MRI of the male genital organs is a study that allows us to speak with high confidence about the causes of certain problems in the patient.
Let's look at the examples of several studies.
The corpora cavernosa surrounded by the tunica albuginea (arrowheads), the corpus spongiosum (*) and the arteries of the corpora cavernosa (curved arrows) are visualized.
Penile injury
There is a violation of the integrity of the right corpus cavernosum and a rupture of the surrounding tunica albuginea (arrows) with the formation of a subcutaneous hematoma - a “fracture” of the penis.
Peyronie's disease
Connective tissue is damaged with the formation of fibrous local thickenings of the tunica albuginea of the penis and intracavernous septa. Synonyms: fibrous cavernitis, plastic induration of the penis.
Dorsal induration of the tunica albuginea and significant dorsal deformation of the penis are determined. Arrows show significant focal thickening of the dorsal parts of the tunica albuginea (large plaque).
Inflammation of the corpus spongiosum of the penis (spongiositis)
Inflammatory infiltration of the ventral sections of the penis, an increase in the size of the corpus spongiosum.
Tumors of the penis.
The most common cancer is penile cancer. Peak incidence occurs between 50 and 70 years of age.
In the distal parts of the penis, a tumor mass of heterogeneous structure is determined, with invasion of the cavernous bodies (black arrow). A small metastasis is identified in the proximal part of the corpus cavernosum (small white arrow).
Metastatic lesion of the penis
Etiology: primary tumors of the genitourinary tract (PCa, urothelial cancer).
The patient had a history of bladder resection for urothelial cancer 4 years ago. A tumor of the glans penis (metastatic lesion) is determined to have a heterogeneous structure.
Thrombosis of the corpus cavernosum
Arterial or venous causes leading to poor circulation in the corpora cavernosa of the penis.
An increase in size and a change in the signal from the left corpus cavernosum are determined. The corpus cavernosum on the right is without features. Segmental thrombosis of the corpus cavernosum.
Fibrous changes of the cavernous bodies
Fibrous tissue is formed in the corpora cavernosa due to prolonged disruption of the blood supply.
Post-traumatic fibrotic changes, most pronounced in the left cavernous body.
Consequences of priapism
Condition after 2-sided corpora cavernosa bypass for priapism. On the right, successful shunting (normal size and signal from the corpus cavernosum). On the left, bypass surgery was unsuccessful; the corpus cavernosum was enlarged in size, with signs of ischemia and developing infarction.
Organs of the scrotum
Testicular tumors most often occur between the ages of 15 and 40 years.
Small right-sided hydrocele (*). The septal structure of the tumor, revealed by intravenous contrast.
Left-sided seminoma with invasion of the left spermatic cord.
Lipoma of the spermatic cord, hydrocele
Hematoma of the right spermatic cord after repair of an inguinal hernia.
Varicocele (arrow) and hydrocele (*) on the left.
Polyorchidism
Inflammatory diseases of the scrotum
Anatomy of the scrotum and penis
The scrotum is a part of the male reproductive system, located behind and inferior to the penis and anatomically representing a saccular formation of skin and smooth muscle. The organs of the scrotum are the testes (male reproductive glands), epididymis and vas deferens. In addition, there are blood vessels, a venous plexus, lymphatic ducts and nerves.
The main functions of the scrotal organs are the production of sperm and the synthesis of male sex hormones. If the latter are secreted directly into the blood, then a complex system of the vas deferens is used to deliver the germ cells. The vas deferens, in turn, communicates with the ducts of the seminal vesicles and prostate gland, forming the ejaculatory duct, which opens into the urethra.
The urethra mostly passes inside the penis, formed by the cavernous and spongy bodies, opening at the top of the glans with the external opening of the urethra. The clinical significance of this structure of the male reproductive system is that for successful fertilization it is necessary to meet several conditions - the production of normal sperm in sufficient quantities, the synthesis of male sex hormones, the absence of obstacles in the lumen of the vas deferens and the ejaculatory duct, the absence of pathologies of the prostate gland and seminal vesicles, physical the ability to maintain an erection during sexual intercourse. The consequence of violation of these conditions at any level is male infertility.
What research information is important for the doctor?
Correct diagnosis of changes in the arterial and venous system of the penis allows the attending doctor to accurately prescribe treatment and achieve a positive result. To make a diagnosis, he needs to evaluate:
- the condition of the vascular wall of the circulatory system in the area of the penis;
- width of the arterial and venous lumen;
- the presence and number of atherosclerotic plaques.
Based on the results obtained, the andrologist can diagnose:
- vascular thrombosis of varying degrees;
- fibrosis of the corpora cavernosa;
- stenosis of the penile arteries;
- tumor of various origins;
- Peyronie's disease;
- atherosclerotic vascular disease of the organ under study.
