- home
- Useful
- CYSTITIS IN WOMEN
Cystitis is an inflammation of the bladder. Women suffer from it more often. Cystitis occurs as a result of pathogenic flora entering the urethra and the proliferation of bacteria in the bladder. Depending on the course, it can be acute or chronic. Acute cystitis appears suddenly, soon after exposure to unfavorable factors. The chronic form is characterized by a long course, the symptoms either worsen or subside. This type of pathology occurs as a complication of other genitourinary diseases.
Symptoms
The first signs that should alert you:
- the urge to urinate more often than usual;
- discomfort, feeling of bladder distension;
- lower abdominal pain;
- burning and stinging during and after visiting the restroom;
- change in color, impurities in the urine (blood, mucus).
With a longer course, persistent signs of general intoxication appear: chills, weakness and fatigue, fever, headache, sweating. The disease, in addition to the mucous membrane of the bladder, can affect the muscle layer. In this case, there is a constant feeling of heaviness and fullness in the lower abdomen, and urinary incontinence.
Cystitis after sexual intercourse
Inflammation sometimes develops as a result of certain genitourinary infections or after unprotected sexual contact. There is such a thing as “honeymoon cystitis,” or defloration cystitis. This is the development of an acute form of the disease due to the onset of sexual activity in a woman. The female urethra is much wider and shorter than that of men. A partner may be a carrier of pathogenic bacteria and not feel any symptoms. When you have sexual intercourse for the first time, a set of new bacteria enters the urethra. Together with them, an infection can enter the body, causing disease.
It is worth noting that the risk of bladder inflammation after sex exists for all women, regardless of whether they had sexual intercourse for the first time or not.
What does blood in urine mean?
This symptom is a direct reason to immediately consult a doctor. Cystitis with blood is called hemorrhagic. This is the most severe form, most often associated with an adenovirus infection. With the hemorrhagic type of the disease, patients suffer from severe abdominal pain extending to the perineum. Urination is frequent and painful. Body temperature is elevated, general intoxication is rapidly increasing.
Blood in the urine appears due to damage to the vessels located near the bladder. The infection can enter the bloodstream and quickly spread throughout the body. Frequent complications after hemorrhagic cystitis are pyelonephritis and other kidney inflammations.
This form can also change from acute to chronic with periods of remission. But it is best not to delay the process, but to immediately consult a doctor and treat the disease at the first manifestations.
Cystitis during menstruation
Manifestations of an acute form or exacerbation of a chronic form often occur in women during menstruation. This is due to the fact that bacteria enter the urethra along with the blood.
An exacerbation at the beginning of the cycle can be provoked by:
- inflammatory processes in the pelvic organs;
- hormonal changes in the body;
- thrush and other infections;
- venereal diseases;
- decreased immunity (including local);
- failure to comply with hygiene rules;
- allergies to pads, tampons.
During menstruation, cystitis is manifested by severe abdominal pain, which the patient may confuse with menstrual pain. Against the background of inflammation, cycle disruptions and delays may occur. This is due to the influence of the inflammatory process on the woman’s body.
Important! Pain in the lower abdomen, delayed menstruation and frequent urge to urinate may not be signs of cystitis, but of pregnancy. Therefore, if such symptoms occur, you should not self-medicate. You need to see a doctor immediately.
Pregnancy and cystitis
This disease is the most common among urological problems to which expectant mothers are susceptible. Due to pregnancy, immunity decreases, which means there is a greater risk of bladder inflammation.
While expecting a child, the risk is higher for a number of other reasons.
- Due to the enlargement of the uterus, the ureters may be compressed. As a result, the outflow of urine from the kidneys is disrupted and stagnation occurs.
- During pregnancy, many old ailments return, being in a state of stable remission. Especially pathologies of the genitourinary system.
Risk to maternal and fetal health:
- High risk of complications, such as pyelonephritis.
- Fetal weight deficiency, anemia, arterial hypertension.
- Risk of premature birth and fetal death in utero.
Why does cystitis occur?
The main reason is the penetration of bacteria, viruses, fungi and other pathogenic microorganisms into the bladder cavity.
The most common infectious agents:
- Streptococcus.
- Escherichia coli.
- Staphylococcus.
Cystitis can also be caused by the following factors:
- taking certain medications (for example, cyclophosphamide);
- decreased immunity and hormonal imbalances;
- ionizing radiation in the treatment of cancer;
- allergy;
- invasive interventions, foreign body in the urethra (for example, catheter);
- aggressive chemicals in personal care products;
- stones in the bladder and other pathologies of the genitourinary system;
- spinal injuries;
- local or general hypothermia;
- stagnation of urine in the bladder;
- lack of physical activity;
- unhealthy eating habits, abuse of spicy foods;
- pregnancy and childbirth;
- neglect of personal hygiene rules;
- tight underwear made of synthetic materials, clothing that restricts movement;
- sexual infections.
Predisposing factors
Predisposing factors for the development of cystitis are:
- anatomical and physiological characteristics of the female body, changes in the location of the urethra;
- overly active sex life;
- new sexual partner, frequent change of sexual partners;
- use of spermicides;
- an episode of urinary tract infection (UTI) in childhood;
- history of maternal urinary tract infections.
The causative agent of acute cystitis in 70-95% of cases is E. coli - Escherichia coli. Other pathogens, such as staphylococcus, Klebsiella, Proteus, are much less common.
What is the difference between acute and chronic cystitis
The acute course of the disease begins with severe pain in the lower abdomen, frequent intense urge to urinate, many of which are ineffective. If the bladder is emptied, it is accompanied by cutting pain and itching. The acute course of the disease always causes severe discomfort, which literally forces you to see a doctor.
In this condition, there is a quantitative and qualitative change in the patient’s urine: at first there may be a lot of it, and then the volume of urine excreted greatly decreases. As the disease progresses, the color of the liquid becomes darker, it becomes less transparent, and impurities of pus and blood appear. A typical symptom of acute cystitis is urinary leakage or incontinence.
Chronic cystitis is a condition even more dangerous than acute one. With a long course of the disease, the epithelial cells of the bladder change and cysts form, which increases the risk of cancer problems. Signs of a chronic illness may wax and wane over time: pain in the lower abdomen and when urinating, a feeling of fullness, frequent trips to the toilet, aching pain in the lower back, etc. When the disease goes into remission, patients do not consider it necessary to continue treatment. During an exacerbation, many do not consult a doctor using “proven” treatment methods. Chronic cystitis may be a consequence of incompletely cured acute cystitis.
