lactate, and mortality. Thus, in victims with hypotension (SBP < 90 mmHg), mortality increased as the severity of hypotension progressed and the level of lactate in the blood increased (Fig. 2).
Figure 2.
Relationship between hypotension and mortality rates based on blood lactate levels in patients
DISCUSSION
The presented study, based on a large cohort of polytrauma patients (n = 475), shows that initial blood lactate levels measured within 3 hours after injury provide additional prognostic information to traditional clinical predictors of mortality [11, 12, 15]. We found a complex relationship between systolic blood pressure, lactate and mortality in patients with hypotension (SBP < 90 mmHg). As the severity of hypotension progresses, increasing levels of lactatemia have been shown to be associated with an increased risk of death. The relationship between high SBP and mortality requires further study. The results obtained are consistent with published data from other authors, where the initial blood lactate level was closely associated with mortality in trauma patients, regardless of factors such as injury severity, age and hemodynamic parameters [19, 20]. The importance of measuring lactatemia in the first hours after injury is determined by the fact that it is the most operational indicator of hypoxia: its level in the blood increases before the appearance of other signs of oxygen deficiency (in particular, changes in blood pressure and heart rate) [1]. It has been shown that studying the dynamics of blood lactate can be used to assess the adequacy of therapy and serve as one of the prognostic criteria for the patient’s treatment outcome [3, 5]. The presented study has several important methodological limitations. In particular, this is a retrospective study, which already has some limitations. The heterogeneity of the population of patients with polytrauma (comorbidity, gender) is not sufficiently taken into account. In addition, only the initial lactate level was assessed and pre-hospital interventions (replenishment of circulating blood volume with fluids, resuscitation measures, etc.) were not taken into account. All this determines the tasks of future research.
CONCLUSIONS:
1. The level of lactate in whole blood in the first three hours after injury is an independent prognostic factor for mortality in polytrauma. 2. Victims with lactatemia levels above 2.5 mmol/l need careful examination and monitoring.
Funding and conflict of interest information:
The study had no sponsorship.
The authors declare that there are no obvious or potential conflicts of interest related to the publication of this article.
LITERATURE:
1. De Backer D. Lactic acidosis. Intensive Care Med
.
2003; 29: 699-702 2. Ustyantseva IM, Khokhlova OI. New ideas about the role of lactate in shock (literature review). Polytrauma
.
2009; 2: 70-73. Russian (Ustyantseva I.M., Khokhlova O.I. New ideas about the role of lactate in shock (literature review) // Polytrauma
. 2009. No. 2. P. 70-73) 3. Spahn DR, Gerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Gordini G, et al.
Management of bleeding following major trauma: a European guideline. Crit.
Care. 2007. 11(1): R17.
4. Callaway DW, Shapiro NJ, Donnino MW, Baker C, Rosen CL. Serum lactate and base deficit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma
.
2009; 66: 1040-1044 5. Kruse O, Grunnet N, Barfod C. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: a systematic review. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine.
2011;
19: 74 6. Vandromme MJ, Griffin RL, Weinberg JA, Rue LW 3rd, Kerby JD. Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg
.
2010; 210: 861-867, 867-869 7. Odom SR, Howell MD, Silva GS, Nielsen VM, Gupta A, Shapiro NI et al. Lactate clearance as a predictor of mortality in trauma patients. Trauma Acute Care Surg.
2013;
74 (4): 999-1004 8. Paladino L, Sinert R, Wallace D, Anderson T, Yadav K, Zehtabchi S. The utility of base deficit and arterial lactate in differentiating major from minor injury in trauma patients with normal vital signs. Resuscitation
.
2008; 77: 363–368 9. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med
.
2003; 31(4): 1250-1256 10. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med.
2013;
41(2): 580-637 11. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al. The third international consensus definitions for sepsis and septic sShock (Sepsis-3). JAMA
.