The information obtained during diagnostics at the “Men’s and Women’s Health Clinic” is absolutely reliable, therefore we can guarantee the effective elimination of any deviations.
Diseases of the scrotal organs

Inflammation of the testicles and their appendages
Inflammation of the testicles (orchitis) and their appendages (epididymitis) can be caused by various infections. In children, the most common cause of epididymitis orchiodermitis is the mumps virus (mumps). In adults, epididymitis orchiepididymitis is often a consequence of sexually transmitted infections. The disease can occur either in an acute form, with pain, swelling and redness of the scrotum, or in a chronic form, without obvious symptoms.
Hydrocele or hydrocele
Dropsy is the accumulation of serous fluid in the scrotal cavity, between the membranes of the testicles. The cause of the disease can be congenital developmental anomalies, inflammatory diseases, neoplasms and injuries. Dropsy itself is rarely accompanied by severe symptoms; pain, heaviness in the scrotum, and discomfort are possible.
Varicocele

Varicocele or varicose veins of the pampiniform plexus is a common disease that, without treatment, can lead to male infertility. The disease is provoked by weakness of the venous wall and often occurs as a concomitant pathology with hemorrhoids and varicose veins of the lower extremities. Most often, varicocele is diagnosed on the left side, but it can also be bilateral. Due to stagnation of venous blood, the blood supply to the testicles is disrupted, a lack of oxygen (ischemia) occurs, followed by sclerosis and atrophy of the testicles (which ultimately leads to infertility). That is why varicocele must be treated (surgical treatment).
Testicular torsion
Testicular torsion is a condition that often occurs in children and young adults in which the neurovascular bundle that suspends the testicle in the scrotal cavity is twisted. As a result, the blood supply to the testicle is disrupted, causing acute ischemia, intense pain, swelling, nausea and vomiting. Treatment is surgical.
Hypogonadism or testicular atrophy
Hypogonadism or testicular atrophy can occur as a result of hormonal disorders (pituitary hormone deficiency) or as a result of a long-term chronic disease such as varicocele. The deficiency of male sex hormones that occurs during hypogonadism leads to impotence, infertility, enlarged mammary glands, depression, osteoporosis and a number of other serious disorders.
Spermatocele
Spermatocele or epididymal cyst is a benign neoplasm that rarely requires treatment. Epididymal cysts are cavities filled with seminal fluid. If the spermatocele is small in size, it may be asymptomatic, and only if it is significantly enlarged, the patient may experience pain and a feeling of heaviness.
Developmental anomalies
Anomalies in the development of the genitourinary system in men are most often represented by cryptorchidism or undescended testicles into the scrotal cavity. During intrauterine development, the testicles initially develop in the abdominal cavity, from where they gradually descend into the scrotum through the inguinal canal. If this process is disrupted, the child may be born with dystopia or a violation of the normal location of the scrotal organs. In half of the cases, the testicles descend into the scrotum during the first year of life, but if this does not happen, mandatory surgical treatment is required - cryptorchidism significantly increases the risk of testicular cancer and infertility.
Benign and malignant tumors
The testicle is a gland of internal and external secretion, and like other glands, benign and malignant neoplasms often arise in it. Testicular tumors are divided into several groups, depending on their origin and nature. In some countries, testicular cancer is the most common malignancy in young men.
Magnetic resonance imaging of the scrotum is an ideal method for diagnosing all possible diseases of the male reproductive glands and related pathologies. MRI is especially important in diagnosing developmental anomalies and testicular tumors. Magnetic resonance imaging does not require complex procedures, is comfortable for the patient who does not need to undress in front of an unfamiliar doctor, and is safe for health. Clear, detailed images greatly facilitate the diagnosis of diseases of the scrotal organs.
Diagnostic results
Using this type of examination, such as MRI of the uterus, a huge number of different pathologies of the pelvic organs are revealed. So an MRI of the uterus and ovaries shows:
- inflammation of the fallopian tube, as well as a decrease in the lumen in it due to suppuration and other things;
- neoplasms and metastases, for example, uterine fibroids;
- obstruction of the fallopian tubes or the presence of adhesions;
- abnormalities in the development of the pelvic organs, for example, the presence of a septum in the uterus or its atypical shape and structure;
- acute inflammations in which emergency surgical intervention is indicated;
- consequences of injuries and past surgical operations, for example, scars, fistulas and others;
- vascular problems, such as thrombosis;
- enlarged lymph nodes.
