Tuberculosis is a disease of an infectious-allergic nature, caused by the tuberculosis bacillus and occurring as a chronic inflammatory process in various organs and tissues. The main route of entry of the pathogen into the body is aerogenic, so the disease most often affects the respiratory organs - the lungs, bronchi and trachea, the upper respiratory tract, as well as the pleura and intrathoracic lymph nodes.
The pathology is characterized by a protracted course and a variety of clinical manifestations, and therefore several forms of tuberculosis lesions are distinguished. There are open tuberculosis processes, which occur with the release of the pathogen into the environment, and closed ones, in which the release of Mycobacterium tuberculosis does not occur.
Primary tuberculosis
It is diagnosed much more often in childhood and adolescence, but in recent years it has also occurred in adults. The disease can occur in clinically expressed and erased forms, which depends on many reasons: the amount of the pathogen that has invaded, its pathogenic properties, and the state of the body’s immune system.
The variant with obvious clinical manifestations is characterized by an acute onset with high fever (38–39 °C) and moderate impairment of general condition. Cough, runny nose, redness of the mucous membrane of the pharynx are often observed as manifestations of an allergic reaction, as well as an increase in groups of peripheral lymph nodes. In erased forms of the disease, body temperature is normal or slightly increased, inflammation of the upper respiratory tract is not expressed, and the general condition is practically not affected.
Radiologically, primary tuberculosis is manifested by an area of opacity in the affected lung, similar to pneumonia, as well as expansion of the lung root. A characteristic feature that speaks in favor of a specific process is the lack of a quick positive result when antibacterial treatment is prescribed.
Prevention measures
Provides for the prevention of tuberculosis, first of all, protection from infection with the active form of the disease. To do this, it is undesirable to stay in close quarters for a long time with people suffering from active tuberculosis. To prevent tuberculosis, people in crowded areas should wear protective face masks and follow all hygiene rules. We must not allow the latent form of the disease to become active. Prevention of tuberculosis in children involves protection against infection. To do this, everyone who works in children's institutions should be regularly examined.
Prevention of tuberculosis in children requires mandatory BCG vaccination, as well as chemoprophylaxis of the disease. In addition, in order to prevent tuberculosis, mass examinations of the population are carried out through fluorography. Early detection of signs of tuberculosis allows you to start treatment at the initial stages and make it as effective as possible.
It is equally important to take all measures to strengthen the immune system. In this case, a healthy lifestyle, proper and regular nutrition, complete cessation of smoking, drugs, and alcohol abuse are important.
Disseminated pulmonary tuberculosis
The pathogen enters the lungs through the bloodstream. The source of infection can be existing tuberculosis foci in various organs or a process in the lymph nodes of the root of the lung. The leading place in the mechanism of development of disseminated pulmonary tuberculosis belongs to the body’s reaction to the tuberculosis bacillus, in particular, weakening of the immune system and a decrease in protective forces.
The process can occur acutely, subacutely and chronically. Acute cases occur in children, less often in the elderly. Acute disseminated pulmonary tuberculosis in its debut occurs as an intestinal infection - with fever up to 38 ° C, malaise, headache, and stool upset. Subsequently, the body temperature increases to 39–40°C, rapid heartbeat, dry cough, and shortness of breath appear.
In adults, as a rule, a subacute form of the disease is observed. Its symptoms are no different from an acute process, but increase gradually and are less pronounced. The general condition is slightly disturbed.
Chronic disseminated tuberculosis is the most common variant of the disease. It occurs with a mild clinical picture and is detected in most cases many years after the primary process. The appearance of symptoms of the disease does not indicate the onset of the disease, but an exacerbation of existing tuberculosis.
In the disseminated form, multiple small tuberculous foci are located in both lungs. At the onset of the disease, radiological signs may be absent. After a week, the vascular pattern of the lung tissue changes, acquiring a reticular appearance, and then multiple focal shadows appear. Depending on the degree of activity of the process, the lesions can merge, increasing in size, or become denser, turning into fibrosis.