Many patients suffer for years from alternating remissions and exacerbations. But with the correct selection of therapy and compliance with the treatment regimen, the symptoms quickly disappear, and the disease can be cured completely.
After an episode of acute cystitis. Preventive measures
After adequate treatment of acute cystitis, there is no need for additional examinations. Sufficient fluid intake, avoidance of hypothermia, personal hygiene, sexual hygiene, timely treatment of gynecological diseases and sexually transmitted infections are recommended. Prophylactic use of any drugs after a single episode of acute cystitis is not indicated.
If symptoms of cystitis occur within two weeks after treatment, in the absence of a therapeutic effect, a urine culture test should be performed to determine the sensitivity of the isolated pathogens to antibiotics (urine culture). Based on the results of bacteriological culture, it is recommended to prescribe an antibacterial drug according to the sensitivity of the pathogen to it.
Is it possible to go to the sauna or lie in a hot bath if you have cystitis?
No. Overheating the body and in particular the pelvic organs during the acute phase of this disease is strictly contraindicated. If the disease is bacterial in nature, a bath or hot bath will lead to the proliferation of the pathogenic environment, the release of pus, and the appearance of internal abscesses. If the disease is viral or other in nature, overheating will accelerate microcirculation, which will increase inflammation and can cause blood to appear in the urine. It is not worth heating the body during this disease, so as not to provoke severe fever and increased pain.
After the disease has been successfully cured with the help of drugs or during a period of stable remission, the bath is not dangerous, but, on the contrary, can be beneficial for the patient’s health. Visiting a bathhouse or sauna has a restorative effect on the body:
- removes toxins;
- increases immunity;
- relieves stress, promotes relaxation;
- activates the functioning of the kidneys and bladder, removes excess fluid from the body.
This effect can be an excellent prevention of cystitis and other inflammatory processes. The main condition is to visit the bathhouse only in the stage of remission, without trying to “cure” the disease with its help.
Diagnostics
The diagnosis of acute cystitis is established based on the patient’s complaints. To clarify the diagnosis, a general urine test is used, ideally a urine test with test strips (not common in Russia).
Prescribing treatment for acute cystitis is also possible only on the basis of the patient’s complaints (so-called empirical therapy), without obtaining the results of a urine test. Taking urine for culture (bacteriological examination) is not mandatory in patients with uncomplicated cystitis. Urine culture is necessary only in a number of cases, such as: pregnancy, suspected acute pyelonephritis, prolonged course of cystitis (more than 2 weeks), atypical course of the disease. If there are more than 10³ bacteria in the urine culture, the diagnosis of acute cystitis can be microbiologically confirmed.
Ultrasound or other imaging techniques are not part of the diagnostic algorithm for acute cystitis. A specific picture according to ultrasound of the bladder may not be observed. Ultrasound signs such as “thickening of the bladder wall” and “presence of bladder suspension” do not necessarily indicate inflammation of the bladder mucosa. Most often, the purpose of ultrasound is to exclude bladder tumors and ureteral stones.
Performing cystoscopy in acute cystitis is contraindicated.
Differential diagnosis
Vaginitis . Characterized by increased urination associated with vaginal irritation. It appears as an erased, sluggish course. Predisposing factors may include excessive sexual activity and frequent changes of sexual partners (new sexual partner). There is usually no blood in the urine, pain when urinating, or pain in the lower abdomen. Upon examination, you can detect vaginal discharge, which, when examined, reveals an inflammatory process.
Urethritis . This disease is also characterized by frequent, painful urination, but the severity of symptoms is usually milder than with acute cystitis. The most common causes of urethritis are gonorrhea, trichomoniasis, chlamydia and herpes simplex virus. The disease can also occur due to a change in sexual partner. Discharge from the urethra is more common in men.
Which doctor should I see and what tests should I take?
A urologist diagnoses and treats this disease. The specialist knows how to assess the patient’s condition, as well as what treatment regimen to choose in order to relieve inflammation and not cause harm to health. Self-medication and, even more so, ignoring symptoms can lead to a serious deterioration of the situation and significant consequences: the transition of the acute stage to the chronic stage, the development of kidney inflammation, the proliferation of cysts, etc.
Therefore, if any of the listed signs appear, you should immediately contact a urologist. The doctor conducts an examination, makes an accurate diagnosis and selects appropriate therapy.
To confirm cystitis, the doctor will prescribe:
- general urine analysis;
- analysis according to Nechiporenko;
- bacteriological examination;
- cystoscopy;
- Ultrasound of the abdominal cavity, kidneys and bladder.
Urine tests can reveal which pathogenic organism caused the disease. This means choosing the right treatment. It is also very important to track the presence and amount of protein in urine. This may be a sign of kidney dysfunction.
Cystoscopy is an invasive endoscopic examination of the bladder cavity. The cystoscope consists of a metal tube with a video camera at the end, which is inserted into the bladder through the urethra, as well as a set of miniature instruments. With its help, the mucous membrane is examined, a tissue sample is taken for histology, and polyps are removed.
Ultrasound examination allows you to assess the condition of organs and adjacent tissues.
The cost of seeing a doctor and diagnostic tests for cystitis depends on the choice of clinic, the patient’s condition, medical history and other factors. This information is clarified when making an appointment with a specialist or on the medical institution’s website.
Treatment of cystitis
The treatment plan for the patient is drawn up by a urologist. Cystitis is usually treated on an outpatient basis. Hospitalization is resorted to only in severe cases: severe intoxication, pregnancy, spread of the inflammatory process to the kidneys and other complications.
When treating cystitis, experts advise following several important rules:
- bed or semi-bed rest;
- taking medications strictly as prescribed by the doctor;
- compliance with relapse prevention measures.
How to help yourself at home
When the first signs of inflammation appear, before consulting a doctor, the patient can take some measures to alleviate her condition and relieve severe pain.
- You can drink a warm solution of baking soda (dosage – 2 teaspoons per glass of water). This composition alkalinizes urine, relieves burning sensation, and soothes pain in the bladder.
- Cranberry juice also helps with pain.