MRI for uterine fibroids allows you to determine the exact size and number of tumors, as well as track the rate of their growth. It is also possible to obtain data on the condition of the pelvic floor muscles, bones, bladder and rectum, relevant for injuries and cancer.
Contraindications to MRI of the scrotum
Magnetic resonance imaging has virtually no contraindications - all limitations to the study are related to the fact that in order to obtain images it is necessary to constantly maintain a powerful magnetic field. It is for this reason that MRI is prohibited in the following cases:
- The patient has electronic medical devices in his body - cochlear implants, artificial heart pacemakers, neurostimulators, and other devices;
- There are metal foreign bodies in the patient's body - iron or steel particles in the eyes, stainless steel vascular clips, stents, shot or shrapnel.
It is not recommended to do an MRI of the scrotum in children under the age of 5 years - during the examination, the patient must be completely immobile, which cannot be achieved in small patients without sedation. This study should be performed in specialized diagnostic departments of children's hospitals.
Excess body weight may interfere with MRI. The equipment is designed to accommodate patients weighing up to 130 kg and body circumference up to 150 cm. Otherwise, they are physically unable to fit into the MRI installation.
Indications for examination
MRI of the uterus is performed as prescribed by a doctor in the following cases:
- suspicion of ectopic pregnancy;
- pelvic organ injuries;
- infertility of unknown etiology;
- inflammatory diseases of the pelvic organs;
- disrupted menstrual cycle;
- the presence of benign and malignant neoplasms;
- the presence of sharp pain in the lower abdomen as the main examination procedure;
- preparation for operations;
- vaginal bleeding of unknown origin;
- monitoring the effectiveness of therapy and the persistence of remission.
Preparing for MRI of the scrotum
Magnetic resonance imaging of the testicles does not require any preparatory measures. The study can be done at any time convenient for the patient, without regard to diet or diet. What is really important is strict adherence to safety regulations. Due to the presence of magnetic fields in the MR imaging room, it is prohibited to undergo the examination with metal objects or electronic devices in your pockets or on your body. This could be jewelry, cell phones, piercings, multitools, or cigarette cases. When exposed to a magnetic field, any metal object can heat up, causing burns, or turn into a projectile, causing injury and disfigurement.
Purpose of the procedure
MRI is used to diagnose organs for completely different indications. Among them are:
- injuries and bruises;
- pain of unknown origin;
- suspected pathologies;
- monitoring the impact of therapy;
- detection of diseases in men and women with infertility in couples.
In most cases, doctors of narrow specializations are referred for the study: urologist, proctologist, gynecologist or oncologist. The doctor makes a conclusion about the need for hardware diagnostics based on previously collected information: anamnesis (patient testimony), tests, primary examinations. When it is necessary to examine a woman’s pelvis, and what indications are more common in men, is determined only by a doctor of a particular specialization.
Make an appointment now!
How to do an MRI of the scrotum and penis

To perform an MRI, the patient is placed in a special machine - an MRI scanner. Outwardly, it looks like a large cylinder laid on its side. In the center of the cylinder there is a short and wide tunnel (60x60 cm), along which the table moves. During the examination, the patient lies on his back.
Before starting the procedure, you will be asked to put on headphones - they protect your hearing from noise coming from the equipment. The headphones also serve to communicate with the operator - to call him, just press a button, which is also given to the patient. Music is also broadcast through headphones - it helps the patient relax and make the procedure more comfortable.
The duration of MRI scanning of the scrotal organs is up to 15 minutes. In some cases, if a tumor or inflammation is suspected, MRI may be performed with contrast. To do this, a special contrast agent is injected into the patient's antecubital vein. It selectively collects in pathologically altered tissues affected by the disease, which is clearly visible in the photographs. Contrast facilitates diagnosis and increases the accuracy and reliability of the method. When using contrast, the duration of the study increases to 30 minutes.
After completing the examination, you must wait 15-30 minutes - the images obtained during the procedure must be decrypted. This is done by a radiologist, who, after completing the decoding, will advise the patient on the results of the examination, show the images and the detected changes. The images and doctor's report must be submitted to your attending physician. To store and transfer images, use CDs (free), film or flash drive (paid separately).
Video about the service
MRI of the external genitalia for men is absolutely safe. This diagnostic examination is characterized by the absence of radiation exposure, and therefore does not affect the ability to have children, as well as sexual activity. This diagnostic has no analogues in terms of information content and reliability. With its help, you can reliably establish any pathologies that have arisen in the external genitalia of a man.
Our MRT24 centers, located near metro stations in Moscow, receive patients around the clock. Therefore, for diagnosis you will not need to make changes to your usual schedule. We have indicated the addresses and prices of diagnostic tests on this page. A loyal pricing policy for medical services has allowed us to make their costs affordable for a large number of residents and guests of the capital.