Forecast
Favorable - complete resorption of specific changes in the lymph nodes.
Relatively favorable -
a) sclerosis of the root of the lung with the subsequent formation of new bronchiectasis. Pathological changes in the bronchi are detected only during bronchoscopy
b) formation of calcifications in the roots of the lungs.
Unfavorable—process progression.
With tuberculosis of the intrathoracic lymph nodes, complications can occur, which are divided into early and late. Early complications of tuberculosis of the intrathoracic lymph nodes: exudative pleurisy is a common complication of tuberculosis of the intrathoracic lymph nodes.
Bronchial tuberculosis occurs due to the spread of the process from the lymph nodes to the wall of the bronchus. Accompanied by the appearance of a severe cough. Microperforation of the bronchial wall with subsequent development of specific endobronchitis. Atelectasis, which can develop due to compression of the bronchus by the affected lymph node (compressive atelectasis) or the development of specific endobronchitis (obstructive atelectasis).
Bronchogenic seeding of the lower parts of the lungs, occurring after perforation of the bronchial wall.
Focal pulmonary tuberculosis
Accounts for about 50% of all detected cases of tuberculosis. It develops against a background of reduced immunity and is characterized by the presence of single or several lesions in the upper parts of the lungs. Unilateral or bilateral lesions may occur.
The clinical course can range from acute to asymptomatic, but even with an acute process, symptoms are usually mild. Patients are bothered by a cough, sometimes hemoptysis, chest pain, as well as increased fatigue, sleep disturbances and digestive disorders - manifestations of chronic intoxication. Body temperature is increased to 37.1–37.5 oC.
The X-ray picture of focal pulmonary tuberculosis is characterized by a variety of manifestations and depends on the stage of the disease. It is possible to identify both fresh forms with blurred boundaries of the foci, and long-existing processes with clear outlines and phenomena of fibrosis.
Infiltrative pulmonary tuberculosis
This form of the disease combines all variants of tuberculosis processes that occur with the formation of foci of compaction (infiltration) in the lung tissue. In this regard, it is characterized by a variety of clinical manifestations, determined by the degree of damage and the stage of the process.
Uncomplicated infiltrative tuberculosis in the active phase resembles the clinical picture of pneumonia. It occurs with high fever (38 °C and above) and is accompanied by a dry cough, chest pain, shortness of breath, and a disturbance in the general condition. With extensive infiltrates, the temperature reaction persists for 2–3 weeks. If the course is unfavorable, infiltrates can spread to the entire lobe of the lung or undergo decay. A favorable outcome is the delimitation of the process and its transition to a focal form.
X-ray images reveal round or cloud-like infiltrates, and in cases of complicated forms, damage to the lung lobe or foci of decay.
How to eat?
Nutrition for pulmonary tuberculosis is aimed at restoring body weight and replenishing the lack of vitamins C, B, A and minerals.
The diet for tuberculosis includes the following categories of products.
- It is recommended to obtain healthy fats from olive, butter and vegetable oil.
- Carbohydrates contained in any foods (cereals, legumes). Honey and flour products are recommended. Easily digestible carbohydrates are found in fruits and vegetables.
- An increased amount of proteins is required due to their rapid breakdown. Easily digestible proteins found in dairy products, fish, poultry, veal and eggs are preferred. Meat products should be boiled, stewed, but not fried.
Food should be high in calories and served freshly prepared. The diet consists of 4 meals a day.
Pulmonary tuberculoma
Tuberculoma is a focus of decay, delimited from surrounding tissues by a dense connective tissue capsule. Education is a variant of the outcome of various forms of pulmonary tuberculosis: primary, focal, disseminated, but more often - infiltrative. Tuberculomas are more common at a young age and can form both with and without the use of antibacterial therapy.
A characteristic feature of tuberculomas is their low-symptomatic and asymptomatic course. Proof of this is the frequent detection of formations during preventive fluorographic studies. Sometimes tuberculomas manifest themselves as a disturbance in the general condition, a slight increase in general temperature, and less often - cough, chest pain.
