Author:
Strokina O. A., therapist, functional diagnostics doctor. December 2020
Synonyms: fibrogastroduodenoscopy (outdated name), endoscopy (current name), “swallow a light bulb.”
The abbreviation FGDS stands for fibrogastroduodenoscopy. The procedure got its name from the first words:
“fibro-” is a study using fiber optics (in this case, inserting a probe) of the esophagus, stomach (i.e. “gastro-”) and duodenum (“duodeno-”), and “-scopy” means “look” .
Today fiberglass is used, but very rarely. In its place came video endoscopy. Therefore, it is more correct to call the procedure video-esophagogastroduodenoscopy, but in the old fashioned way the procedure is called FGDS.
The procedure is one of the most common methods for examining the upper gastrointestinal tract.
FGDS is very unpleasant, but tolerable and practically painless, but it allows the doctor to assess the condition of the esophagus, stomach and duodenum.
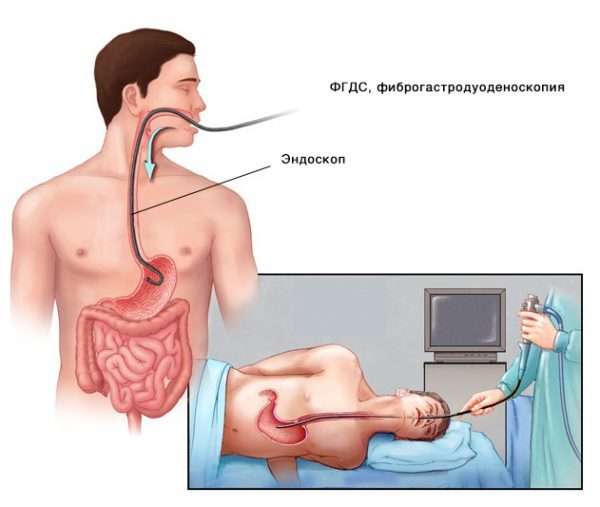
Photo: the process of performing FGDS using an endoscope.
What is FGDS
The abbreviation FGDS in medicine refers to one of the most common methods for studying the upper parts of the digestive system. It stands for fibrogastroduodenoscopy - examination of the mucous membrane of the stomach and duodenum using an endoscope (gastroscope).
Sometimes the procedure is called EGD. The letter E in the name means “esophagus” - esophagus. However, this abbreviation is used less frequently, since FGDS itself already implies examination of the esophagus; the endoscope passes into the stomach through it.
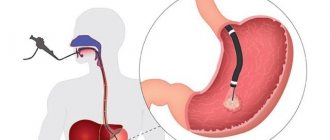
The essence of the technique is that the patient swallows a probe, which, after passing through the mouth, enters the stomach and the initial part of the intestine. At the end of this probe is a miniature light bulb and a camera. The image from the camera is transmitted to a computer screen, after which it is deciphered by a gastroenterologist.
Types of gastroscopy
Options and methods of fibrogastroscopy are given in the table:
| View | Description |
| Classical | It is carried out without anesthesia; the patient swallows a tube after applying an anesthetic spray to the pharyngeal mucosa. Used in most subjects |
| With anesthesia support | Some categories of patients require anesthesia in order to be able to fully carry out the manipulation. A short-term general anesthesia is used, during which the muscles of the pharynx and esophagus relax, allowing the doctor to insert the endoscope |
| Planned | It is carried out by appointment, for patients who do not require an urgent diagnosis. |
| Emergency | It is carried out for vital indications, when it is urgently necessary to determine what happened to a person. The risk of complications increases due to lack of proper preparation |
| Diagnostic | Used only for examining the mucous membrane of the esophagus, stomach and intestines, identifying pathological changes |
| Medical | In addition to the examination, the doctor can carry out the required treatment measures:
|
What diseases are diagnosed
Using gastroscopy, a doctor can diagnose the following diseases:
- various tumor neoplasms - polyps, cysts, cancer of the esophagus or stomach;
- gastritis - erosive, atrophic, hypertrophic;
- gastroesophageal reflux disease;
- Barrett's esophagus;
- Mallory-Weiss syndrome;
- ulcers of various parts of the digestive tract;
- wounds to the mucous membrane.
With the help of endoscopic equipment, dilation of the esophageal veins can be detected, which is one of the signs of liver cirrhosis.
Photo gallery
The photo shows the main nuances of the implementation of FGDS and the detected pathologies

Position of the endoscope in the stomach
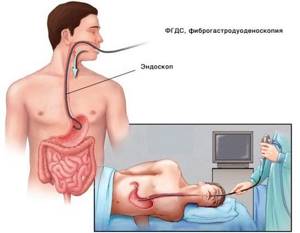
FGDS implementation scheme

