Periodontitis is an inflammation of the periodontium - the connective tissues that are located between the root part of the tooth and its bone bed, alveolar processes. In addition to nerve endings, it contains many capillaries and vessels that are vulnerable to infections. As a rule, this disease is a complication of pulpitis (when inflammation of the nerve turns into necrosis and the products of nerve decay begin to penetrate into the bone tissue around the tooth root).
the difference between pulpitis and periodontitis in the localization of the inflammatory process
Symptoms of periodontitis
- continuous throbbing pain, both with and without contact with the tooth;
- a sharp unpleasant odor from the mouth that cannot be gotten rid of;
- swelling of the gums;
- feeling of heaviness and mobility of teeth;
- a sharp change in the color of the enamel - darkening or yellowing;
- accumulation of pus in periodontal pockets.

purulent fistula on the gum with chronic periodontitis
Causes of periodontitis
The etiology of periodontitis in most cases is associated with advanced forms of caries. When the pulp is damaged, the inflammation spreads to the root of the tooth and then spreads through the canal to the periodontium. In addition, the causes of the disease can be:
- tooth trauma - fracture or crack of the root, bruise, chipped crown with subsequent penetration of infection into the pulp;
- violation of the root canal treatment technique with tissue injury with sharp instruments;
- violation of the root canal filling technique with filling material extending beyond the root apex;
It is important for the dentist to find out the cause of periodontal inflammation in order to select the optimal treatment regimen for the tooth and prevent relapse.
Kinds
There are many types of periodontitis, and dentists distinguish several classifications - depending on the source of inflammation, the stage and form of the disease.
By localization:
- Marginal – a type of periodontal lesion at the gingival margin. Most often it occurs due to traumatic factors - even a minor chip can provoke the disease.
- Apical - inflammation in the apical part of the root. It is often misdiagnosed as a form of pulpitis (nerve inflammation).
By stage:
- Acute form - can be of serous and purulent type. The second type is dangerous due to serious complications, further development of purulent inflammation in nearby tissues, development of abscesses or phlegmon of the oral cavity.
- The chronic form is divided into fibrous, granulating and granulomatous periodontitis. Often it is practically asymptomatic, but exacerbations with severe pain are periodically possible.
Acute periodontitis –
In accordance with the theory of the course of the inflammatory process, the acute form of periodontitis is usually divided into serous and purulent forms. Diagnosis of acute serous and acute purulent periodontitis is carried out only by symptoms, because There are usually no changes on the x-ray.
This is due to the fact that the diagnosis of “acute periodontitis” is made only when it first occurs. It can arise, for example, as a consequence -
- during untreated pulpitis,
- poor-quality filling of canals (after treatment of pulpitis).
Acute serous periodontitis –
Symptoms - at first, the pain may be spontaneous, which is due to the fact that the inflammatory exudate accumulating in the periodontium is localized in a confined space, and therefore it compresses the nerve endings. The pain intensifies sharply when biting on a tooth.
It is periodontal edema that is associated with patients’ complaints about the feeling of elongation of the causative tooth, and its premature closure with antagonist teeth of the other jaw. The swelling actually causes the causative tooth to protrude slightly vertically.
There may be slight swelling of the soft tissues of the face in the projection of the causative tooth, but upon palpation (feeling) it is usually painless. Since the pulp, as a rule, is already dead during the development of periodontitis, probing the carious cavity is usually painless. There are still no changes on the x-ray at this stage of inflammation.
Acute purulent periodontitis –
Symptoms: After about two days, the serous stage of inflammation turns into a purulent stage. This is associated with a significant increase in symptoms. Painful sensations take on the character of throbbing pains with rare pain-free intervals.
As a result of the pus melting the periodontium (the ligamentous apparatus of the tooth), the tooth becomes mobile. Significant swelling of the soft tissues of the face may occur. The gums in the area of the causative tooth are usually sharply painful when pressed. The radiograph still does not show any significant changes.
