Detailed description of the study
Pseudomembranous colitis is a disease of the colon caused by the bacteria Clostridium difficile. It occurs in people whose normal intestinal microflora is disrupted, usually due to recent use of antibiotics. The disease may develop against the background of long-term asymptomatic carriage of this type of clostridia or infection with this bacterium in a medical institution.
C. difficile is a spore-forming bacteria that, when overproduced, produces toxins A and B. These toxins are the main cause of the inflammatory response in the colon, which leads to increased vascular permeability and the formation of gray-yellow plaques (pseudomembranes) on the mucous membrane intestines. This condition is known as pseudomembranous colitis, or Clostridioides difficile-associated colon disease.
C. difficile is one of the most common causes of diarrhea in hospitals worldwide. This is facilitated by the transmission of infection from a sick person or carrier due to insufficient hand washing, changing bed and underwear, using shared showers and toilets, and inattention to careful personal hygiene.
The main risk factors for the development of pseudomembranous colitis are old age, severe concomitant diseases, previous use of broad-spectrum antibiotics and prolonged hospitalization. Medicines that suppress stomach acid also increase the risk of developing this disease.
Symptoms of pseudomembranous colitis include watery diarrhea, sometimes mixed with blood, abdominal pain and increased gas production. The frequency of stool depends on the severity of the disease. In addition, in severe cases, there is an increase in body temperature to 38-39 C, and there is a risk of complications in the form of pathological expansion of the intestinal area (toxic dilatation).
Laboratory diagnosis of pseudomembranous colitis is based on the detection of C. difficile toxins A and B in the stool. This is a reliable way to identify waste products of bacteria, which does not require complex manipulations to collect biomaterial, which helps to quickly prescribe optimal treatment.
Clostridium (clostridia)
Clostridia
(lat.
Clostridium
) - a genus of gram-positive spore-bearing bacteria.
Clostridia are part of the normal human microflora. However, some types of clostridia can cause disease. The name “clostridia” comes from the Greek κλοςτεδ
(spindle), since during sporulation the clostridia swell in the center and take on the shape of a spindle.
Clostridia - normal human microflora
Clostridia are found in healthy people in the intestines, in the female genital tract, and sometimes on the skin and in the mouth. The main habitat of clostridia in the human body is the large intestine. There are no clostridia in the duodenum and jejunum; in the ileum, their population is normally 102–104 colony-forming units (CFU)/ml. The following amounts of clostridia are found in the stool of healthy people:
- in children under one year of age - up to 103 CFU/g
- in children over one year old and adults up to 60 years old - up to 105 CFU/g
- in adults over 60 years old - up to 106 CFU/g
During their life activity, clostridia produce short-chain fatty acids: butyric, isobutyric, valeric, capronic, isovaleric, isocaproic (Akopyan A.N.).
Clostridia are pathogens
Most clostridia are not pathogenic, but some types of clostridia can cause various human diseases, some of which are severe and can be fatal. In particular, Clostridium botulinum
can cause botulism,
Clostridium tetani
- tetanus,
Clostridium perfringens, Clostridium novyi, Clostridium oedematiens
and
Clostridium septicum
- gas gangrene.
Clostridium perfringens
can also cause foodborne illness due to a toxin produced by
Clostridium perfringens
.
8–14 hours after eating Clostridium perfringens-
meat, poultry, or legumes, watery diarrhea, nausea, abdominal cramps, and sometimes fever begin. The duration of the illness is one or two days.
Clostridium perfringens
type A can cause antibiotic-associated diarrhea or pseudomembranous colitis.
Clostridium perfringens
type F can cause necrotic enteritis.
Clostridium tetani
is the causative agent of tetanus, an acute infectious disease of humans and animals, characterized by damage to the nervous system and manifested by tonic tension of skeletal muscles and generalized convulsions.
Clostridia can cause diseases of the human genitourinary organs, in particular acute prostatitis.
By Order of the Ministry of Health and Social Development of Russia No. 1664n dated December 27, 2011 “On approval of the nomenclature of medical services,” medical and “A26.19.007 Bacteriological examination of stool for clostridium (Clostridium spp.)” are included in the nomenclature of medical services, section 26.
Antibiotics active against clostridia
Antibacterial agents (those described in this reference book) active against clostridia: metronidazole, tinidazole, rifaximin, tetracycline, doxycycline, lincomycin.
Clostridia species resistant to clindamycin: Clostridium sporogenes
and
Clostridium tertium.
Clostridia in the taxonomy of bacteria
According to modern classification, the genus of Clostridia is included in the family Clostridiaceae
, order
Clostridiales
, class
Clostridia
, phylum
Firmicutes
, <group without rank>
Terrabacteria group
, kingdom Bacteria.