Types of pathologies

Biopsy using an endoscope
What parameters are assessed?
During the FGDS, the doctor evaluates the following parameters:
- color of the mucous membrane throughout the examined area of the gastrointestinal tract;
- the presence of folds of the mucous membrane;
- integrity of all shells;
- the presence of inflammatory changes and neoplasms;
- severity of peristalsis.
If there are pathological changes for each item, they are described in the conclusion.
The video describes the FGDS procedure. Filmed by TNT channel.
Fibrogastroscopy
Fibrogastroscopy is the most common way to examine the gastric mucosa by inserting a fibrogastroscope into the organ cavity. This procedure is indicated for patients who are suspected of having gastritis, stomach ulcers, tumors, or polyps. Sometimes FGS is prescribed to identify possible causes of allergies or neuroses; the range of diseases is quite wide. Now the study is carried out in two versions of the probe: through the mouth and through the nose.
FGS with transoral administration
The procedure lasts only a few minutes, and the doctor can announce preliminary results immediately after the manipulation.
The patient is in a reclining position on his stomach, holding a special plastic mouthpiece in his mouth. The gastroenterologist endoscopist passes a probe through it and asks the patient to swallow the tube. Since light anesthesia was administered in advance, his gag reflex is weakened, and the patient does not feel the urge to gag, only discomfort and a sensation of a foreign body.
The advantages of this method include:
- Esophageal dysphagia symptoms
- short duration of the study (only 2-5 minutes);
- quick receipt of visual observation results;
- the ability to manipulate a video camera under eye control to study areas of particular interest;
- the possibility of carrying out therapeutic measures (biopsy, coagulation of bleeding vessels, removal of polyps);
- minimal risk of complications.
The disadvantages of fibrogastroscopy include:
- long period of preparation for the study, dietary restrictions;
- discomfort during gastroscopy;
- a large number of contraindications.
FGS with transnasal administration
This test is not yet widely used; transnasal testing means passing a flexible probe through the nose, along the back of the throat and down the esophagus. Since the fiberscope does not affect the root of the tongue and the uvula of the soft palate, the patient is not bothered by the gag reflex. The patient no longer requires local anesthesia or sedation. If there are allergic reactions to the anesthetic, this will be a separate point in favor of the transnasal method.
Obviously, the tube in this case will be much thinner than with fibrogastroscopy through the mouth. The diameter of the tube should not exceed half a centimeter, which means that the additional capabilities of gastroscopy will be significantly limited (you cannot take a biopsy through a thin channel, you cannot perform coagulation during bleeding). Such a tube is easier to insert, and the quality of the study itself does not deteriorate at all.
Scheme of passing the tube through the nose.
In addition, with the transnasal route of administration, the patient’s verbal functions are preserved; he can immediately report any unpleasant sensations to a specialist, which significantly reduces fear and anxiety before the procedure.
But, like any procedure, transnasal FGS has its drawbacks. Some patients report the appearance of nosebleeds after gastroscopy through the nose.
Advice from the head of the gastroenterology department! Baishev V.M.: “I can recommend only one remedy for the rapid treatment of ulcers and gastritis, which is now recommended by the Ministry of Health...” Read more »
For fibrogastroscopy, regardless of the method of administration, there are a number of contraindications that reduce the versatility of the method. Relative contraindications are temporary; when reduced body functions are restored, they are removed, and FGS becomes possible. In addition, with the development of life-threatening conditions and the need for urgent gastroscopy, you can turn a blind eye to some of these indications. Such restrictions include:
- inflammatory diseases of the ENT organs;
- last trimester of pregnancy;
- burns of the esophagus and oral cavity;
- angina pectoris and advanced arterial hypertension.
Absolute contraindications limit gastroscopy indefinitely. In the presence of varicose veins, severe narrowing, scars of the esophagus, aortic aneurysm and curvature of the spine, FGS is strictly contraindicated.
- What to do if patients experience pain in the throat or stomach after gastroscopy
Indications
The gastroscopy procedure is prescribed if the patient has the following symptoms:
- difficulty swallowing;
- frequent vomiting for no apparent reason;
- admixture in vomited blood;
- constant pain in the stomach area, along the esophagus;
- vague abdominal pain;
- unexplained weight loss;
- sudden loss of appetite;
- untreatable anemia.
For a newborn child, gastroscopy is performed when:
- poor weight gain;
- refusal to eat;
- constant colic;
- other health problems.
Since FGDS is not only a diagnostic, but also a therapeutic procedure, it is prescribed for the following pathological processes:
- foreign body entering the stomach;
- polyposis of the stomach or esophagus;
- consequences of chemical burns of the esophagus;
- stomach bleeding;
- neoplasms of the esophagus or stomach.
For these diseases, the doctor uses a gastroscope to carry out the required medical manipulations.
Interpretation of survey results