Stages of development of acute purulent periodontitis (Fig. 1-4) –
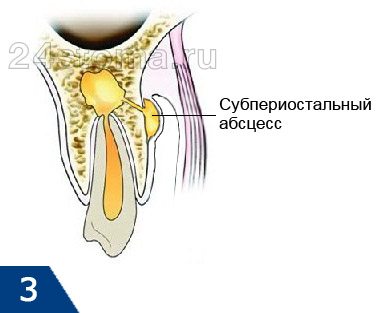
- Periodontal stage - the purulent process is limited to the area of the periodontal fissure, i.e. a microabscess occurs in the area of the apex of the tooth root (Fig. 1). Clinically, this may correspond to the appearance of a feeling of an overgrown tooth.
- Endosseous stage - pus penetrates the bone tissue and infiltrates it (Fig. 2).
- Formation of a subperiosteal abscess - pus accumulates under the periosteum (Fig. 3). Clinically manifested by severe swelling of the gums, soft tissues of the face, and severe pain. Patients call this gum flux.
- Submucosal stage - destruction of the periosteum occurs and pus comes out into the soft tissues (with the formation of an abscess in them). After the periosteum breaks through, the pain immediately subsides, because tension in the focus of purulent inflammation decreases. But at the same time, swelling of the soft tissues of the face increases (Fig. 4).
Acute purulent periodontitis: video
In the video you can see how, when opening a tooth with acute purulent periodontitis, pus begins to emerge from the mouth of one of the root canals.
Treatment of periodontitis
Treatment of periodontitis is prescribed depending on the clinical picture. In most cases, it involves several stages with x-rays, as well as the use of drug therapy. In advanced forms, a course of antibiotics is prescribed, and physiotherapeutic procedures are recommended.
The standard course of treatment consists of the following stages:
- Preliminary examination, including x-rays, determining the form of the disease and the extent of the lesion.
- Treatment of dental canals, rinsing with antiseptic preparations.
- In acute purulent phases - dissection of the gums to drain the pus.
- Repeated cleaning of the canals, control x-ray or computed tomography.
- Installing a temporary filling with a medicinal product containing antiseptics to get rid of the effects of inflammation.
- Removing the temporary filling after a week, re-processing and washing the canals. Repeated filling of the canals with a drug. The procedure is repeated until the doctor is convinced that all traces of suppuration have been removed and the risk of relapse is minimal.
- Installation of a permanent filling.

Even an experienced dentist will not give specific dates. Some patients manage to cure periodontitis in one week, while others have to visit the clinic for six months. The greatest difficulties are caused by chronic forms of periodontitis; in such cases, treatment can last up to six months
It is important to follow the doctor’s instructions for the entire period of treatment. Physiotherapy includes UHF and electrophoresis as additional measures.
Chronic apical periodontitis –
Chronic periodontitis is most often the outcome of an acute process, but in some cases it can develop independently (especially with weak immunity). Chronic periodontitis occurs, as a rule, asymptomatically, or with slight pain when biting on the causative tooth.
Severe symptoms appear only during exacerbation of a chronic process, which can be triggered by hypothermia of the body, decreased immunity after suffering from acute respiratory viral infection. There are 3 forms of chronic periodontitis...
Chronic fibrous periodontitis –
It is characterized by the fact that periodontal fibers (the ligamentous apparatus of the tooth that connects the tooth to the bone) are gradually replaced by connective fibrous tissue. Chronic fibrous periodontitis has extremely few symptoms, and pain may be completely absent.

Sometimes a diagnosis can only be made based on an x-ray. If on an x-ray the normal periodontium is defined as a narrow uniform strip between the tooth root on one side and the alveolus of the bone on the other, then with fibrous periodontitis there is sometimes a significant expansion of the periodontal fissure.
Chronic granulating periodontitis –
This is the most active form of chronic periodontitis. It is characterized by the appearance in the area of the root tips - granulation tissue, which visually looks like loose granular tissue of red color. Granulation tissue has the ability to grow rapidly, which leads to active bone destruction and its replacement with granulation tissue.
