Clinical signs of brain tumors, as a rule, appear only in the last stages, so early diagnosis of pathologies is important for successful treatment. The magnetic resonance imaging method allows you to obtain layer-by-layer images of the organ with a scanning step of 1 mm. Thanks to the high level of detail and the additional use of contrast agents, MRI shows a brain tumor in the absence of symptoms.
Preparing the patient for MRI of the brain
MRI of the brain: will it show a tumor?
If oncology is suspected, MRI of the brain solves several diagnostic problems:
- detects a pathological focus;
- accurately determines the location of the tumor (extra- or intracerebral location);
- establishes the macroscopic form of formations (appearance, size, secondary changes, etc.).
Like computed tomography, MRI diagnostics is based on identifying direct and indirect signs of head tumors. In the case of CT, the first include a violation of the density of the brain substance, accompanied by calcification of the affected areas. For magnetic resonance imaging, a direct indication of oncology is a change in signal intensity from the tissues in question.
On the tomogram, arrows indicate places with different intensities of the MR signal from tumors: on the left - hyperintense (after contrast), on the right - hypointense signal
Among the indirect signs of a tumor, MR images will show:
- displacement of the midline structures or choroid plexus of the brain (mass effect);
- deviations in magnitude, shift, compression, deformation of the ventricles;
- changes in the basal cisterns of the brain;
- blockade of the cerebrospinal fluid pathways with the development of occlusive hydrocephalus;
- axial dislocation;
- swelling of the brain near the tumor and along the periphery of the formation.
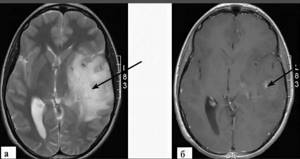
Astrocytoma of the left temporal lobe of the brain on MRI. The tomogram reveals a large formation with a heterogeneous structure and unclear contours, causing a moderate mass effect. T2-weighted image (photo a): a change in the signal from the tumor substance and cerebral edema are determined (arrow); T1-weighted image after gadolinium administration (photo b): focal enhancement of tumor tissue is observed (arrow)
In addition to primary tumors (including those complicated by intraorgan metastases), magnetic resonance imaging shows secondary lesions associated with neoplasms in other areas of the body. They are found anywhere:
- head bones and dura mater (can simulate meningiomas) - characteristic of melanomas, kidney and prostate cancer;
- soft shell of the brain - most often occur with adenocarcinoma of the stomach;
- brain substance - in most cases develop as a result of lung and breast cancer.
What formations can be detected

A brain tumor is not a diagnosis. The diagnosis is, for example, a neuroma - a tumor of tissue along the cranial nerves. Or ependymoma - a tumor disease of the central nervous system. By comparing the MRI readings with symptoms, as well as other tests, the specialist can make a conclusion
- about the primary or secondary nature of the tumor
- its malignancy or benignity
- about the stage of development
A benign brain tumor on MRI is visible as a dark spot with a clear outline that does not spread to other tissues and cells. Due to the variety of tumor diseases, an MRI of the brain for a tumor can only be given by a specialized specialist.
To clarify the diagnosis, additional capabilities of tomographs are used: ultrathin (less than 1 mm) sections are made, differential diagnosis of brain lesions is carried out.
Important!
The capabilities of tomographs are constantly expanding, so when clarifying the diagnosis, it is important to conduct examinations using modern equipment. This will facilitate diagnosis for prescribing the correct treatment. Which can be conservative, without surgery.
Using DWI (diffusion-weighted images), a specialist studies the structure of the pathology and can measure the diffusion coefficient, which is an important indicator for identifying metastases of regional lymph nodes.

Brain edema on MRI: causes of occurrence
Edema is an increase in the volume of brain tissue due to excess fluid accumulation and changes in the lipid structures of cells. This condition is not a separate disease, but the result of the development of various pathologies, including tumors and metastases.
Edema and swelling are the brain’s reaction to the growth of a neoplasm, causing disruption of the normal functioning of nerve cells and the conductivity of synapses, difficulty in blood and liquor circulation due to displacement and infringement of tissue. The larger the size of the tumor and the higher its malignancy, the more pronounced the swelling, which will definitely be shown by MRI.