- In general, with cystitis you need to drink at least 2 liters of fluid per day. Proper diuresis allows you to quickly remove bacteria from the bladder, preventing them from multiplying.
- You need to give up coffee and alcohol, as well as drinks that increase the acidity of urine: grape, orange, pineapple juice.
- The body must be kept warm, protected from drafts, and not walk barefoot on the cold floor.
- Avoid physical exercise. Do not swim in ponds or pools under any circumstances!
All of these methods are suitable for alleviating the condition and relieving severe pain before visiting a doctor. But it is impossible to cure the disease with their help. Only a doctor can prescribe therapy that will help cope with the disease forever.
Drugs for the treatment of cystitis
To get rid of this disease in acute and chronic forms, antibiotics, anti-inflammatory, immunomodulatory and painkillers are used. Antibacterial tablets, selected by a specialist taking into account test results, provide a quick and lasting therapeutic effect.
Among the most common medications in tablets used to treat cystitis:
Furadonin.
A drug from a series of nitrofurans for the treatment of genitourinary infections. Active against most microorganisms (gram-positive and gram-negative). Resistance to it often develops. The drug is used in the treatment and prevention of infections, including after invasive examinations of the urethra and bladder. Dosage for adults: 100-150 mg 3-4 times a day after meals, with plenty of liquid.
Nitroxoline.
The drug contains 8-hydroxyquinoline derivatives. The tablets cope with most gram-positive and gram-negative microbes and some fungi. Effective against candida. Prescribed for cystitis, urethritis, pyelonephritis. Adults: 100 mg 4 times a day with meals.
Cyston.
Antimicrobial, anti-inflammatory, analgesic drug of plant origin. Has a pronounced diuretic property. Prevents stone formation in the urinary tract. Dosage for adults: 2 tablets twice a day.
Furagin.
A drug with antibacterial properties based on nitrofuran. It has high activity against various gram-positive and gram-negative bacteria. It is actively used to treat all types of infectious and inflammatory diseases of the urinary tract, as well as complications after operations. Dosage - 100 mg 3 times a day.
Furazolidone.
Antimicrobial drug based on nitrofurans. Active against most microbes, resistance to it develops slowly. It is used to treat colpitis, urethritis, dysentery and other diseases. Take 100 mg 4 times a day, after meals, with plenty of water.
Levomycetin.
A broad-spectrum bacteriostatic antibiotic, effective even against bacteria resistant to penicillin and tetracycline. Used to treat various infections, including urinary tract infections. Dosage for adults: 200-400 mg, 3 times a day, half an hour before meals.
Norbactin.
An antibacterial drug that belongs to the group of fluoroquinolones. Has a pronounced bactericidal effect against a wide range of microorganisms. It is actively used to treat genital infections and urinary tract diseases. Dosage for adults: 400 mg 2 times a day.
Tsiprolet.
Antimicrobial drug from the group of fluoroquinolones. It has a rapid bactericidal effect on many gram-positive and gram-negative organisms. Effectively helps with infections of all types, including those affecting the kidneys and genitourinary system. Adults are prescribed 100–200 mg 2 times a day, regardless of meals.
Biseptol.
Combined antimicrobial drug. The tablets contain sulfamethoxazole and trimethoprim. Active against most microorganisms. It is good for infections of various types, including those affecting the kidneys and urinary tract. The dosage of the drug is calculated depending on the patient’s weight. It should be taken after meals with plenty of liquid.
Flemoxin solutab.
The active ingredient is amoxicillin. Broad-spectrum antibiotic from the group of semisynthetic penicillins. Active against most bacteria that cause infections of the genitourinary system. Dosage: 500–700 mg 2 times a day, regardless of meals.
Trichopolum.
A derivative of 5-nitromidazole, an antiprotozoal drug with a pronounced antibacterial effect. In combination with amoxicillin and independently used in the treatment of diseases of the genitourinary system and other infections. Take 250 mg 3 times a day with meals.
Canephron.
A herbal remedy that is used to treat and prevent exacerbations of cystitis. Eliminates or reduces the intensity of pain in the urethra, relieves inflammation. Dosage: 2 tablets 3 times a day with meals.
Hemorrhagic cystitis in women: diagnosis and treatment
17.08.2021
2215
0
Team of authors:
- L.A. Sinyakova – Doctor of Medical Sciences, Professor of the Department of Urology and Surgical Andrology of the Russian Medical Academy of Postgraduate Education, urologist of the State Budgetary Healthcare Institution City Clinical Hospital named after. S.P. Botkin DZM; Moscow, Russia; RSCI Author ID 735597
- ABOUT. Laurent - Academician of the Russian Academy of Sciences, Professor, Doctor of Medical Sciences, Head of the Department of Urology and Surgical Andrology of the Russian Medical Academy of Postgraduate Education, urologist of the State Budgetary Healthcare Institution of the State Clinical Hospital named after. S.P. Botkin DZM; Moscow, Russia; RSCI Author ID 370312
- I.V. Kosova – Candidate of Medical Sciences, urologist, State Budgetary Healthcare Institution “City Clinical Hospital named after. V.P. Demikhova DZM"; Moscow, Russia
- D.N. Kolbasov – Candidate of Medical Sciences, Head of the Urology Department of the State Budgetary Institution “City Clinical Hospital named after. V.P. Demikhova DZM"; Moscow, Russia
- ME AND. Nezovibatko – urologist, State Budgetary Institution “City Clinical Hospital No. 29 named after. N.E. Bauman"; Moscow, Russia
Treatment of urinary tract infections (UTIs) is often challenging, in most cases due to the difficulty of diagnosing the causes of UTIs and identifying risk factors that lead to persistent recurrence of the disease. At the first visit, the doctor cannot answer the question: is this episode of infection an uncomplicated UTI? After all, only by examining the patient can the cause of the development of dysuria, pain over the pubis, gross hematuria, etc. be established. and prescribe therapy according to accepted recommendations. Only this approach will avoid the uncontrolled use of antimicrobial drugs, including fluoroquinolones, the development of antibiotic resistance, the transition of infection to a chronic form, and disruption of the normal biocenosis of the intestine and vagina.