What does an MRI of the scrotum show?
MRI images of the scrotum, which are virtual layer-by-layer sections through the area of interest, show the testicles, epididymis, vessels and nerves, pampiniform plexus, vas deferens and testicular membranes. Looking through the images, the doctor pays attention to signs of pathological changes - inflammation, fluid accumulation, dilation of the veins of the pampiniform plexus, the presence of cysts and other space-occupying formations, such as benign or malignant tumors.

Preparation measures
The doctor usually explains how to prepare for the procedure. For most pelvic procedures, an empty bowel is desired, but not an empty bladder. Prepare for the examination the day before: eating a light meal that does not cause gas formation, using an enema, laxatives.
Before MRI using contrast, the presence of allergies or relative contraindications is clarified. For example, contrast is not used for pregnant and lactating women and all people suffering from complex kidney diseases.
At the “MRI Center” you can consult about everything that is included in an MRI, how to prepare for a man and a woman, what is the price of the procedure for certain types of examination.
MRI or CT scan of the scrotum
Magnetic resonance imaging, unlike computed tomography, has the ability to “see” soft tissue. CT, unlike MRI, is based on the use of X-rays - and the denser the tissue, the better they are visible in the images. Soft tissues practically do not block x-rays and are poorly visible on photographs, only in the form of shadows. Moreover, the use of CT for diagnosing diseases of the scrotum is undesirable for safety reasons - the radiation that accompanies computed tomography negatively affects spermatogenesis and can lead to the birth of a sick child.
Decoding the received data
Using MRI, you can take a series of digital images. It is the doctor’s task to recognize normal and pathological conditions in photographs. The decoding usually takes a specialist from 1 to 3 hours, after which the patient receives digital images on paper or electronic media, as well as a doctor’s report.
If studies have already been carried out regarding diseases of the genital organs or pelvis, you can take their results with you. Any information about the disease, previous diagnoses and treatment provided can make the functional diagnostic doctor’s conclusion more informative.
When is ultrasound diagnostics mandatory?
The occurrence of the slightest disorder or neoplasm requires immediate consultation with a doctor. Early diagnosis and adequate treatment will avoid complications, large financial costs and drastic medical intervention.
To draw up a complete picture of the disease, the specialist needs an examination of the patient and the results of clinical diagnostics.
The doctor will necessarily ask you to do an ultrasound of the penile structures in a number of cases:
- traumatic injury to the reproductive organ;
- decreased erectile function;
- curvature of various types;
- neoplasms in the penis area.
Radiation diagnostics of arteriovenous erectile dysfunction: history and development
P.S. Kyzlasov 1, B.G. Kasymov 2, S.Kh. Al-Shukri 3, E.A. Iskakov 2, R.M. Nugumanov 2, I.V. Kuzmin 3, T.M. Muratov 2, T.N. Turgumbayev 2
1FGBU State Scientific Center of the Russian Federation - Federal Medical Biophysical Center named after. A.I. Burnazyan" FMBA of Russia, Moscow; 2JSC National Scientific Medical Center, Astana, Kazakhstan; 3Federal State Budgetary Educational Institution of Higher Education “First St. Petersburg State Medical University named after. acad. I.P. Pavlova" of the Ministry of Health of Russia
The term “erectile dysfunction” (ED) refers to the inability to achieve or maintain penile rigidity sufficient for sexual intercourse. This term replaced the concept of “impotence,” which in itself placed an additional psychological burden on the patient [1]. ED leads to a significant disruption of the harmony and well-being of sexual health and, as a result, to a significant decrease in the quality of life of men of any age. According to a large epidemiological study, the prevalence of ED in men aged 40 to 70 years is 52%, with mild and moderate ED observed in 17.2 and 25.2% of cases, respectively, and severe ED in 9.6% of cases [2]. The prevalence of the disease is directly dependent on the age of the patient: at the age of 18-29 years, the frequency of ED is 7%, 30-39 years - 2-9%, 40-49 years - 9-11%, 50-59 years - 16-18 %, 60–69 years old – 34%, 70 years and older – 53% [3–6]. The incidence of ED is 26 per 1000 men [2].
In the Republic of Kazakhstan, an analysis of the prevalence of ED was carried out, for which 1550 men aged 21 to 79 years were examined. ED was detected in 784 (52.3%) of them, while signs of ED with concomitant age-related hypogonadism were detected only in 21 (1.1%) men [7].