Radiologically, tuberculoma looks like a heterogeneous shadow with clearly defined boundaries. The number of tuberculomas, their size and location depend on the form of the tubercle process that was their predecessor.
Consequences
Possible complications of pulmonary tuberculosis:
- Generalization of the process through hematogenous spread with the development of tuberculous sepsis.
- Pulmonary hemorrhage. Its massiveness and technical difficulties in stopping it are often the cause of death.
- Development of chronic “pulmonary heart” by increasing pressure in the pulmonary circulation with significant changes in the tissues of the lungs.
- Tuberculous pleurisy. Exudative forms, with a gradual accumulation of fluid in the pleural cavity, also lead to the progression of respiratory failure and subsequent heart failure.
- Spontaneous pneumothorax. Penetration of air into the pleural cavity in significant quantities in cavernous forms can lead to displacement of the mediastinum and reflex cardiac arrest.
Cavernous form of pulmonary tuberculosis
The distinctive features of this form of pathology are the presence of a cavity with thin walls (cavities) without infiltration and fibrosis. Cavities are a source of rapid spread of infection along the bronchial tree, and their thin walls threaten the possibility of dangerous complications.
Cavernous tuberculosis has a varied course, which is associated with the unequal size of the cavities and their different locations, but all cases still have common features. Symptoms of intoxication, such as weakness, increased fatigue, loss of appetite, are mild. Patients are bothered by a cough in the morning with mucous or mucopurulent discharge, as well as pain. Manifestations may be expressed to a greater or lesser extent, or may be completely absent. Their severity directly depends on the degree of narrowing of the bronchus, which prevents secretions from escaping.
X-ray images reveal a thin-walled, round-shaped cavity in the upper sections, sometimes containing fluid. Lung tissue of other parts is often not changed.
Fibrous-cavernous form
It takes years to form and is the final stage of all focal processes in the lungs if they continue. The causes of this form are inadequate treatment or its complete absence.
The leading symptom in persons with fibrous-cavernous tuberculosis is a cough with discharge of various types. In some cases, due to spasm of the bronchial muscles, a paroxysmal cough is observed, the intensity of which is higher in the morning. In the acute phase, the amount of sputum increases, and when the inflammatory phenomena subside, it decreases, and hemoptysis may be observed. Patients experience shortness of breath to a greater or lesser extent.
Dystrophic changes develop in the liver, heart, and kidneys due to prolonged chronic intoxication. In addition, metabolism and the functions of endocrine organs are disrupted.
X-ray allows you to see one or more cavities with dense walls and areas of fibrosis, as well as signs of contamination of the lung tissue.
What it is?
Tuberculosis is a widespread infectious disease caused by various types of mycobacteria from the Mycobacterium tuberculosis complex group (M. tuberculosis and other closely related species) or otherwise Koch bacilli.
In humans, tuberculosis usually affects the lungs, less often affecting other organs and systems. Mycobacterium tuberculosis is transmitted by airborne droplets when a patient talks, coughs or sneezes. Most often, after infection with mycobacteria, the disease occurs in an asymptomatic, latent form (tubal infection), but approximately one in ten cases of latent infection eventually becomes active.
The classic symptoms of pulmonary tuberculosis are a prolonged cough with sputum, sometimes with hemoptysis that appears in later stages, fever, weakness, night sweats and significant weight loss.
Cirrhotic pulmonary tuberculosis
This form of the disease is characterized by the absence of the usual tuberculosis foci and cavities. Cirrhosis, as a process of replacement of lung tissue with connective tissue, can be the outcome of various forms of the disease.
The greatest changes in the cirrhotic form concern respiratory function, which can be severely affected due to a decrease in the working surface of the lungs. In addition, due to the narrowing of the pulmonary vessels, gas exchange deteriorates, further aggravating the phenomena of respiratory failure. The most common complaints are shortness of breath, weakness, cough. Dyspnea, which initially appears during exertion, subsequently occurs at rest. Coughing attacks, more pronounced in the first half of the day, stop for a while after clearing the throat, and then reappear.