Bacteria of the Enterobacterales family are the most common etiological agent for the development of UTIs, but in some cases no bacterial agent can be identified, and the main clinical sign, along with dysuria, is gross hematuria [1, 2]. Currently, increasing attention is being paid to the influence of viral infections on the development of UTIs in both adults and children [3–9]. The phenomenon of viruria is also quite actively discussed in the literature [3–12]. According to various authors, viruses from the group of herpes viruses, papillomaviruses, and adenoviruses can cause the development of persistent dysuria [5, 13]. It should be noted that herpes viruses: herpes simplex virus (HSV) types 1 and 2, cytomegalovirus (CMV), Epstein–Barr virus (EBV) can cause secondary immunosuppression and aggravate the course of bacterial infection, leading to the development of relapses [11, 12, 14]. Taking antimicrobial drugs in the presence of a viral component further aggravates the process by suppressing normal flora.
Purpose: to study the causes of hemorrhagic cystitis, develop an algorithm for examining these patients, and also select rational therapy.
Materials and methods
To the urology department of the State Budgetary Healthcare Institution “GKB named after. V.P. Demikhova Department of Health Care" in 2019, 61 patients with a clinical picture of acute hemorrhagic cystitis were hospitalized at the age of 18 to 89 years (average age was 55.56 ± 21.82). This represents 59.2% of all patients hospitalized in the department for inflammatory diseases of the lower urinary tract. Patients underwent a standard examination: general urinalysis, urine culture for flora and sensitivity to antibiotics, ultrasound examination of the kidneys and bladder, and cystoscopy as indicated.
Taking into account the high frequency of viral infections as an etiological factor in the development of hemorrhagic cystitis, on the basis of the Department of Urology and Surgical Andrology of the Russian Medical Academy of Postgraduate Education, an algorithm for examining this category of patients was developed, additionally including the method of polymerase chain reaction (PCR) of the first portion of urine (scraping from the urethra) on presence of HSV types 1 and 2, CMV, EBV during an exacerbation, enzyme-linked immunosorbent assay (ELISA) with determination of immunoglobulins G and M to HSV types 1 and 2, CMV and EBV, culture of vaginal discharge for flora and sensitivity to antibiotics with mandatory indication of quantity lactobacilli
According to this algorithm, 214 patients were examined on the basis of the Department of Urology and Surgical Andrology of the Russian Medical Academy of Postgraduate Education of the Ministry of Health of the Russian Federation, of which 154 (72%) patients were aged from 18 to 44 years.
results
During the examination of 61 patients in the urology department of the State Budgetary Institution "City Clinical Hospital named after. V.P. Demikhov DZM" revealed that an overdose of anticoagulants in elderly patients with a burdened cardiological, neurological history (atrial fibrillation, chronic cerebral ischemia, acute cerebrovascular accident, etc.) as a cause of the development of gross hematuria and dysuric phenomena occurred in 18% of cases (11 patients). Post-radiation cystitis (radiation therapy for cervical cancer in 2 cases and vaginal cancer in 1 patient) occurred in three patients. He performed transurethral resection of the bladder wall and coagulation of bleeding vessels). In two cases, there was a history of a bladder tumor, but tumor recurrence was not confirmed histologically. In other cases, the patients became acutely ill and, due to severe dysuria and gross hematuria, were hospitalized in the urology department (Fig. 1).
Rice. 1. Data from bacteriological urine analysis
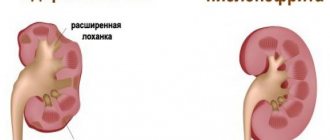
The absence of leukocyturia and bacteriuria, the presence of micro- or macrohematuria, sterile urine cultures, changes characteristic of viral damage to the bladder wall in the form of multiple petechial hemorrhages, which we identified during cystoscopy, allowed us to assume a viral etiology of the disease (Fig. 2).
Rice. 2. Cystoscopic picture of hemorrhagic cystitis. Multiple petechial hemorrhages
And thus, the proportion of hemorrhagic cystitis of presumably viral etiology, viral urethritis in the structure of inflammatory diseases of the lower urinary tract increases, which dictates the need to create
Patients with hemorrhagic cystitis do not require hospitalization, but the presence of hematuria is concerning and, as a rule, they insist on hospitalization to exclude a tumor process.
And thus, the proportion of hemorrhagic cystitis of presumably viral etiology, viral urethritis in the structure of inflammatory diseases of the lower urinary tract is increasing, which dictates the need to create a potentially new algorithm for examining this category of patients and etiologically based therapy.
A similar algorithm was developed on the basis of the Department of Urology and Surgical Andrology of the State Budgetary Educational Institution of Further Professional Education of the Russian Medical Academy of Postgraduate Education of the Ministry of Health of the Russian Federation (Table 1).
Table 1. Algorithm for diagnosing recurrent (hemorrhagic) cystitis
| CAREFULLY COLLECTED HISTORY! With the identification of such risk factors as early onset of sexual activity, frequent change of sexual partners, the presence of invasive manipulations, concomitant chronic gynecological diseases, vaginal dysbiosis. The presence of viral infections (labial and genital herpes, CMV, EBV, human papillomavirus (HPV) of both high and low oncogenic risk) in the patient and her sexual partners. Presence of cervical erosion associated with HPV and/or epithelial dysplasia (CIN) grade II–III, HPV(+) |
| Vaginal examination with O'Donnell test |
| General urine analysis |
| Urine culture, vaginal discharge culture for flora and sensitivity to antibiotics with mandatory indication of the number of lactobacilli! |
| Screening for the presence of sexually transmitted infections (STIs), including viral infections (HSV types 1 and 2, CMV, EBV, high oncogenic risk HPV) ELISA to test antiviral antibodies to these viruses |
| Ultrasound examination of the kidneys, bladder with determination of residual urine, pelvic organs with Doppler sonography |
| Cystoscopy with biopsy |
| Examination by a gynecologist |
The presence of chronic latent herpesvirus infection (CHVI) was detected in 83 (37%) of 214 examined patients at the Department of Urology and Surgical Andrology, which was confirmed by anamnesis data, ELISA results with an increase in the level of immunoglobulin G tens and hundreds of times. The level of antibodies to HSV types 1 and 2 in patients with hemorrhagic cystitis without leukocyturia and sterile bacteriological urine culture was significantly higher than in patients with hemorrhagic cystitis and an identified pathogen by 2.6 times (p < 0.05). Such an increase in the levels of antiviral antibodies does not indicate carriage, but the presence of CHVI.