The availability of various methods of treating ED and the active work of the media have led to the fact that a significant proportion of men self-medicate without undergoing an appropriate medical examination. Less than 10% of patients suffering from ED turn to specialists for medical help, the rest either do not receive treatment at all, or independently use drugs advertised in the media [8]. Many men believe that the problem associated with ED is caused by age-related changes and resign themselves to the current situation. On the other hand, urologists often do not ask patients about their sexual life during appointments, unless, of course, the reason for the visit was ED itself [9].
In 70–80% of cases, the cause of ED is vascular disorders, of which 30% are associated with a decrease in arterial blood flow to the cavernous bodies, 30% with an increase in venous outflow, and 40% have a mixed origin [10, 11]. Modern technical support for hospitals and outpatient clinics makes it possible to carry out all the necessary studies of arteriovenous ED - ultrasound, X-ray, computer or nuclear magnetic diagnostics [12]. The most common methods of radiological diagnosis of arteriovenous ED in modern urology are:
- Ultrasound examination (US) using Dopplerography of the vessels of the penis (Fig. 1, 2);
- cavernosography using computed tomography of the penis (CT), magnetic resonance imaging (MRI).
Rice. 1. Ultrasound Dopplerography of the vessels of the penis is normal: a - 1, 2 (between the arrows) - the penis is not erect; 3 - cavernous bodies of normal echogenicity; 4 (arrows) - urethra; 5 - scrotum; b - 1, 2 - penis during erection; 3 - cavernous bodies during erection; 4 (arrows) - urethra; 5 - scrotum
Rice. 2. Ultrasound Dopplerography of the vessels of the penis. Cavernous arteries highlighted
In all of these studies, pharmacological erection stimulants (PDE-5 inhibitors, prostaglandin preparations) are used [13].
The use of Dopplerography of the penis to diagnose ED began in the late 70s - early 80s, and in the late 90s. XX century due to the advent and distribution of PDE5 inhibitors, it has become a widespread research method [14]. The Consensus Committee on the Study of Erectile Dysfunction in June 1999 recommended penile ultrasound with intracavernous pharmacotest as the first specialized method for examining patients with ED. It was noted that this study is characterized by low invasiveness, high information content and relatively low cost [15]. Modern comprehensive ultrasound of the penis includes the following technologies: B-mode, Doppler methods consisting of the pulse-wave mode, the so-called PulseWave, Color Doppler Energy, triplex mode, which is a combination of the first three, and the B-flow method (B-flow) [16].
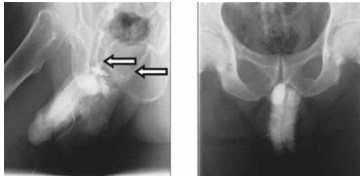
Rice. 3. X-ray cavernosography
Thanks to the minimally invasive nature of Dopplerography of penile vessels, as well as the technical development of ultrasound equipment, this technique has now become indispensable in the diagnosis of ED [17]. However, this study has a number of disadvantages, such as inaccuracy of measurement at high blood flow velocities, inability to estimate the blood flow velocity throughout the entire length of the vessel; in addition, the placement and tilt of the ultrasound sensor itself significantly influence the result of the study [18].
In patients with arteriogenic erectile dysfunction, the diagnostic value of ultrasound of the internal pudendal artery using a transperineal approach has been demonstrated [19]. According to the authors, the method has a sensitivity of 95%, a specificity of 90% and allows one to assess important morphometric features of the internal pudendal artery: its diameter, response to stimulation, course of the artery, type of blood flow in the artery; determine the presence or absence of stenosis and occlusion in the artery.
One of the main methods for diagnosing ED of vascular origin is cavernosography - an X-ray examination of the vessels of the penis, during which a radiopaque substance is injected into the cavernous bodies through a small needle (Fig. 3). The resulting x-ray allows you to determine the condition of the blood vessels of the penis. Using this method, you can confirm or exclude the presence of ED of venous etiology and determine the level of venous blood discharge [20].
Cavernosography was first described in 1946 by A. De la Pena as a method of visualizing the pelvic veins [21]. In 1955, F. May and H. Hirtl described the x-ray image of the normal cavernous bodies, as well as the pathological changes that occur with trauma, inflammation, tumors of the cavernous bodies and priapism [22]. The modern understanding of the term “cavernosography” was proposed in 1984 by R. Virag et al., who performed an X-ray examination of the corpora cavernosa after administration of the vasoactive drug papaverine, which induces erection and allows visualization of the corpora cavernosa in an erect state [23]. Using dynamic cavernosography, it is possible not only to diagnose the presence of pathological leakage, but also to determine the number of pathological communicating veins, their level and discharge basin [24]. Pharmacocavernosography is usually performed in two projections; it demonstrates contrasted venous vessels, through which blood is predominantly discharged from the corpora cavernosa [25].