Radiologically, cirrhotic tuberculosis is represented by decreased transparency of the affected areas and multiple foci of sclerosis. The unaffected part of the lungs, on the contrary, has increased transparency due to a compensatory increase in healthy tissue.
Tuberculous pleurisy
Develops when the pleura is involved in the pathological process. Tuberculous pleurisy, accompanied by the formation of exudate (effusion), is called exudative, and those occurring without effusion are called dry, or fibrinous. In their development, in addition to the infectious component, many factors take part: features of lymph circulation and immunity, as well as a special state of increased sensitivity of the body to the pathogen, called sensitization.
The main symptoms of dry pleurisy are pain corresponding to the affected area and a dry cough. In some cases, a temperature reaction (37.1–37.5°C) and shortness of breath are observed. Exudative pleurisy often manifests itself as chest pain and fever, which is low at first and then reaches 38°C and higher. A cough, usually dry, is an intermittent symptom of the disease. Even more rarely, a latent course of exudative pleurisy is observed. Among the less common forms of pleurisy, purulent and hemorrhagic are distinguished, but they are practically never encountered.
X-ray signs of pleurisy appear as a shadow against the background of a normal pulmonary pattern. In fibrinous pleurisy, the shadow corresponds to the site of the lesion, and in exudative pleurisy it is located in the posterior and lateral sections, which corresponds to the places where exudate accumulates.
In addition to the described forms of pulmonary tuberculosis, there are several less common, but noteworthy types of damage to the respiratory system.
Tuberculosis of the upper respiratory tract, trachea and bronchi is a complication of various active forms of pulmonary processes, often neglected. The pathology occurs with an uncontrollable cough that is difficult to correct with medication. Sometimes coughing attacks are accompanied by chest pain and shortness of breath.
Tuberculosis of the intrathoracic lymph nodes (tuberculous bronchoadenitis) accompanies the formation of a primary focus in the lungs, and can also occur in isolation. It often occurs with a dry cough and low fever, and sometimes it manifests itself only in general disorders - fatigue, poor sleep and appetite, etc.
Symptoms
The temperature in tumor-like and infiltrative forms can rise to 38-39 ° C, and then remain low-grade for a long time. Children experience “unreasonable” sweating at night, their appetite worsens, and young children develop a cough similar to whooping cough or a bitonal cough. Cough often bothers children at night; At first it is dry, and then phlegm appears.
Paraspecific reactions are very often observed, especially erythema nodosum and phlyctenulous conjunctivitis. In connection with vaccination of children and chemoprophylaxis of tuberculosis, the symptoms of damage to the intrathoracic lymph nodes became less pronounced and erased. The body temperature rises periodically to subfebrile levels, the cough is unstable, sometimes there is coughing, loss of appetite, moderate sweating. There may be no paraspecific reactions.
It is difficult to recognize tuberculosis of the intrathoracic lymph nodes only using physical examination methods, since the nodes are located deep in the chest. The following symptoms are the most common when examining patients.
Visual:
Wiedergoffer's symptom is an expansion of the peripheral venous network in the I-II intercostal space on one or both sides (due to compression of the azygos vein).
Frank's sign is the dilation of small superficial vessels in the upper parts of the interscapular space.
Palpation:
Parsley's symptom is pain when pressing on the spinous processes of the III-VII thoracic vertebrae.
Percussion:
Filosofov's symptom ("bowl" symptom) is a parasternal dullness of percussion sound in the 1st-2nd intercostal space, which narrows downward (damage to the paratracheal lymph nodes).
De la Campa's symptom is a dullness of pulmonary sound in the interscapular region at the level of the II-IV vertebra (damage to the bronchopulmonary lymph nodes).
Koran's symptom is dullness upon percussion along the spinous processes below the first thoracic vertebra (in children 1-2 years old), below the second thoracic vertebra (in children under 10 years old) and below the third thoracic vertebra (in children over 10 years old). The symptom is characteristic of enlarged bifurcation lymph nodes.