Symptoms – patients complain of aching pain, which periodically worsens. Biting on a tooth and tapping it causes a moderate pain reaction. There may be a fistula on the gum in the projection of the causative tooth, from which scanty purulent discharge will be released.
On an x-ray – chronic granulating periodontitis is very clearly visible on x-rays. In the projection of the apex of the tooth root, an irregularly shaped darkening with flame-like outlines is determined. This darkening indicates that the bone tissue in this area has collapsed and has been replaced by granulation tissue.
Chronic granulomatous periodontitis –
Chronic granulomatous periodontitis is characterized by the formation of something like a purulent sac at the apex of the root. Depending on the size of this formation, it is customary to distinguish the following 3 types of this form of periodontitis: granuloma, cystogranuloma and radicular cyst. They have the same structure, are filled with pus, and differ only in size...
- Granuloma - differs in that it measures up to 0.5 cm in diameter. Treatment for granuloma is relatively simple, unlike larger lesions.
- Cystogranuloma – has dimensions from 0.5 to 1 cm in diameter.
- Cyst - a formation at the apex of the root is called a cyst when its diameter exceeds 1 cm. Cysts can reach 5-6 cm in diameter, and even completely fill, for example, the maxillary sinus of the upper jaw. For cysts measuring 1-1.5 cm, conservative treatment is possible, and for larger ones, surgical removal is recommended.
Granuloma and cyst on x-ray –
An x-ray shows a darkening with clear, even, rounded contours in the area of the apex of the tooth root. This darkening indicates that bone tissue has resolved in this area. The even, clear contours of such darkening indicate that the formation (cystogranuloma or cyst) has a dense capsule that is not connected to the surrounding bone tissue.
Due to what growth occurs - the growth of these formations and their transformation into each other - occurs due to a constant increase in the amount of pus inside the formation, which leads to an increase in the pressure of the formation on the surrounding bone tissue. The bone is dissolved under pressure. As a result, education occupies a new space, and then everything starts all over again. As the granuloma grows, it turns into a cystogranuloma, and the latter into a cyst.
Symptoms of granulomatous periodontitis - this form of periodontitis, in terms of the nature of its course, occupies an intermediate place between the sluggish fibrous form of periodontitis and the aggressive course of granulating periodontitis. At the beginning of its development, chronic granulomatous periodontitis has very poor symptoms, and biting on a tooth or tapping on it does not always cause pain. However, at a later date, the symptoms intensify (24stoma.ru).
What does a granuloma/cystogranuloma look like (at the apex of the root of an extracted tooth):
Complications of periodontitis
With improper treatment or untimely diagnosis, the patient develops extensive purulent inflammation - multiple ulcers, abscesses and fistulas appear. All this leads to the development of such dangerous diseases as:
- flux;
- periostitis;
- dental cyst;
- osteomyelitis;
- extensive blood poisoning (sepsis).
The possible consequences of each of the complications are very serious. They often lead to hospitalization, surgery and a long rehabilitation period.

complication of dental periodontitis - purulent fistula on the skin
Traumatic periodontitis
Periodontal trauma is one of the initiating factors in the occurrence of hemorrhage and the development of ischemia, which directly leads to the formation of pulp necrosis. The focus of necrosis attracts bacteria, colonizes them and infects the periodontium. With an increase in the number of microorganisms, acute inflammation begins. Traumatic periodontitis develops.
With chronic long-term trauma, periodontal restructuring occurs gradually, first due to its adaptation, then as chronic inflammation with lacunar resorption of the compact lamina.
The main reason for the development of pathology is the inflammatory response. As a result of occlusal trauma, inflammatory mediators are produced in the pulp; they are considered a protective reaction to mechanical aggression. They disrupt microcirculation and increase vascular permeability. The pulp dies.
When pulp necrosis reaches the apical periodontium, due to its cytotoxic effect, interleukins activate osteoclasts and bone resorption.