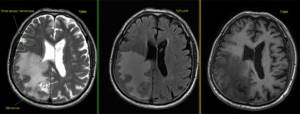
Tomograms of a patient with a history of lung cancer. Noncontrast images of the brain show a focal mass in the right occipital lobe with extensive peripheral edema (photos center and right). After contrast (photo on the left), you can see the metastasis
What can an MRI show?
MRI diagnostics of a brain tumor allows you to obtain visual images of the area being studied. The images are taken in color, and since different tissues of the body have different colors, the pathological area is painted in a different shade compared to healthy tissues. This allows diagnosticians to determine the location of the affected area in the early stages of its development. In this case, it is possible to determine not only the existence and location of lesions, but also the presence of metastases, as well as the degree of penetration of blood vessels into them.
Tomography makes it possible to detect the following pathologies:
- Neoplasms
that are primary in nature. This is the rarest type of gray matter abnormality in which aggressive cells spread exclusively to the body of the brain. - Oncological lesions
of a secondary nature. With this development, the disease, which appeared in other parts of the body, metastasizes to the head area. - Malignant formations
. In this case, MRI reveals oncology, in which there is rapid and uncontrolled growth of cancer cells, crowding healthy tissue and growing through them. At the same time, it is difficult to mark clear boundaries. - Benign lesions
. These areas are characterized by clear dimensions and boundaries. They are separated from the gray matter by their own membrane and have no penetrating processes.
The distinctive signs of malignant tumors in the images include:
- fuzzy outlines;
- irregular shape;
- mass effect, that is, displacement of nearby structures;
- clear perifocal edema;
- heterogeneous distribution of contrast, which sometimes does not accumulate at all;
- hydrocephalus;
- “variegation” caused by necrosis, hemorrhages and/or cysts.
Note!
If cancer is suspected, an examination using a contrast agent administered intravenously is usually prescribed. It colors the damaged areas, making them visible even in the early stages.
What does brain cancer look like on an MRI - photo?
Signals from tumors vary depending on the MR scanning program. In T1 WI mode, neoplasms are usually hypointense; in T2 WI mode they can be of any kind. Post-contrast images are of great importance for differentiating malignant and benign pathologies. Aggressive blastomas are usually colored heterogeneously on tomograms due to foci of necrosis, calcifications, and hemorrhages. Some types of tumors (for example, diffusely growing astrocytoma) do not accumulate contrast agent or the enhancer is concentrated in different places.
Benign formations are located in a dense capsule and, as they increase in size, push away neighboring tissues without growing inside. When scanning, the images will show a clear delineation of the affected area from other structures.
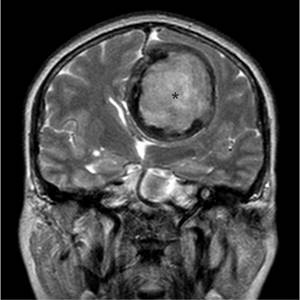
On an MRI scan, an asterisk indicates a benign tumor in the capsule.
Typical for malignant brain processes are:
- lack of pronounced contours;
- infiltrative type of growth: pathology develops between healthy cells, damaging the latter;
- necrotic decay (self-digestion of the tumor in the affected area);
- hemorrhages into the mass of formation: newly sprouting vessels are defective and easily damaged;
- the presence of cysts and calcifications within the tumor.
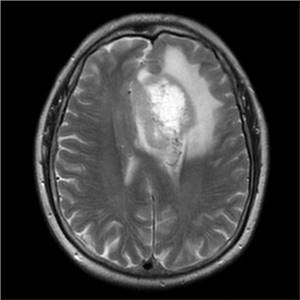
Malignant neoplasm of the left frontal lobe of the brain without clear boundaries, with edema and signs of necrotic decay
Metastatic tumors consist of tissue from damaged organs that enter the brain through the bloodstream. On tomograms, secondary formations have pronounced outlines, and swelling is visualized around them. Sometimes multiple metastases merge, forming one large lesion. Based on the characteristics of the signal, a specialist can determine where exactly the malignant cells supposedly entered the brain.
It happens that MRI does not show the pathological process. For high-quality imaging of organs and systems, a tomograph with a high magnetic field voltage is required. If a tumor is suspected, it is recommended to do a head scan using a closed-type device from 1.5 Tesla with intravenous contrast enhancement.