2016; 315(8): 801–810 12. Jansen TC, van Bommel J, Woodward R, Mulder PG, Bakker J. Association between blood lactate levels, sequential organ failure assessment subscores, and 28-day mortality during early and late intensive care unit stay: a retrospective observational study. Crit.
Care Med .
2009; 37: 2369–2374 13. Husain FA, Martin MJ, Mullemx PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg
.
2003; 185: 485–491 14. McNelis J, Marini CP, Jurkiewicz A, Szomstein S, Simms HH, Ritter G et al. Prolonged lactic clearance is associated with increased mortality in the surgical intensive care unit. Am J Sarg
.
2001; 182: 481–485 15. Zhang Z, Xu X. Lactate clearance is a useful biomarker for the prediction of allcause mortality in critically ill patients: a systematic review and meta-analysis. Critical Care Medicine.
2014;
42(9): 2118-2125 16. Agadzhanyan VV, Ustyantseva IM, Pronskikh AA, Novokshonov AV, Agalaryan AKh. Polytrauma. Septic complications. Novosibirsk: Nauka Publ., 2005. 391 p. Russian (Agajanyan V.V., Ustyantseva I.M., Pronskikh A.A., Novokshonov A.V., Agalaryan A.Kh. Polytrauma. Septic complications. Novosibirsk: Nauka, 2005. 391 p.) 17. Ustyantseva IM , Khokhlova OI, Petukhova OV, Zhevlakova YuA. Dynamics of the lipopolysaccharide-binding protein and blood lactate of the patients with polytrauma. General Critical Care Medicine
.
2014; 10(5): 18-26. Russian (I.M. Ustyantseva, O.I. Khokhlova, O.V. Petukhova, Yu.A. Zhevlakova. Dynamics of lipopolysaccharide-binding protein and lactate in the blood of patients with polytrauma // General Reanimatology. 2014. Vol. 10, No. 5. P. 18-26) 18. Ustyantseva IM, Khokhlova OI, Petukhova OV, Zhevlakova YuA, Agalaryan AKh. The prognostic value of the inflammation markers, lipopolysaccharide-binding protein and blood lactate in the sepsis development in patients with polytrauma. Polytrauma.
2014;
3: 15-23. Russian (I.M. Ustyantseva, O.I. Khokhlova, O.V. Petukhova, Yu.A. Zhevlakova, A.A. Agalaryan. Prognostic significance of inflammatory markers, lipopolysaccharide-binding protein and lactate in the development of sepsis in patients with polytrauma // Polytrauma. 2014. No. 3. P. 15-23) 19. Butcher I, Maas Al, Lu J, Marmarou A, Murray GD, Mushkudiani NA et al. Prognostic value of admission blood pressure in traumatic brain injury: results from the IMPACT study. J Neuroti- auma.
2007;
24: 294–302 20. Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med.
2009; 37: 1670-1677
View statistics
Loading metrics...
Links
- There are currently no links.
Indications
- Diagnosis of circulatory pathologies resulting in tissue hypoxia (insufficient oxygen consumption by tissues);
- Assessing the degree of acidosis and prescribing resuscitation measures;
- Detection of diseases of the cardiovascular system;
- Suspicion of non-insulin-dependent diabetes mellitus;
- Determining the cause of lactic acidosis;
- Assessment of the acid-base status of the body and blood pH;
- Diagnosis of asphyxia (severe oxygen deprivation) and enzymopathy (impaired enzyme activity) in newborns;
- Pathological changes in muscles and tissues;
- Differential diagnosis of myopathies (hereditary muscle diseases).
The analysis is deciphered by specialists: endocrinologist, cardiologist, oncologist, traumatologist, surgeon, therapist, pediatrician, etc.
- 0.5 - 2.2 mmol/l.
In this case, the ratio of the concentration of lactate and pyruate is assessed, which normally should correspond to 10:1.