Traditional cavernosography and pharmacocavernosography are diagnostic methods for visualizing the pathology of the venous system of the penis. However, despite the relative reliability and widespread use of pharmacocavernosography, this method has a number of noticeable disadvantages: the use of iodine-containing contrast agents in large doses and the associated possibility of developing complications (allergic reactions), the presence of ionizing radiation in high doses. In addition, traditional cavernosography cannot be digitized and there is no possibility of constructing a three-dimensional image. Moreover, the frequency of false positive results when using the above methods reaches 20–25% [26]. In modern diagnostics, given the high invasiveness and radiation exposure, cavernosography is often combined with other techniques. The combination of cavernosography with manometry is effective for detecting anatomical defects primarily in veno-occlusive ED [27].
Computer cavernosography is used in patients with suspected arteriovenous ED and when dynamic cavernosography is ineffective [26].
In 2011, a new method for recognizing venous erectile dysfunction was studied at the Takamatsu Red Cross Hospital (Japan). The authors of the study used a 3D-processing technique for CT images of the penis after introducing a radiocontrast agent into the cavernous bodies (Fig. 4). 3D computer cavernosography was performed in 90 patients, and the diagnosis of ED was confirmed in all patients. The study authors noted that with venous erectile dysfunction, in almost 92% of patients, blood leaked into the preprostatic venous plexus, into which the deep dorsal vein of the penis drains [28].
To visualize anatomically “deeply” located vascular structures and assess their volumetric and spatial relationships O.B. Zhukov et al. (2009) used multislice computed tomography of the pelvic organs, penis and scrotal organs in patients with ED [29]. E.A. Efremov et al. (2012) used dynamic computer cavernosography to diagnose ED in patients with suspected pathological venous drainage. The authors concluded that among the currently available methods for diagnosing venogenic ED, dynamic computer pharmacocavernosography has the best sensitivity and specificity [30]. Unfortunately, this method, despite its low invasiveness and the absence of the need for intracavernosal contrast administration, is not without such disadvantages as the presence of radiation exposure, high cost, rapid passage of the vascular phase with contrast, and therefore it is often difficult to obtain images of both major and minor vessels.
Flat panel CT is used to diagnose disorders of the veno-occlusive mechanism in ED. Advantages of the method: a small amount of contrast agent, the possibility of three-dimensional reconstruction of the vascular bed due to high spatial resolution, low radiation dose, and the absence of artifacts from metal objects. However, the following disadvantages of the method were noted: the need to use complex equipment, intracavernous administration of a contrast agent [31].
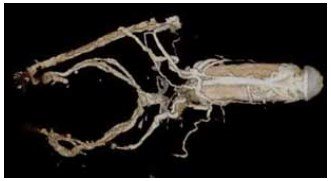
Rice. 4. Computer cavernosography
MRI is a highly effective research method that allows one to obtain contrast images of internal organs in any plane with high resolution without the use of ionizing radiation or the introduction of radioactive substances, which is especially important for diagnostic studies of the genitourinary system [32]. MRI of the penis makes it possible to analyze the structure of the cavernous tissues and visualize the perineal and penile arteries affected by ED (Fig. 5). However, more reliable vascular insufficiency in ED can only be detected using contrast-enhanced MR angiography [33].
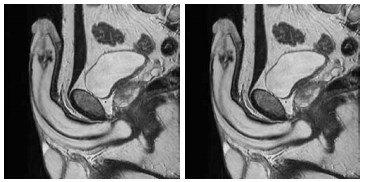
Rice. 5. Magnetic resonance cavernosography
M. Bernstein et al. (1998) conducted this examination in 17 patients with post-traumatic ED with preliminary intracavernosal administration of a vasoactive drug (prostaglandin E1) and in 70% of cases they visualized damage to the pelvic vessels (occlusion of the internal pudendal artery) [34]. MRI of the penis is possible against the background of functional cavernosography using gadolinium [35]. The contrast effect is achieved due to the ability of gadolinium-containing drugs to change the relaxation properties of extracellular fluid, which is manifested by a shortening of the T1 relaxation time and an increase in the intensity of the signal from the blood with special pulse sequences. Thus, an effect similar to that achieved with angiography is recorded [35]. MRI of the penis helps to identify the anatomical structures of the penis, and when diagnosing surrounding and pathologically altered tissues, it is possible to verify the state of the veno-occlusive mechanism, regardless of the predominance of corporal and post-corporal factors. However, the disadvantages of penile MRI in diagnosing veno-occlusive ED include the maximum invasiveness and high cost of the procedure. It is believed that MRI with intracavernosal contrast is the method of choice for objective visualization of pathological draining veins of the penis in patients with venogenic ED and its use is advisable in difficult diagnostic cases [36]. Considering the high efficiency of MRI and the complete absence of ionizing radiation, this research method is the main one in the diagnosis of venogenic ED, especially in young patients.