MRI and oncology
Diagnostics to identify tumor processes is in some cases indicated and strictly mandatory. The absence of radiation exposure to the patient’s body makes it possible to conduct research regularly and monitor processes over time. If oncology is suspected, the picture can be taken again. MRI studies using modern tomographs:
- are distinguished by clear visualization of three projections;
- provide better spatial resolution;
- determine not only the size and area of the tumor, but also the structure.
The non-invasiveness of the method and the absence of contraindications for most patients allows us to state that MRI detects oncology with a high degree of probability.
Diagnosis of brain tumor diseases
In order for an MRI to show a brain tumor, a so-called contrast agent must be injected before the procedure, the volume of which is determined depending on the patient’s weight.
Next, the patient is asked again about implants, including dental ones. Modern metal-ceramic fillings are not a contraindication to the procedure. Denture pins are now made mainly from paramagnetic materials, but this should be checked with the treating dentist.
Important!
Strict contraindications for MRI diagnostics are the presence of metal or non-ferromagnetic implants or electronic support devices in the body.
Also, medical plates are made from paramagnetic material (titanium), which are used, among other things, in the treatment of injuries to the head, legs, and spine. The presence of such a plate does not interfere with diagnosis.
If the procedure is indicated, then after the administration of “contrast”, the patient is given projection photographs of the head, which make it possible to determine:
- determine the presence and location of an anomaly;
- the presence of secondary foci (metastases);
- the degree of vascular supply of secondary lesions.
If a tumor is suspected, MRI diagnostics is performed again. If there are difficulties in prescribing treatment, the procedure may be repeated several times.
MRI for brain cancer
Remember: the sooner you detect a pathology, the greater the chance of quick and successful treatment! An MRI is the best way to help yourself get better. However, it is important that the examination is carried out by experienced doctors using modern equipment. Otherwise, there is a risk of missing pathology.
The Elena Malysheva Diagnostic Center is your confidence in the quality of MRI diagnostics! Qualified doctors with many years of experience and the latest expert-class tomograph are at your service to obtain the most accurate results!
Sign up for an MRI at the Elena Malysheva Diagnostic Center near the Baumanskaya metro station (see map) by phone or leave a request on the website.
Baumanskaya metro station (see map) 8
leave a request on the website
Treatment
Surgery is an effective method for many types of metastases and is especially indicated for the treatment of tumors that are not sensitive to radiation.
To decide on indications for surgery, the patient’s general condition, the technical feasibility of removing metastases, and the prospects for combined treatment in the presence of metastatic lesions of other organs and systems are assessed.
Modern technical capabilities make it possible to diagnose and operate metastases at an early stage and small sizes.
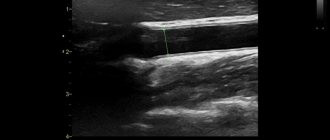
The use of modern ultrasound diagnostic methods makes it possible to accurately localize the tumor, determine the direction of access and avoid damage to functionally significant areas of the brain.
Removal of metastatic tumors, especially large ones and located in functionally important areas, is usually carried out according to the same principles as other CNS tumors, i.e. fragmentation.
The likelihood of complete destruction of the tumor after surgery can be increased by irradiating the tumor bed with a laser beam. Experimental work is underway on the use of photodynamic therapy during surgery.
RADIATION THERAPY
For metastatic tumors of the central nervous system, irradiation of the entire brain is necessary in most cases. For this purpose, lateral opposite fields are used.
They should cover the space from the vault to the base of the skull and from the upper edge of the orbit to the mastoid process. If the tumor is located in the lower part of the frontal or temporal lobe, the radiation field should cover the lower edge of the orbit and the external auditory canal. In this case, blocks are installed on the lens and base of the skull.
The usual dose is 20 Gy in 4-5 fractions or 30 Gy in 10-12 fractions.
Considering the long-term side effects (dementia) at a dose of 30 Gy in 10 fractions, it has recently been recommended to carry out irradiation in fractions of 1.8-2 Gy, but the effectiveness of treatment in this case decreases.
When treating single metastases, local irradiation of the lesion is added to a total dose of 50 Gy. In the presence of deeply located and (or) multiple small metastases, radiosurgical treatment is indicated.
Prophylactic irradiation of the brain after removal of small cell lung cancer reduces the number of intracranial metastases, but does not affect survival rates.
CHEMOTHERAPY
The choice of chemotherapy regimen depends on the nature of the primary source of metastasis.