Lactate
Lactic acid and pyruvate are substances formed during the metabolism of glucose in glycolysis reactions. Lactic acid is the end product of glycolysis and glycogenolysis. They are indicators of adequate oxygen delivery to organs and tissues and allow one to assess “oxygen starvation” of tissues.Most of the lactic acid is produced in the muscles. Lactic acid formed in the muscles from glucose enters the blood. Further, in the reactions of gluconeogenesis in the liver, lactate is again converted into glucose, which in turn can again be broken down into lactate in the muscles (Cori cycle). Thus, lactic acid is a substance that is normally formed during the utilization of glucose. In cases of mitochondrial dysfunction, which occurs with pathology of energy metabolism and inadequate oxygen supply, lactate accumulates in the blood. Lactic acidosis is divided into two types A and B:
- Lactic acidosis type A - occurs when there is a violation of the delivery or utilization of oxygen by tissues (heart failure, respiratory problems, shock, severe anemia, defects in mitochondrial enzymes or inhibition of mitochondrial enzymes by carbon monoxide or inhibition of mitochondrial enzymes by cyanide).
- Lactic acidosis type B - occurs with excessive formation of lactate or insufficient utilization of lactate (glycogenosis, epileptic seizures, diabetes mellitus, alcohol intoxication, liver failure, malignant neoplasms, salicylate poisoning).
An increase in the content of lactic acid in the blood, caused by hypoxia, is observed during heavy physical activity (5-10 times higher than normal), in pathological conditions accompanied by increased muscle contractions (seizures after epilepsy, tetany, tetanus, various convulsive conditions), shock, bleeding , sepsis, myocardial infarction, pulmonary embolism, cardiac arrest. In the absence of obvious reasons for impaired tissue perfusion, the cause of increased levels of lactic acid in the blood may be diseases such as diabetes mellitus, leukemia and lymphomas, liver damage, renal failure, as well as deficiency of certain enzymes (Gierke's disease - glucose-6phosphatase deficiency, fructose deficiency). 1,6-bisphosphatase). Lactic acidosis can develop after taking large doses of acetaminophen and ethanol, as well as after administering epinephrine, aspirin, insulin, glucagon, fructose, or sorbitol.
Increase in content
- Lactic acidosis type I (increased lactic acid content, absence of pronounced acidosis, normal lactate/pyruvate state): physical activity, hyperventilation, glucagon, glycogenosis, severe anemia, insulin administration, Reye's syndrome.
- Type IIA associated with hypoxia (increased lactate/pyruvate ratio): any condition with inadequate oxygen supply to tissues, acute bleeding, severe acute congestive heart failure or other causes of vascular collapse, cyanotic heart disease or other causes of acute hypoxia, extracorporeal circulation.
- Type IIB, idiopathic (increased lactate/pyruvate ratio): mild uremia, infections (especially pyelonephritis), cirrhosis, third trimester of pregnancy, severe vascular diseases, leukemia, anemia, chronic alcoholism, subacute bacterial endocarditis, poliomyelitis, diabetes (50% of cases) .
Lactate is a diagnostic test to assess the severity of shock.
Lactate (lactic acid) is the end product of glycolysis (aerobic breakdown of glucose). The glycolysis reaction splits a glucose molecule into pyruvate molecules. With a sufficient supply of oxygen, pyruvate is metabolized in mitochondria to the final products: water and carbon dioxide. Under anaerobic conditions, when there is insufficient oxygen supply, pyruvate is converted to lactate. Under resting conditions, the main source of lactate in plasma is erythrocytes. During exercise, lactate is released from the muscles, converted to pyruvate in the liver, or metabolized by brain tissue and the heart. A small amount of lactate is always present in the bloodstream. A significant increase in blood lactate concentration is observed during tissue hypoxia due to decreased tissue perfusion or decreased oxygen content in the blood. The accumulation of lactate in the body leads to acidification of the blood, a shift in its pH to the acidic side, which leads to acidosis. It develops when the supply of oxygen to organs and tissues decreases, as a result of decreased blood flow (sepsis, shock, pulmonary edema, heart failure).