Thus, today the optimal methods for radiological diagnosis of arteriovenous ED should be considered MRI and CT cavernosography with intracavernosal contrast, which have the greatest sensitivity and specificity. Considering the growing trend in the incidence of ED and its high prevalence in all age categories, the main causes of which are vascular disorders, we consider it necessary to introduce into clinical practice new minimally invasive, objective, highly informative and harmless imaging techniques for diagnosing erectile dysfunction, such as MRI and CT cavernosography .
LITERATURE
- NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270(1):83-90. doi: 10.1001/jama.270.1.83.
- Derby CA, Barbour MM, Hume AL, McKinlay JB. Drug therapy and prevalence of erectile dysfunction in the Massachusetts Male Aging Study cohort. Pharmacotherapy. 2001;21(6):676-683. doi: 10.1592/phco.21.7.676.34571.
- Male sexual dysfunction. EAU Guidelines / Ed by K Hatzimouratidis, F Giuliano, I Moncada, et al. EAU: 2021. https://uroweb.org/guideline/male-sexual-dysfunction.
- Goldstein I, Mulhall J, Bushmakin A, et al. The erection hardness score andits relationship to successful sexual intercourse. J Sex Med. 2008;5(10):2374-2380. doi: 10.1111/j.1743- 6109.2008.00910.x.
- Mazo E.B., Gamidov S.I., Iremashvili V.V. Erectile disfunction. – 2nd ed. – M.: MIA, 2008.
- Prins J, Blanker MH, Bohnen AM, et al. Prevalence of erectile dysfunction: a systematic review of population-based studies. Int J Impot Res. 2002;14(6):422-432. doi: 10.1038/ sj.ijir.3900905.
- Khamzin A.A., Frolov R.A. Distribution of erectile dysfunction among the urban population of the Republic of Kazakhstan aged 21 to 79 years // Modern medicine: current issues. – 2014. – No. 30. – S. 89–93.
- Eardley I, Mirone V, Montorsi F, et al. An open-label, multicentre, randomized, crossover study comparing sildenafil citrate and tadalafil for treating erectile dysfunction in men naive to phosphodiesterase 5 inhibitor therapy. BJU Int. 2005;96(9):1323-1332. doi: 10.1111/j.1464-410x.2005.05892.x.
- McKinlay JB. The world wilde prevalance and epidemiology of erectile dysfunction. J Impot Res. 2000;12(Suppl. 4):6-11.
- Pushkar D.Yu., Kamalov A.A., Al-Shukri S.H., et al. Analysis of the results of an epidemiological study of the prevalence of erectile dysfunction in the Russian Federation // Urology. – 2012. – No. 6. – S. 5–9. [Pushkar' DJu, Kamalov AA, Al'-Shukri SH, et al. Analysis of the results of epidemiological study on the prevalence of erectile dysfunction in the Russian Federation. Urologiia. 2012;(6):5-9. (In Russ.)]
- Zhukov O.B., Zubarev A.R., Kulchenko N.G. Pathological venous drainage of the corpora cavernosa of the penis in patients with varicocele // Medical visualization. – 2006. – No. 1. – P. 82–89.
- Briganti A, Naspro R, Gallina A, et al. Impact on sexual function of holmium laser enucleation versus transurethral resection of the prostate: results of a prospective, 2-center, randomized trial.J Urol. 2006;175(5):1817-1821. doi: 10.1016/s0022-5347(05)00983-3.
- Amosov A.V., Petrovsky N.V., Demidko Yu.L., Baiduvaliev A.M. Individual selection of the dose of sildenafil in the treatment of erectile dysfunction // Russian Medical Journal. – 2014. – T. 22. – No. 17. – S. 1292–1297.
- Cappelleri JC, Rosen RC, Smith MD, et al. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54(2):346-351. doi: 10.1016/s0090-4295(99)00099-0.
- Kostylev M.V., Egorova O.N., Khokholya A.V., Dryuk N.F. Diagnosis of erectile dysfunction according to ultrasound examination of the vessels of the penis // Heart and Vessels. – 2005. – T. 11. – No. 3. – S. 45–54.
- Zubarev A.R., Koryakin M.V. Ultrasound diagnosis of venous and corpovenous insufficiency of the penis // Ultrasound diagnostics. – 2000. – No. 2. – P. 56–61
- Yildirim D, Bozkurt IH, Gurses B, Cirakoglu A. A new parameter in the diagnosis of vascular erectile dysfunction with penile Doppler ultrasound: cavernous artery ondulation index. Eur Rev Med Pharmacol Sci. 2013;17(10):1382-1388.