The genus Clostridia includes more than 100 species: C. aceticum, C. acetireducens, C. acetobutylicum, C. acidisoli, C. aciditolerans, C. aestuarii, C. akagii, C. alcalibutyricum, C. alcaliphilum, C. algidicarnis, C. algifaecis, C. algoriphilum, C. amazonense, C. aminobutyricum, C. aminovorans, C. amylolyticum, C. arbusti, C. argentinense, C. aurantibutyricum, C. autoethanogenum, C. baratii, C. beijerinckii, C. bogorii, C. boliviensis, C. bornimense,
C. botulinum , C. bovipellis, C. bowmanii, C. butyricum, C. cadaveris, C. caliptrosporum, C. caminithermale, C. carboxidivorans, C. carnis, C. cavendishii, C. celatum, C. cellulovorans, C. chartatabidum, C. chauvoei, C. chromiireducens, C. cochlearium, C. colicanis, C. collagenovorans, C. corinoforum, C. coskatii, C. crotonatovorans, C. cylindrosporum, C. diolis, C. disporicum, C. drakei, C. elmenteitii, C. estertheticum, C. fallax, C. favososporum, C. felsineum, C. filamentosum, C. formicaceticum, C. frigidicarnis, C. frigoriphilum, C. frigoris, C. fusiformis, C. ganghwense, C. gasigenes, C. grantii, C. guangxiense, C. haemolyticum, C. halophilum, C. homopropionicum, C. huakuii, C. hveragerdense, C. hydrogeniformans, C. hydrolyticum, C. ihumii, C. intestinale, C. isatidis, C. islandicum, C. kluyveri, C. kogasensis, C. lacusfryxellense, C. liquoris, C. ljungdahlii, C. longisporum, C. lundense, C. luticellarii, C. magnum, C. malenominatum, C. massiliodielmoense, C. maximum, C. merdae, C. moniliforme, C. neonatale, C. neuense, C. nitrophenolicum, C. novyi, C. oceanicum, C. oryzae, C. paraputrificum, C. pascui, C. pasteurianum, C. peptidivorans, C. perfringens, C. phoceensis, C. polyendosporum, C. polynesiense, C. proteolyticus, C. psychrophilum, C. punense, C. puniceum, C. putrefaciens, C. quinii, C. ragsdalei, C. roseum, C. saccharobutylicum, C. saccharoperbutylacetonicum, C. sardiniense, C. sartagoforme, C. saudiense, C. scatologenes, C. schirmacherense, C. senegalense, C. septicum, C. sordelli, C. sporogenes, C. subterminale, C. sulfidigenes, C. swellfunianum, C. taeniosporum, C. tagluense, C. tarantellae, C. tepidiprofundi, C. tepidum, C. tertium, C. tetani, C. tetanomorphum, C. thermobutyricum, C. thermopalmarium, C. thermophilus, C. thiosulfatireducens, C. tunisiense, C. tyrobutyricum, C. uliginosum, C. uzonii, C. ventriculi, C. vincentii, C. vulturis, [Butyribacterium] methylotrophicum
.
Clostiridia C. sporogenes
and others have active proteolytic enzymes and are able to use proteins and peptides as substrates, hydrolyzing them to amino acids and then subjecting the latter to fermentation. Such clostridia belong to the group of proteolytic clostridia.
Formerly clinically important species Clostridium perfringens
called
Clostridium welchii
.
Changes in the composition of the genus Clostridium
In recent years, clostridia have been seriously reclassified, in particular:
The most important clinically important species is Clostridium difficile
was transferred to the newly created genus
Clostridioides
of the family
Peptostreptococcaceae
and was given the name
Clostridioides difficile
.
Clostridium mangenotii
was transferred to the same genus .
Species Clostridium litorale
moved to the genus
Peptoclostridium
of the same family
Peptostreptococcaceae
and renamed
Peptoclostridium litorale.
Species Clostridium sticklandii
moved to the genus
Acetoanaerobium
of the family
Peptostreptococcaceae
and renamed
Acetoanaerobium sticklandii
.
Species Clostridium dakarense
moved to the genus
Romboutsia
of the family
Peptostreptococcaceae.
Clostridium hiranonis, Clostridium paradoxum,
and
Clostridium thermoalcaliphilum
, their modern names: [
Clostridium
]
hiranonis
, [
Clostridium
]
paradoxum
and [
Clostridium
]
thermoalcaliphilum
, transferred to the family
Peptostreptococcaceae
without specifying a genus.