Prevention
To avoid any form of periodontitis, you must follow simple recommendations from dentists, which apply to most clinical cases:
- You need to brush your teeth at least twice a day - the brush should not be too hard, so as not to injure the gums or introduce infection into the soft tissues.
- After each meal, use mouthwash - if you don’t have a special liquid on hand, just rinse your mouth thoroughly with warm boiled or filtered water.
- Visit the dentist at least 2 times a year - a scheduled appointment allows you to identify most diseases in the early stages, begin treatment in a timely manner and avoid serious consequences.
- Have your teeth professionally cleaned and tartar removed annually – even minor plaque creates conditions for the proliferation of pathogenic bacteria.
General advice for everyone includes giving up bad habits. Smoking and alcohol contribute to the deterioration of dental health, as well as their attractiveness and natural whiteness.
Exacerbation of chronic periodontitis
At this stage, all symptoms resemble the acute form. There is sharp pain, swelling and growth of lymph nodes. Considering that a chronic disease leads to bone destruction, during an exacerbation there is a risk of exudate getting inside the jaw. There is a possibility of a fistula.
The patient feels weak, his body temperature rises, and complaints of feeling cold arise.
What exactly are the consequences if chronic periodontitis worsens?
- Violation of the integrity of a periodontal type abscess. In the case of granulomatous periodontitis, the inflammatory area has boundaries of strong fibrous tissue in the form of a bag of pus. Excessive load on the tooth negatively affects the infected lesion, which is at rest. As a result, the pressure increases and the capsule ruptures, and the infection goes beyond the limits, leading to an exacerbation.
- Improper drainage of purulent contents. With granulomatous and granulating forms, pus is continuously discharged. However, it successfully exits through a fistula or root canals, ending up in the area of caries. Thus, the patient does not feel discomfort. But when the exits are closed, the pus accumulates, bursts and becomes inflamed. Pain and swelling occur.
- Reduced protective properties of the body. As a result, all those factors that previously prevented periodontal infections from growing and developing no longer carry out their main protective function. The infection is spreading on a large scale.
How to prevent the development of the disease? Prevention
The main preventative point is the treatment of caries immediately after the onset of dental problems. The infection enters the periodontium through the carious area. To prevent marginal or marginal types of disease, in which the infection passes through the deep periodontal areas, it is important to monitor the condition of the gums. Periodontal treatment immediately after its appearance, as well as timely removal of tartar, is of great importance.
Acute forms of the disease are eliminated using an integrated approach to treatment in order to prevent the anomaly from moving to the chronic stage. This rule fully depends on the qualifications of the doctor and the availability of high-quality equipment in the clinic.
SYMPTOMS OF THE DISEASE
Granulating periodontitis manifests itself as periodic dull pain in the gum area: it hurts to bite hard foods and chew. When tapping, a characteristic pain also appears. The affected tooth becomes mobile. Unlike pulpitis, there are no pronounced reactions to hot/cold or spontaneous night pain.
Characteristic signs of the disease in the acute stage are hyperemia of the mucous membrane, swelling, fistulas with purulent discharge, unpleasant odor, symptoms of general intoxication (headache, weakness, enlarged lymph nodes).
If treatment is not started, the number of granulations increases, they grow quickly, come to the surface and turn into fistulas, through the open channels of which re-infection with microorganisms occurs, the disease takes a protracted form.
Classification of periodontitis
It is believed that the main cause of periodontitis is complications from caries (pulpitis), when the inflammatory process moves to the apex of the root and tooth root periodontitis occurs. This is indeed one of the most common reasons, but this does not always happen.
Classification of periodontitis by reason of occurrence
| Type of periodontitis | Price for installation of one implant |
| Infectious | The most common type of disease when a chain of caries occurs is pulpitis - periodontitis. Appears both after primary and secondary caries. It can be difficult to detect visually (especially periodontitis under a crown or filling). |
| Medication | Periodontitis after dental treatment. Occurs when potent or toxic drugs (arsenic, formaldehyde, phosphate cement, etc.) enter the periodontium. It can often be a consequence of an allergy to certain medications. |
| Traumatic | Its cause is mechanical damage, including due to an incorrectly installed seal. May become infectious. |
Types of periodontitis
The disease is classified according to its defining characteristics:
- for reasons of occurrence: infectious (caries, pulpitis, infection from nearby foci of infection), medication (during the treatment of other ostomy problems) and traumatic;
- according to the course: acute (develops over 2–3 days, diagnosed only by symptoms) and chronic (sluggish nature with periodic exacerbations, diagnosed radiographically).