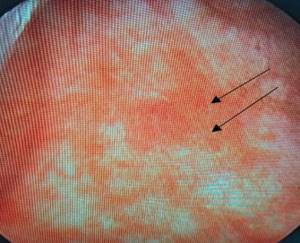
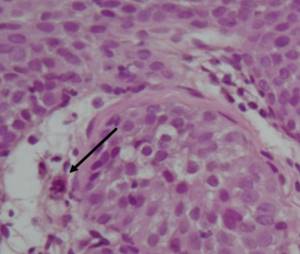
Rice. 3. A fragment of a bladder biopsy with signs of a pronounced inflammatory infiltrate, with a predominance of lymphocytes (L), signs of intracellular infection: koilocytosis (K), intranuclear inclusions (indicated by arrows). Hematoxylin-eosin UV staining. 40 x 0.65
There may be an increase in antibodies not only to HSV and types 2, but also to other herpes viruses: CMV (clinical example 1) and EBV (clinical example 2).
A combined herpes-viral infection in the form of a mixed infection of HSV types 1 and 2 and CMV was detected in 66.3% of cases, in the rest, EBV was additionally detected.
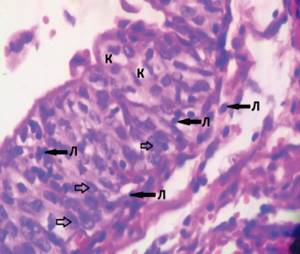
Cystoscopy with biopsy of the bladder mucosa was performed in 32 patients. The morphological features of viral hemorrhagic cystitis are koilocytosis, detected in 29 (90%) patients (Fig. 3) and cell changes of the “mulberry” type were noted in 18 (50.2%) patients (Fig. 4).
Rice. 4. A fragment of a bladder biopsy with signs of a pronounced inflammatory infiltrate, the presence of cell changes of the “mulberry” type. Env. hematoxylin-eosin. Magnification 10 x 10
The clinical examples below show the effectiveness of the algorithm we developed.
Clinical example 1.
Patient D., 33 years old. For 3 years he has been suffering from recurrent cystitis, periodically mixed with blood. During the inter-relapse period, burning, pain, discomfort in the urethra, severe asthenia, and dyspareunia are a concern. It should be noted that the symptoms intensified during ARVI, which, in our opinion, is one of the pathognomonic signs of the viral etiology of cystitis. She repeatedly received courses of antimicrobial therapy (levofloxacin, furazidin, suprax, fosfomycin trometamol) with a partial positive effect. Bacteriuria and leukocyturia were not detected. Suffers from labial herpes (relapses approximately 1-2 times a year). According to ELISA data, an increase in the level of antiviral antibodies to CMV was detected: IgG to HSV types 1 and 2 9.7 ind.pos., anti-CMV IgG - 228.7 units/ml (positive - more than 6 units/ml), anti-EBV IgG- EBNA – 15.5 units/ml, anti-EBV IgG-VCA – 21.2 units/ml. The patient was prescribed long-term suppressive antiviral therapy with a positive effect. After 6 months, the level of antibodies to CMV decreased to 8.5 units/ml.
Clinical example 2.
Patient B., 56 years old. Postmenopause. He has been suffering from genital herpes for 20 years. Recently there have been exacerbations 2-3 times a year. Hemorrhagic cystitis for the last 2 years; during the inter-relapse period, discomfort and burning sensation when urinating are bothersome. There is no leukocyturia, no bacteriuria, and no viral damage was detected in scrapings from the urethra taken outside of an exacerbation. Therefore, it is very important to conduct an examination in the acute period (performing PCR of the first portion of urine and/or taking scrapings from the urethra). Cystoscopy picture of hemorrhagic cystitis. However, a pronounced increase in the level of antiviral antibodies to HSV types 1 and 2, CMV, EBV was detected: anti-HSV type 1 IgG - 222 units/ml, anti-HSV type 2 IgG - 3 units/ml (more than 22 units/ml - positive) , anti-CMV IgG – 407.8 units/ml (positive – more than 1 unit/ml), anti-EBV IgG-EBNA – 196 units/ml (more than 20 units/ml – positive), anti-EBV IgG-VCA – 505 units /ml (more than 20 units/ml – positive). Long-term antiviral therapy was prescribed with a positive effect.
Clinical example 3.
Patient Kh., 26 years old, was urgently hospitalized at the City Clinical Hospital named after. S.P. Botkin with complaints of blood in the urine with clots, frequent and painful urination, pain at the end of urination, burning in the external genital area. The above complaints bother me throughout the day. She did not seek medical help. She did not treat herself.
The patient has a history of recurrent cystitis for three years. Exacerbations occurred three times in the last 6 months. Treatment and examination took place on an outpatient basis with a urologist. In a general clinical analysis of urine, leukocytes were determined up to 10 per field of view, erythrocytes up to 2 per field of view. All bacteriological urine cultures were sterile. Courses of antibacterial therapy (fosfomycin, fluoroquinolones, nitrofurans) and anti-inflammatory therapy (diclofenac) were carried out with a slight temporary effect. At the same time, the burning sensation in the urethral area persisted. According to the gynecological history: menstruation since the age of 13, regular, heavy, painful. The patient has no pregnancies or gynecological diseases. Sexual life from the age of 18. Barrier contraception. She has not been sexually active for the last 6 months due to dyspareunia.
When examined in the emergency department, in a general urine test, red blood cells cover all fields of view. According to ultrasound examination of the urinary system, no stones, space-occupying formations, or urodynamic disturbances were detected. The bladder has a clear, even contour, without parietal formations. There is no residual urine. Survey urography revealed no shadows suspicious for stones. Upon admission to the emergency department, she was examined by a gynecologist: there was no evidence of acute gynecological pathology at the time of examination.
The patient was hospitalized in the urology department of the State Budgetary Healthcare Institution of the City Clinical Hospital named after. S.P. Botkin DZM with a preliminary diagnosis: acute hemorrhagic cystitis. The department collected urine for bacteriological culture and cytological examination to identify atypical cells. Antibacterial (ciprofloxacin), hemostatic (etamzilate), and anti-inflammatory (diclofenac) therapy was prescribed. On the 3rd day of hospitalization, positive dynamics were noted in the form of relief of hematuria and a decrease in dysuric phenomena. The result of a bacteriological analysis of urine - no growth of microflora was detected; atypical cells were not detected in all three portions of urine.