Venous blood lactate is now a valuable diagnostic test for assessing the severity of shock. Lactate levels correlate with poor prognosis in the perioperative period, in the intensive care unit and resuscitation room [6].
Studies have shown that lactate concentrations greater than 2 mmol/L in the blood serum of critically ill patients at the time of hospitalization were associated with a 1.94-10.89-fold increase in their mortality compared with patients whose lactate concentrations were below 2 mmol /l [2,3,4,5,7].
In a study presented by Claridge JA et al. (2000), it was found that persistent hyperlactatemia is a predictor of hospital mortality [1].
Thus, lactate screening and monitoring may be a valuable tool for risk stratification and outcome prediction in sepsis.
Bibliography
- Claridge JA, Crabtree TD, Pelletier SJ, Butler K., Sawyer RG, Young JS Persistent occult hypoperfusion is associated with a significant increase in infection rate and mortality in major trauma patients. // J Trauma - 2000. - Vol.48. – P. 8 – 14.
- Khosravani H., Shahpori R., Stelfox HT, Kirkpatrick AW, Laupland KB Occurrence and adverse effect on outcome of hyperlactatemia in the critically ill. // Crit Care – 2009. – Vol.13. – P. 90.
- Kruse O., Grunnet N., Barfod C. Blood lactate as a predictor for in-hospital mortality in patients acutely admitted to hospital: a systematic review. // Scand J Trauma Resusc Emerg Med – 2011. – Vol.19. – P. 74.
- Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M., Fuchs BD, Shah CV, Bellamy SL, Christie JD Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. // Crit Care Med – 2009. – Vol.37. – P. 1670 – 1677.
- Shapiro NI, Howell MD, Talmor D., Nathanson LA, Lisbon A., Wolfe RE, Weiss JW Serum lactate as a predictor of mortality in emergency department patients with infection. // Ann Emerg Med – 2005. – Vol.45. – P. 524 – 528.
- Cho S.Y., Choi J.H. Biomarkers of Sepsis. // Infect Chemother – 2014. – Vol.46. – No. 1. – P. 1 – 12.
- Wacharasint P., Nakada TA, Boyd JH, Russell JA, Walley KR Normal-range blood lactate concentration in septic shock is prognostic and predictive. // Shock – 2012. – Vol.38. – P. 4 – 10.
General information
Lactate is a product of cellular metabolism that can be present in the body in the form of lactic acid or its salts (normally its content is minimal). Lactate is utilized by the liver, kidneys, heart, and brain. When there is a deficiency of oxygen in tissue cells, the concentration of lactic acid in the blood increases.
When the so-called lactate threshold is reached, when the internal organs do not have time to cope with the volume of lactic acid, lactate begins to accumulate in the body (hyperlactic acidemia). This condition can develop into lactic acidosis (acidification), which the body successfully neutralizes. But in the most severe cases, a violation of the acid-base balance occurs, which is manifested by negative symptoms (weakness, increased breathing, nausea, vomiting, sweating).
Lactic acidosis is divided into 2 types:
Type A - develops against the background of slow blood circulation and insufficient oxygen supply to tissue cells. Type A lactic acidosis accompanies the following diseases:
- severe anemia;
- pulmonary edema;
- cardiovascular failure;
- myocardial infarction;
- sepsis (general infection of the body by pathogenic microorganisms);
- shock due to bleeding or injury;
Type B - occurs when the metabolism of lactic acid is impaired. Examples of type B lactic acidosis:
- diabetes;
- epilepsy;
- renal failure;
- liver pathologies;
- oncological processes (leukemia, lymphoma);
- AIDS;
- severe poisoning with alcohol, salicylates, cyanide, methanol, etc.
Excessive exercise can also release lactic acid.
Under the influence of accumulated lactate, the blood pH changes to the acidic side, which is dangerous to health and requires effective treatment.
To confirm lactic acidosis, a biochemical blood test is performed and 2 components are analyzed: the concentration of lactic acid in the serum, the ratio of lactate and pyruvate.