The chronic form, in turn, is divided into several subtypes:
- fibrous – an increase in the volume of fibrous tissue and expansion of the periodontal gap;
- granulating - rarefaction of the mow structure under the tooth root, formation of pus with release into the fistula;
- granulomatous – formation of granulomas and cysts (purulent formations).
Surgery
If the granuloma is large and cannot be removed therapeutically, it becomes necessary to resect the upper part of the root. To do this, the canal is filled with materials that quickly harden but do not dissolve. It is allowed to use the material in excess, since the doctor will remove it later. During the operation, high-quality anesthesia will be required. The dentist cuts the gum and widens the area of the jaw where the granuloma is present. At the site of destruction, the bone and part of the root are cut out and the granulation is scraped out. Instead, an antibacterial substance is compacted and the wound is sutured. It is recommended to install drainage for a day.
There are situations when the entire tooth needs to be removed. Reasons include obstruction of the root canals, lack of treatment effect, closely located mandibular canal, etc. After removal, the inflamed area goes away on its own. But there are cases when it is necessary to make an incision, disconnect the periosteum and install drainage. This manipulation is carried out when there is an accumulation of pus that did not come out during tooth extraction.
Indications for treatment
The following indications exist for conservative treatment:
- Periodontitis of acute and chronic forms of single-rooted teeth, when the periapical tissues have not undergone large-scale changes.
- Periodontitis of acute and chronic forms of multi-rooted teeth, subject to patency of the canals and the absence of an irreversible process in the periapical tissues.
How is periodontitis eliminated? Treatment of the disease at the chronic stage
Regardless of the form, the root cause must be addressed first. To do this, the doctor works in the main root canal and its branches, as well as in the periodontium itself. If exudate is present, it must be quickly released. At the end of treatment, the gap between the periodontium and the root canals is carefully sealed.
Contraindications to treatment
Absolute contraindications for this type of treatment include:
- Severe changes in periapical tissues (cyst, cystogranuloma) with the presence of focally caused ailments.
- Obstruction of the canals at the acute stage.
- Tooth mobility of 1I-IV degrees, when the alveolar arch at the level of the diseased tooth has atrophied.
- Cysts of peri-root teeth with root penetration into the pathological process.
- Irreversibility of the course of the disease and the impossibility of performing post-apical therapy.
- Perforation of a cavity or tooth root.
Therapeutic treatment
Chronic periodontitis is often successfully treated with therapy. To do this, the carious area is prepared and the old filling is removed. Continuous treatment of the affected area with an antiseptic is mandatory. After removing the old filling, measures will be needed to ensure the unimpeded outflow of exudate and rinsing the cavity with an antiseptic.
The following measures will help enhance the effect:
- Phonophoresis with the introduction of an antiseptic under the influence of ultrasound into microtubules.
- Electrophoresis with potassium iodide and other antiseptics, in which molecules quickly form polarized ions.
- Laser treatment. The laser affects the disease in two ways at once: it sterilizes the root canal, removing bacteria, and releases special oxidizing agents that arise under the influence of radiation from more complex molecules as a result of their breakdown.
Elimination of the disease at the acute stage is carried out, starting with the demobilization of the factors that led to this condition. Antiseptic is not enough for this. Good drainage will be required, as well as antibacterial therapy.
When the root cause of the exacerbation is destroyed, with granulating periodontitis the doctor acts on the tissue using various means (calcium hydroxide). The same measures are taken in the case of the granulation form.
At the end of therapy, the tooth is sealed, as well as the canal is filled, if the patient has no complaints.