Due to persistent discomfort in the urethral area, the patient was examined in a gynecological chair. When examined in the area of the outer labia, multiple vesicular elements of a polycyclic scalloped shape with transparent contents, characteristic of herpes, are determined.
A detailed history collection made it possible to find out that the patient had been bothered by labial herpes for three years; over the last 6 months, relapses of herpes had become more frequent. She was treated independently with topical acyclovir.
The patient was discharged with a final clinical diagnosis: acute hemorrhagic cystitis. Genital herpes. Recommendations for further examination are given. A urogenital smear of three loci (urethra, cervical canal, vagina) was performed on an outpatient basis. Qualitative real-time PCR analysis of scrapings of the urethral mucosa revealed HSV type 2. Enzyme-linked immunosorbent assay (ELISA) showed an increase in antibody titer (HSV 1 IgG - 144.3; HSV 2 IgG - 130.5). Urine real-time PCR revealed HSV types 1 and 2 (HSV 1.2 – 8.6 x 102).
The patient was sent to the herpetic center, where the previously established diagnosis was confirmed: genital herpes. Antiviral therapy was prescribed: Valacyclovir at a dosage of 500 mg 2 times a day for 5 days, then maintenance therapy 500 mg 1 time a day for 3 months.
After 2 weeks, cystoscopy with a punch biopsy was performed as planned. When examining the external genitalia, the vesicular rashes had residual traces. The cystoscopic picture had characteristic mucosal features. In the area of the orifices and the bladder triangle, whitish plaques were detected, somewhat similar to changes in the mucosa during leukoplakia.
A morphological study of biopsy specimens of the bladder wall taken during a pinch biopsy revealed the presence of koilocytosis and cell changes of the “mulberry” type as a pathognomonic sign of herpesvirus infection.
Subsequently, during follow-up during the year, the patient did not note relapses of herpesvirus infection and cystitis. The long-term absence of dysuria, dyspareunia and burning in the urethral area improved the quality of life, made it possible to return to sexual activity and give birth to a healthy child.
After additional examination and confirmation of the viral nature of the disease, all patients received antiviral therapy, which, in case of relapse of the disease, continued in a suppressive mode for 3 to 6 months. If a viral infection was a co-factor in the development of inflammatory and dysbiotic diseases of the urogenital tract, then in case of exacerbation of the disease, therapy began with symptomatic treatment - the use of a drug that has a local analgesic effect and alleviates the symptoms of dysuria, then, according to the recommendations for the treatment of acute cystitis, the use of fosfomycin trometamol or nitrofuran drugs. When combined with inflammatory gynecological diseases, local antimicrobial therapy was used. If the bacterial pathogen was known, antimicrobial therapy was prescribed according to urine culture. The use of the specified algorithm for the diagnosis and treatment of recurrent lower urinary tract infections in women made it possible to establish the viral nature of the disease, as well as increase the relapse-free period from 6 to 12 months, improve the quality of life of patients, relieving them of the symptoms of urethritis, dyspareunia, and most importantly, exclude a tumor of the urinary tract bladder, as a cause of gross hematuria, that is, contributed to the solution of a social and demographic problem.
Discussion
In clinical practice, we are increasingly encountering patients with repeated relapses of cystitis, in whom the use of antibacterial drugs leads to temporary improvement or does not help at all. In contrast to typical predisposing factors for bacterial cystitis, such as sexual intercourse and hypothermia, in this category of patients an exacerbation most often occurs against the background of stressful situations, after a climate change and is often accompanied by gross hematuria. Viral cystitis and/or urethritis most often affects young women with various concomitant inflammatory diseases and problems with immunity. In addition, symptoms of urethritis are also present during the inter-relapse period. Repeated, often unjustified courses of antibacterial therapy contribute to the development of vaginal dysbiosis and dysbacteriosis, which also aggravates the severity of the problem. The presence of dyspareunia forces patients to refuse sexual activity, which makes the problem not only medical, but also social, as it leads to impaired childbearing.
To date, data on the role of viruses in the development of urological diseases are extremely scattered, mosaic and not systematized [5]. The presence of koilocytes during a morphological study, as a manifestation of papillomavirus infection, is the most reliable sign of viral damage to the bladder wall, both according to our data and the literature [3–5]. As for herpesvirus infections, according to Russian researchers, HSV type 1 DNA was detected in urine and bladder biopsies in 7.1% of cases in patients suffering from chronic cystitis [15–16]. A. Ito et al. indicate the etiological role of HSV type 2 in the development of nongonococcal urethritis in men without visible herpetic eruptions [17]. According to the literature, the asymptomatic course of genital herpes is registered in 20% of cases, and atypical in 60% [18, 19]. In our study, a latent viral infection was detected in a third of patients; in most cases there was a mixed infection (HSV types 1 and 2, CMV, EBV), and therefore the use of traditional antimicrobial therapy is an ineffective method of treatment.
It should be noted that herpesvirus infections are a medical and social problem and require an integrated approach to the treatment of this category of patients, since herpes infections affect the reproductive health of both women and men. In the conclusion of key experts following the results of an interdisciplinary scientific meeting on the topic: “Diagnostics, treatment, prevention of virus-associated diseases: solutions” (Sochi, September 9, 2019) chaired by corresponding member. RAS, Doctor of Medical Sciences, Prof., V.E. Radzinsky noted that the role of viral infections (HPV, HSV, CMV) in “irretrievable” reproductive losses has been established; the risk of viral diseases (HPV, HSV, CMV) is higher in individuals with insufficient anti-infective protection; viral infections (HPV, HSV, CMV) evade the host’s innate immune response, in particular by suppressing the production of interferon, etc.[20].
conclusions
Thus, cystitis of viral etiology is currently a reality, which is confirmed by literature data. Given the frequency of relapses and the ineffectiveness of traditional therapy, a thorough examination of patients should include not only urine culture and testing for sexually transmitted infections, but also the use of methods to exclude or confirm the viral nature of the disease.