And voluntary :
D'Espin's sign - listening to bronchophony on the spine below the first thoracic vertebra.
Heubner's sign is the auscultation of tracheal breathing above the spine (below the 1st thoracic vertebra).
X-ray examination is important in the diagnosis of tuberculosis of the intrathoracic lymph nodes. In this case, it is necessary to conduct studies in anteroposterior and lateral projections, since the shadow of the lymph nodes may be hidden behind the heart and other mediastinal organs. Tomography of the tracheobronchial tree plays an important role. This method is used in children with strict indications, only in the absence of pathological changes on the radiograph and significant clinical symptoms.
Radiologically, in the infiltrative form of tuberculosis of the intrathoracic lymph nodes, the roots of the lungs are expanded and have an indistinct, blurred outer contour due to infiltration of the lung tissue. The tumor-like form of tuberculosis of the intrathoracic lymph nodes is characterized by a more pronounced intensity of the shadow of the roots of the lungs; they have a convex, wavy, clear outline.
On the part of the blood, there may be changes such as slight leukocytosis, increased ESR in the caseous form - lymphopenia.
Diagnosis of tuberculosis
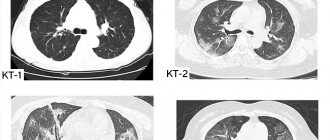
The main methods for detecting pulmonary tuberculosis are radiography and computed tomography (CT). Tuberculin diagnostics and bronchoscopy also play an important role in this. Bacterioscopy and bacteriological techniques make it possible to determine and identify the pathogen. A blood test confirms the presence of an infectious-inflammatory process in the body and indicates its activity.
The variety of clinical and radiological changes in tuberculosis requires the doctor to have deep knowledge and the ability to distinguish its various forms from other diseases. Medical specialists have modern skills and techniques for identifying various pathologies of the respiratory system.
Fluorography
Fluorography is a method of x-ray examination that involves photographing an image from a fluorescent screen that appears on it after X-rays pass through the human body. There are several types of techniques:
- small frame;
- large-frame;
- electronic.
Small- and large-frame fluorography may not show tuberculosis if changes in the lungs are small in size or not clear enough. This is its main drawback, due to which it is impossible to make a diagnosis based on this study. Currently, only electron fluorography is relevant, in which the above disadvantages are eliminated.
It is used to detect tuberculosis during mass preventive studies. Modern fluorography reveals pulmonary tuberculosis thanks to the high quality of the resulting image, the ability to dynamically change the contrast and computer image editing. These features allow you to find the smallest changes.
Here are some examples of what tuberculosis looks like in a fluorography image:

Small-frame fluorogram.
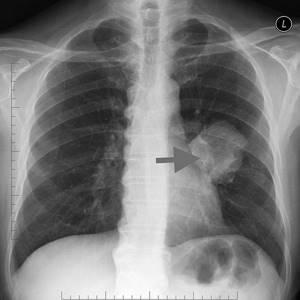
Electronic fluorography. A large focal shadow in the region of the root of the left lung, heterogeneous in structure, has a clear contour.
Principles of tuberculosis treatment
Antibacterial treatment plays a leading role in the treatment of pulmonary tuberculosis. Chemotherapy of all forms of infectious process significantly increases the effectiveness of conservative and surgical treatment. Today, modern phthisiology has a wide arsenal of drugs with different mechanisms of anti-tuberculosis action.
In addition to antibacterial drugs, drugs from other groups are widely used in the treatment of pulmonary tuberculosis - corticosteroids, desensitizing and restorative drugs, immunostimulants, as well as symptomatic therapy - analgesics, antipyretics, expectorants, hepatoprotectors, etc. An important role is given to therapeutic nutrition, adherence to the regimen, and health procedures . Only an integrated approach to the treatment of tuberculosis promotes a rapid and complete recovery.
In case of extensive damage to the lung tissue, as well as in clearly demarcated tuberculosis foci that cannot be resolved, surgical intervention is resorted to. The operation is also indicated to eliminate cicatricial deformities and other late complications of the tuberculosis process.