Species Clostridium histolyticum
was moved to the genus
Hathewaya
of the family
Clostridiaceae
and given the name
Hathewaya histolytica.
Clostridium limosum
and
Clostridium proteolyticum
were transferred to the same genus with the name changed to
Hathewaya limosa
and
Hathewaya proteolytica
, respectively.
Species Clostridium ramosum
moved to the genus
Erysipelatoclostridium
, family
Erysipelotrichaceae
, order
Erysipelotrichales
, class
Erysipelotrichia
and given the name
Erysipelatoclostridium ramosum
.
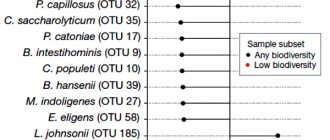
Species Clostridium aerotolerans, Clostridium aldenense, Clostridium algidixylanolyticum, Clostridium aminophilum, Clostridium amygdalinum, Clostridium asparagiforme, Clostridium bolteae, Clostridium celerecrescens, Clostridium citroniae, Clostridium clostridioforme, Clostridium fimetarium, Clostridium glycyrrhizinily ticum, Clostridium herbivorans, Clostridium hylemonae, Clostridium indolis, Clostridium lavalense, Clostridium methoxybenzovorans, Clostridium polysaccharolyticum, Clostridium populeti, Clostridium saccharolyticum, Clostridium scindens, Clostridium sphenoides, Clostridium symbiosum, Clostridium xylanolyticum
were transferred to the genus
Lachnoclostridium
of the family
Lachnospiraceae
and they are currently called [
Clostridium
]
aerotolerans
, [
Clostridium
]
aldenense
, [
Clostridium
]
algidixylanolyticum
, [
Clostridium
]
aminophilum
, [
Clostridium
]
amygdalinum
, [
Clostridium
]
asparagiforme
, [
Clostridium
]
bolteae
, [
Clostridium
]
celerecrescens
, [
Clostridium
]
citroniae
, [
Clostridium
]
clostridioforme
, [
Clostridium
]
fimetarium
, [
Clostridium
]
glycyrrhizinilyticum
, [
Clostridium
]
herbivorans
, [
Clostridium
]
hylemonae
, [
Clostridium
]
indolis
, [
Clostridium
]
lavalense
, [
Clostridium
]
methoxyben zovorans
,
Lachnoclostridium phytofermentans
, [
Clostridium
]
polysaccharolyticum
, [
Clostridium
]
populeti
, [
Clostridium
]
saccharolyticum
, [
Clostridium
]
scindens
, [
Clostridium
]
sphenoides
, [
Clostridium
]
symbiosum
, [
Clostridium
]
xylanolyticum
, respectively.
Eubacterium moniliforme species
and
Eubacterium tarantellae
are transferred from the genus
Eubacterium
and named
Clostridium moniliforme
and
Clostridium tarantellae
.
On the website GastroScan.ru in the “Literature” section there is a subsection “Microflora, microbiocenosis, dysbiosis (dysbacteriosis)”, containing articles addressing the problems of microbiocenosis and dysbiosis of the human gastrointestinal tract. Back to section
References
- Ivashkin V.T., Yushchuk N.D., Maev I.V., Lapina T.L., Poluektova E.A., Shifrin O.S., Tertychny A.S., Trukhmanov A.S., Sheptulin A. O.A., Baranskaya E.K., Lyashenko O.S., Ivashkin K.V. Recommendations of the Russian Gastroenterological Association for the diagnosis and treatment of Clostridium difficile-associated disease. Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2016
- Shelygin Yu.A. et al. Clinical guidelines for the diagnosis, treatment and prevention of Clostridium difficile-associated diarrhea. Clinical recommendations. — Moscow, 2021.
- Hassoun Ali. Clostridium difficile associated disease BMJ 2018
Who should be tested for C difficile infection?
In the work of Kwon et al. A study was conducted to determine the presence of infection in hospitalized patients. Initially, patients were divided into several groups according to the likelihood of a positive test based on clinical, laboratory and radiological data. C difficile was determined in stool using toxigenic culture or enzyme-linked immunosorbent assay.
- The results showed that 9 of 111 patients were diagnosed with clostridial infection by toxigenic culture and 4 by ELISA. The majority of patients (65%) had a low likelihood of infection before stool testing, while 31% had a moderate likelihood and 5% had a high likelihood.
- It is interesting to note that 9 patients with a positive ELISA result had a low likelihood of infection before the test.
These results highlight the importance of selecting patients for testing for clostridial infection. Signs and symptoms of infection must be carefully assessed and whether there is an alternative explanation for the diarrhea.