- Shcheplev P.A., Danilov I.A., Kolotinsky A.B., et al. Clinical recommendations for erectile dysfunction // Andrology and genital surgery. – 2007. – No. 1. – S. 59–65.
- Povelitsa E.A., Dosta N.I., Parkhomenko O.V., et al. Ultrasound examination of the internal pudendal artery using transperineal access for arteriogenic erectile dysfunction // Urology. – 2021. – No. 4. – S. 55–61. . doi: 10.18565/urol.2017.4.55-61.
- Baev A.A., Gromov A.I., Kulchenko N.G. Radiation diagnostics and therapy in urology. – M.: GOETAR-Media, 2011.
- De la Pena A. Flebografia de plexos e vasos palvianos en el vivo. Revista Espaniola de Cirugia, Traumatologia y Ortopedia. 1946;4:245-251.
- May F, Hirtl H. Das cavernosogramm. Urol Int. 1955;1(2): 120-134. doi: 10.1159/000277078.
- Virag R, Frydman D, Legman M, Virag H. Incavernous injection of papaverine as a diagnostic and therapeutic method in erectile failure. Angiology. 1984;35(2):79-87. doi: 10.1177/0003319784 03500203.
- Mikhailov M.K., Lobkarev O.A., Prokopyev Ya.V. Prevalence and structure of erectile dysfunction and the role of dynamic cavernosography in its diagnosis // Public health and healthcare. – 2008. – No. 1. – S. 94–98.
- Laurent O.B., Shcheplev P.A., Nesterov S.N., Kuharkin S.A. Modern methods of diagnosis and treatment of erectile dysfunction // Russian Medical Journal. – 2000. – T. 8. – No. 3. – P. 130–134.
- Kurbatov DG, Kuznetsky YY, Kitaev SV, Brusensky VA. Magneticresonance imaging as a potential tool for objective visualization of venous leakage in patients with veno-occlusive erectile dysfunction. Int J Impot Res. 2007;20(2):192-198. doi: 10.1038/ sj.ijir.3901607.
- Patel DV, Halls J, Patel U. Investigation of erectile dysfunction. Br J Radiol. 2012;85(1):69-78. doi: 10.1259/bjr/20361140.
- Kawanishi Y, Izumi K, Muguruma T, et al. Three-dimensional CT cavernosography: reconsidering venous ligationsurgery on the basis of the modern technology. BJU Int. 2011;107(9):1442-1446. doi: 10.1111/j.1464-410X.2010.09644.x.
- Zhukov O.B., Zubarev A.R., Kulchenko N.G. Ultrasound parameters and morphological criteria of veno-occlusive erectile dysfunction in age-related androgen deficiency // Andrology and genital surgery. – 2009. – No. 1. – P. 39–43.
- Zhukov O.B., Efremov E.A., Shcherbinin S.N., et al. Dynamic computer cavernosography in the diagnosis of veno-occlusive erectile dysfunction // Andrology and genital surgery. – 2012. – No. 1. – S. 55–58.
- Zhuravlev V.N., Kogan O.S., Romanenko D.V., et al. Flat-panel computed tomography (CONE-BEAM CT) in the preoperative diagnosis of disorders of the veno-occlusive mechanism in erectile dysfunction // Medical Bulletin of Bashkortostan. – 2013. – T. 8. – No. 2. – S. 293–295.
- Karmazanovsky G.G. Modern computer and magnetic resonance imaging // Computer technologies in medicine. – 1997. – No. 3. – S. 26.
- Zhukov O.B. Diagnosis of erectile dysfunction. Clinical guidelines. – M.: Binom, 2008.
- Bernstein MR, Schnall MD, Stolpen AH. Gadolinium enhanced three dimensional magnetic resonance angiography of pelvic vasculature in posttraumatic impotence / Proceedings of AUA Annual Meeting, Long Beach, CA, USA; 27-29 March 1998.
- Kurbatov D.G., Shchetinin V.V., Kitaev S.V. The role of magnetic resonance imaging in the diagnosis and treatment of vasculogenic erectile dysfunction // Medical visualization. – 2005. – No. 4. – S. 120–127.
- Brusensky V.A. Radiation research methods in the diagnosis of venogenic erectile dysfunction: Dis. ...cand. honey. Sci. – M., 2008. Moscow; 2008. (In Russ.)]
The article was published in the journal “Urological Gazette” 2021 No. 1, pp. 40-46
Topics and tags
erectile disfunction
Magazine
Urological bulletins 2021 No. 1
Comments
To post comments you must log in or register