This procedure is aimed mainly at studying the secretory function of the stomach. It can be used to diagnose most diseases of the digestive system:
- a clear, non-viscous liquid with normal acidity indicates a completely healthy stomach;
- the predominance of yellow or green in the liquid indicates an admixture of bile, red and brown - an admixture of blood;
- food residues in the pumped out fluid and an increased total volume make it possible to judge hypersecretion of gastric juice;
- increased fluid viscosity indicates the presence of gastritis;
- depending on the content of hydrochloric acid, treatment is directed either to limit its production, or, conversely, to stimulate it;
- The acidity of the stomach is determined: low or high.
Contraindications
The gastroscopy procedure is not performed for all patients - contraindications to FGDS are:
- scoliosis 3-4 degrees;
- severe chest deformities;
- obstructive pulmonary diseases;
- obesity 4 degrees;
- multiple strictures of the esophagus;
- large goiter;
- severe blood clotting pathology;
- cachexia - extreme exhaustion of the body;
- early period after a heart attack or stroke.
The following may also be contraindications:
- the patient’s categorical refusal to undergo the procedure (in this case, the study can be rescheduled);
- state of severe drug or alcohol intoxication;
- acute psychosis.
How is probing carried out?
This diagnostic method takes quite a long time and can last up to two and a half hours. This depends on the condition of the patient and on the procedure used.
It is usually carried out in a standard way:
- First, all its contents are aspirated from the stomach.
- Then, every 10 minutes for an hour, the secretion produced by the stomach on an empty stomach is collected. The fluid collection time is five minutes.
- Afterwards, a so-called test breakfast is introduced into the stomach. This could be cabbage broth, light broth, or medicinal secretion stimulants: insulin, pentagastrin or gestamine. These drugs have their own contraindications for use, so a trial breakfast is now practically not carried out. In addition, it does not give the desired stomach reaction.
- Half an hour after the introduction of breakfast, the secretion caused by stimuli is again selected. The collection is also carried out within an hour at intervals of fifteen minutes.
Each portion of liquid received is tested in the laboratory. The smell, appearance, consistency and total amount of the resulting contents are assessed.
Preparation
In order for the patient to endure the procedure easily psychologically and physically, the doctor tells how to prepare for it.
Nutrition
A person is warned about a planned FGDS 2-3 days in advance. At this time, he follows a special diet and prepares himself mentally for the procedure.
It is recommended to temporarily exclude the following foods from the diet:
- fatty meat and fish dishes;
- mushrooms;
- baking;
- seasonings and spices;
- sausages;
- fatty cheese, milk;
- legumes;
- sweets;
- bread;
- cabbage;
- coffee;
- alcohol.
A person’s menu before an FGDS consists of:
- chicken meat;
- lean fish;
- stewed vegetables;
- porridge with water;
- weak tea.
On the eve of the study, you can eat a light dinner. Since FGDS is usually done in the morning on an empty stomach, you can drink water no later than three hours before the procedure.
General recommendations
Additional proper preparation is carried out taking into account the following nuances:
- a few days before the procedure, it is recommended to quit smoking (or reduce the number of cigarettes as much as possible);
- if a person is forced to take any medications for medical reasons, the doctor who will conduct the FGDS should be notified about this;
- If the tablet needs to be taken in the morning, it is not swallowed, but dissolved in the mouth.
Moral preparation
The moral preparation of the patient is of great importance, because if a person has a strong fear of the upcoming procedure:
- the patient will be nervous, which will prevent him from swallowing the probe;
- the doctor will not be able to fully examine the stomach.
The patient needs to understand that the procedure is painless, so the better the person relaxes, the easier it will be for him to survive the manipulation.
It is important not to be afraid of the upcoming procedure and to set yourself up positively - for this you can:
- meditate on the eve of the study;
- take a sedative;
- talk to a psychologist.
Sometimes gymnastics helps you get into the right mood.
Learning to breathe correctly
During FGDS, the patient is only required to lie still and breathe correctly, while:
- breathing should be carried out only through the nose, without using the intercostal muscles and diaphragm;
- you need to inhale the air slowly and deeply, measuredly;
- It is best to mentally count the rhythm while breathing.
Deep breathing helps you calm down, especially if you are very afraid of pain.
How to reduce your gag reflex
To reduce or alleviate the severity of the gag reflex, first of all, you must strictly follow the doctor’s recommendations.
The urge to vomit during FGDS occurs in a person due to irritation of the root of the tongue with the gastroscope hose, therefore:
- to reduce the sensitivity of nerve endings, this area is irrigated with an anesthetic - lidocaine or ultracaine;
- reduction of muscle tension is achieved by administering muscle relaxants;
- During insertion of the tube, the person must actively swallow the probe - this will reduce the pressure on the root of the tongue.
Description of the procedure
Planned FGDS is prescribed in the morning. The procedure is carried out in an equipped endoscopy room.
Before manipulation, it is necessary to remove objects squeezing the body:
- belts;
- chains;
- tight clothes.
How does the procedure work?
Step-by-step process of the procedure:
- An hour before gastroscopy, the patient is given premedication - 1 ml of atropine and 1 ml of trimeperidine are administered intramuscularly.
- The person is placed on the couch on his left side. You can bend your legs slightly and wrap your arms around yourself at elbow level. Place a tray in front of your face. During the examination, you need to behave correctly - you cannot move, turn your head, swallow saliva, or talk.
- The patient is given a silicone insert to clamp between the teeth, through which the probe is inserted. It is necessary to prevent damage to the gastroscope. If it is impossible to perform the procedure due to the person’s strong tension or a pronounced gag reflex, anesthesia is performed - then it will be painless.
- Next, the doctor inserts a tube into your throat. You need to swallow it while taking a deep breath. When the tube passes through the pharyngeal ring, the discomfort stops.
- The endoscopist examines the internal organs. Sometimes it is possible to go through the intestine completely and examine the place of its transition to the next section.
- After this, the doctor carefully removes the gastroscope tube.
Photo gallery