Literature
- Palagin I.S., Sukhorukova M.V., Dekhnich A.V., Eidelshtein M.V., Perepanova T.S., Kozlov R.S. and the DARMIS-2018 research group. Antibiotic resistance of pathogens of community-acquired urinary tract infections in Russia: results of the multicenter study "DARMIS2018". Clinical and Antimicrobial Therapeutics 2019;21(2):134-146. . https://doi.org/10.36488/cmac.2019.2.134-146.
- Perepanova T.S., Kozlov R.S., Rudnov V.A., Sinyakova L.A. et al. Federal clinical recommendations “Antimicrobial therapy and prevention of infections of the kidneys, urinary tract and male genital organs.” M:2020; With. 150. .
- Laurent O.B., Sinyakova L.A., Nezovibatko Ya.I. Hemorrhagic cystitis in women: epidemiology, etiology, pathogenesis, diagnosis. Consillium Medicum 2017;19(7):50-55.
- Ibishev Kh.S., Krakhotkin D.V., Vasiliev A.A., Krainy P.A. Recurrent lower urinary tract infection of viral etiology. Journal of Urology 2017;5(1):26-31. .
- Krakhotkin D.V., Ivanov S.N., Naboka Yu.L., Kogan M.I., Gudima I.A., Ilyash A.V. et al. Viral pathogens in urological diseases. Medical Bulletin of the South of Russia 2018;9(4):14-21. .
- Molochkov V.A., Semenova T.B., Kiselev V.I., Molochkov A.V. Genital viral infections. M.: BINOM Publishing House, 2009. 208 p. .
- Atilla E, Yalciner M, Atilla PA, Ates C, Bozdag SC, Yuksel MK, et al. Is cytomegalovirus a risk factor for haemorrhagic cystitis in allogeneic haematopoietic stem cell transplantation recipients? Antivir Ther 2018;23(8):647-653. https://doi.org/10.3851/IMP3252.
- Badawi H, Ahmed H, Aboul Fadl L, Helmi A, Fam N, Diab M, et. al. Herpes simplex virus type‐2 in Egyptian patients with bladder cancer or cystitis. APMIS 2010;118(1):37-44. https://doi.org/10.1111/j.1600-0463.2009.02556.x.
- Melekhina E.V., Chugunova O.L., Filippov A.V. To the question of the role of viruses in the formation of chronic infections of the urinary system. Russian Medical Journal 2013;2:27-30. [Melekhina EV, Chugunova OL, Filippov AV On the role of viruses in the formation of chronic infections of the urinary tract system. Rossiyskiy meditsinskiy zhurnal=Russian Medical Journal 2013;2:27-30. (In Russian)].
- Gourinat AC, O'Connor O, Calvez E, Goarant C, Dupont-Rouzeyrol M. Detection of Zika virus in urine. Emerg Infect Dis 2015;21(1):84–86. https://doi.org/10.3201/ eid2101.140894.
- Isakov V.A., Arkhipova E.I., Isakov D.V. Human herpesvirus infections. Guide for doctors. St. Petersburg:. SpetsLit, 2013. 2nd ed., revised. and additional 670 pp. .
- Isakov V.A., Arkhipova E.I., Isakov D.V. Human herpesvirus infections. Guide for doctors. St. Petersburg: SpetsLit, 2006. 303 p. .
- Derevianko T.I., Ryzhkov V.V. Viral infections: human papillomavirus and genital herpes types 1 and 2 as the cause of chronic recurrent cystitis with severe dysuric syndrome in women with hypospadias and urethral hypermobility. Urology 2015;4:29-33. .
- Kondratenko I.V. Blogov A.A. Primary immunodeficiencies. - M.: Publishing house MEDPRACTIKA-M, 2005. 232 pp. [Kondratenko VI Blogov A. Primary immunodeficiencies. M.: Publishing house of medical practice-M, 2005. P. 232. (In Russian)].
- Naboka Yu.L., Ilyash A.V., Krakhotkin D.V. Viral-bacterial associations verified in the urine of healthy people (pilot study). Journal of Urology 2018;6(3):44-49. . https://doi.org/10.21886/2308-6424-2018-6-3-44-49.
- Naboka Yu.L., Gudima I.A., Kogan M.I., Ibishev Kh.S., Chernitskaya M.L. Microbial spectrum of urine and bladder biopsies in women with chronic recurrent cystitis. Urology 2013;4:16-18. [Naboka YL, Gudima IA, Kogan MI, Ibishev HS, Chernitskaya ML Microbial spectrum of urine and bladder biopsies in women with chronic recurrent cystitis. Urologiya = Urology 2013;4:16-18. (In Russian)].
- Ito S, Yasuda M, Kondo H, Yamada Y, Nakane K, Mizutani K, et al. Clinical courses of herpes simplex virus-induced urethritis in men. J Infect Chemother 2017;23(10):717-719. https://doi.org/10.1016/j.jiac.2017.03.017
- Ashley RL, Wald A. Genital Herpes: Review of the Epidemic and Potential use of type-specific serology. Clinical microbiology reviews, Jan.1999. P.1-8.
- RODVK - “Federal clinical guidelines for the management of patients with herpes zoster”; Moscow, 2015. .
- Khryanin A.A. In search of interferon. Status Praesens (gynecology, obstetrics, infertile marriage) 2020;1:79-83. [Khryanin AA In search of the interferon. Status Praesens (gynecology, obstetrics, infertile marriage) 2020;1:79-83. (In Russian)].
Comments
To post comments you must log in or register
Suppositories for the treatment of cystitis
Many medicines come in several forms. In addition to tablets, vaginal and rectal suppositories are used to quickly deliver the active substance through the mucous membranes. Candles are well suited for people with gastrointestinal disorders. In addition, vaginal suppositories with anti-inflammatory, antifungal and bactericidal effects better stop the spread of pathogens directly in the affected area. This is much more effective than using tablets.
Capsules
Another common dosage form for the treatment of cystitis. Their peculiarity is that capsules are taken less often than tablets. In most cases - 1 time per day. The concentration of the active substance in the capsule is higher. But its hard gelatin shell, gradually dissolving, ensures optimal absorption of the drug.
The following are most often prescribed in capsules:
Azithromycin.
Broad-spectrum antibiotic from the macrolide-azalide group. Slows down the proliferation of bacteria, and in high concentrations has a bactericidal effect. Dosage – 2 capsules (500 mg at a time).
Monural.