Full insertion of the probe

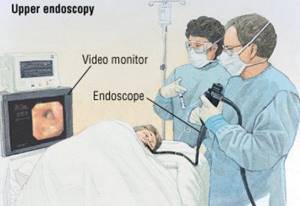
Examination directly through a gastroscope

On-screen inspection

Gastroscopy with anesthesia
Is it painful to swallow a tube and tube?
The gastroscope probe has a diameter of 1.5-2 cm, so it does not cause pain when swallowing. Only discomfort appears from the presence of a foreign object in the throat.
The thickness of the tube for small children is even smaller - 5-10 mm. Therefore, there is no need to worry about pain, because the diameter of the esophagus is much larger and the tube will pass through it absolutely freely.
How often can you do it
Initially, healthy people do not often need to undergo gastroscopy. FGDS is carried out only according to indications, on which the regularity of the manipulation will depend. It is prescribed when appropriate symptoms appear; the further number of examinations depends on the established diagnosis.
If you have uncomplicated gastrointestinal diseases, the test can be taken once a year. Severe pathologies - with complications, rapidly progressing - require gastroscopy every 3-6 months. In most cases, the frequency of FGDS is determined individually.
Testing without swallowing the tube and probe
If it is absolutely impossible to perform a classic gastroscopy, if the patient has contraindications, there is an alternative method of visual examination of the gastrointestinal tract. This is a capsule FGDS - the patient swallows not a tube, but a small chamber in the form of a capsule. It sequentially passes through all parts of the gastrointestinal tract and leaves the body naturally. The data recorded by the camera is then transferred to a computer where the doctor can study it.
This lightweight method is no less informative than classic gastroscopy; it allows you to study not only the upper gastrointestinal tract, but also the entire intestine from the inside. However, it is not performed on all patients. The cost of such a study is very high - together with the capsule itself, the price of the procedure is within 50 thousand rubles.
As with classical gastroscopy, there are several contraindications:
- swallowing disorder;
- installed pacemaker;
- epilepsy;
- intestinal obstruction.
The preparation required is the same as for conventional FGDS. The capsule passes through the entire gastrointestinal tract in 12-14 hours, so the test result is issued the next day.

Capsule FGDS
Features and capabilities of the procedure
Swallowing a probe to check the stomach or FGDS is an endoscopic method for examining the esophagus, stomach and part of the duodenum to confirm suspected tumors, identify sources of bleeding, and generally assess the condition of the mucous membranes. Otherwise, the procedure is called swallowing a light bulb for the stomach.

What is the name of the procedure for swallowing a light bulb for the stomach? The official name of the manipulation is fibroesophagogastroduodenoscopy or FGDS. The procedure is performed using a gastroscope equipped with a long thin probe with a tip. At the end of the tube there is a built-in video camera and lighting device, which transmit the resulting image to a computer monitor.
Possibilities
FGDS combines both diagnostic and therapeutic-diagnostic functions. Fibroesophagogastroduodenoscopy has the following special capabilities:
- detection and management of bleeding sources;
- removal of polyps, tumors;
- treatment of ulcerative-erosive lesions;
- antiseptic treatment of mucous membranes in acute inflammation;
- possibility of taking a biopsy sample for histological analysis.
FGDS allows you to provide emergency care for ulcerative bleeding, suspected perforation of an ulcerative-erosive focus. Biopsy plays an important clinical value in relation to tumor-like neoplasms. The analysis allows you to accurately determine the presence of atypical cancer cells, make prognoses and individual treatment tactics.
Advantages and disadvantages
Fibrogastroscopy has a number of positive and negative aspects, taking into account which the need for it is determined.
The pros and cons of gastroscopy are presented in the table:
| Advantages | Flaws |
|
|