An antibiotic with bactericidal properties that has a broad spectrum of action against bacteria that cause urinary tract infections. The drug is used in the treatment of cystitis, including in the blood. Monural is approved for use by pregnant women, as it does not harm the health of the fetus.
Take one dose (3 grams), if necessary, the drug can be repeated every other day.
The effectiveness of medications depends on a number of factors, including the type of pathogen, the severity of the condition, the presence of complications, and the patient's general medical history. Therefore, individual selection of drug therapy based on test results is so important.
How is acute cystitis treated at the Rassvet Clinic?
Urologists at Rassvet, like all doctors at our clinic, adhere to the principles of evidence-based medicine. Unnecessary examinations and ineffective medications are not prescribed. The diagnosis of acute cystitis is established based on the patient’s complaints and the collected medical history, and antibiotic therapy with first-line drugs is prescribed. Additional studies are carried out only if there are indications - there is no effect of the therapy.
It is important to know: if therapy is ineffective or there are frequent relapses, cystitis is classified as recurrent, which, with some simplification, can be called “chronic”.
Author:

Loktev Artem Valerievich urologist
Physiotherapy for cystitis
Physiotherapeutic techniques are used for the chronic course of the disease. The procedures can be carried out in parallel with drug therapy.
- Electrophoresis. Directed exposure to a weak electric current along with the use of medications. Electrophoresis accelerates and enhances the penetration of active substances into tissues. Relieves inflammation, soothes pain, destroys germs.
- Magnetotherapy. Exposure of the inflamed organ to a magnetic field. Accelerates the destruction of bacteria and viruses.
- Inductotherapy. Warming the affected organ with electrical impulses. Dilates blood vessels, accelerates blood flow, facilitates the functioning of the urinary system.
- Magnetophoresis. Exposure of the affected areas of the mucous membrane to a directed magnetic field. It is carried out strictly as prescribed by the doctor.
- EHF. The electromagnetic field affects the bladder. The procedure relieves pain, reduces inflammation, destroys bacteria and viruses.
What is bioflora and why do you need to know its composition?
Flora is a complex of bacteria that inhabit a specific department or area in the body. Bioflora can be normal and pathogenic. Pathogenic composition implies the inclusion of pathogenic bacteria that have a detrimental effect on health. They can cause inflammation, destroy tissue, poison the body, or destroy beneficial flora, making room for other pathogens.
Knowing the composition of the flora in the organ, it is easy to choose an effective treatment. If pathogens are found that are resistant to most common drugs, an additional study is carried out - antibiotic sensitivity tests. The laboratory technician treats the sample with bacteria with different drugs, determining the strongest one that completely destroys the infection.
Traditional methods of treating cystitis
The condition can be alleviated not only with medications, but also with alternative medicine methods. As a supplement to the main therapy and in consultation with the attending physician, the use of folk remedies is permissible.
Infusion of dill seeds.
Pour boiling water over one tablespoon of seeds, cover and let steep for 2 hours. You can use a thermos for this purpose. Take a glass of the drink three times a day until the condition improves.
Millet decoction.
Pour 2 tablespoons of millet into 500 ml of boiling water, put on low heat and cook for 4 - 5 minutes. Then let the broth brew, pour into a glass, and cool. For acute cystitis, take the decoction 20 ml every hour on the first day, 60 ml on the second, 100 ml on the third. Treatment continues for up to 7 days.
Chamomile decoction.
Pour 10 grams of dried flowers with a glass of boiling water, cover and let it brew for half an hour. Throughout the illness, take 60 ml of decoction half an hour before meals.
Lingonberry berries and leaves.
You can simply eat the berries, and a healing infusion is prepared from the leaves. To do this, pour one tablespoon of crushed leaves into a glass of boiling water, cover, and let it brew for several hours. For acute cystitis, this drink should be drunk three times a day, 60 ml.
For the treatment of cystitis, decoctions and infusions of bearberry, birch leaves, horsetail, plantain, flax seeds, licorice root, parsley, black currant leaves, celandine, string, sage, calendula, linden are also good. Special mixtures and medicinal teas can be bought at the pharmacy or prepared yourself.
An effective remedy for alleviating the general condition of cystitis is warm (not hot!) sitz baths. These procedures relieve pain in the urethra, relax, and promote bladder emptying. For baths, it is good to use infusions of sage, chamomile, pine needles, and horsetail. Water temperature – no more than 42 °C. The procedure is carried out before bedtime for 15 minutes.
Important! Baths are contraindicated for hemorrhagic cystitis!
An interesting folk way to combat illness is aromatherapy. Proponents of this treatment advise using essential oils at the first signs of cystitis. To relieve pain attacks, it is recommended to inhale the aromas of anise, bergamot, spruce and cedar, pine, cypress, lime, lavender, eucalyptus, tea tree.
Healing mixture: 10 drops of lavender oil, 8 drops of bergamot, 5 drops of eucalyptus, 3 drops of tea tree. Oils are added to the aroma lamp.
Also among the popular non-traditional methods of treating cystitis are acupuncture (acupuncture) and homeopathy.
Diet for the treatment of cystitis
A predominantly dairy-vegetable diet helps to cope with the disease faster. You need to eat more vegetables, fruits, and dairy products. It is worth giving up fatty, fried, spicy, salty, and lots of spices. Alcohol is strictly prohibited during medication treatment. The best solution is mostly vegetarian food and plenty of water.
Following a diet helps alleviate the condition:
- reduces the manifestations of intoxication in the body;
- reduces the rate of microbial reproduction;
- increases the effectiveness of antibacterial therapy.
Timely seeking medical help, competent selection of medications and strict adherence to recommendations are the conditions for successfully overcoming the disease. Don't delay your visit to the doctor!
Risk factors predisposing to the development of cystitis
- Hypothermia of the body - if you sit on something cold, dress lightly in cool weather, swim in cool water;
- Insufficient consumption of plain water;
- Eating spicy, fried, salty, sour, spicy foods;
- Drinking large amounts of alcohol;
- Chronic foci of infection (chronic tonsillitis, carious teeth, frequent sore throats);
- Wiping with toilet paper from the anus to the vagina, this applies to the female sex;
- Sedentary lifestyle;
- Irregular or, conversely, too vigorous sex life;
- Promiscuous sexual intercourse leading to STDs;
- Rare visits to the gynecologist;
- Prolonged abstinence from urination;
- Constipation.