Tracheobronchoscopy (full name of the procedure) is a modern diagnostic and treatment method for visualizing the internal surfaces of the trachea and bronchi.
The examination is performed with a special optical device – a fiberoptic bronchoscope. Essentially, this is a multifunctional endoscope, which consists of a flexible cable with a light source and a video/photo camera at the end and a control handle with an additional manipulator.
The essence of the method
Examination of the mucous membranes of the bronchi and trachea using a bronchoscope is called bronchoscopy.
A special device (bronchoscope), which has a video camera and lighting, is inserted into the patient’s airways for examination. As a result, the doctor accumulates accurate (up to 97%) data. A bronchoscope is used to diagnose various pathologies:
- Bronchitis;
- Pneumonia;
- Lung oncology.
We also use a bronchoscope for therapy, for which it is equipped with the necessary devices.
What can and cannot be done after the procedure?
The patient may experience a feeling of numbness after using the anesthetic, so it is advisable to postpone drinking water and food for a while to avoid choking. 1-2 hours after the procedure, you can drink a few sips of water. If swallowing has been restored and the process does not cause discomfort, you can start eating and drinking.
You should refrain from smoking for 2 hours after bronchoscopy.
You should ask your doctor when you can start taking your medications.
If the study was carried out “in a dream”, then within 24 days after anesthesia the patient will not be able to drive a vehicle, and he will need accompanying persons in order to get home.
A little history
It should be noted that bronchoscopy is not an invention of today. It was first used at the end of the 19th century. At that time, and for many decades later, it was painful, associated with injuries, and caused significant complications.
The first models were equipped with lenses and mirrors, with the help of which the doctor could examine the patient's respiratory tract.
In the mid-50s, the first safety bronchoscope was developed, although it remained rigid. But already in the late 60s the first flexible one appeared. Another 10 years passed, and new technologies made it possible to achieve significant image enlargement. Thus, doctors received a unique opportunity to see any changes in detail.
Indications for bronchoscopy
Bronchoscopy is most often a diagnostic procedure that is done to diagnose lung diseases, tumors, chronic cough, and infections. Depending on the condition and disease of the patient, during bronchoscopy you can find: blood, mucus, signs of an infectious process, swelling, puffiness, the presence of a foreign body, tumor.
Indications for bronchoscopy:
- to detect the cause of the problem (eg, bleeding, chronic cough, difficulty breathing);
- to take tissue samples when other tests, such as a chest X-ray or CT scan, show problems with the lung or lymph nodes in the chest;
- to diagnose lung disease by collecting samples of tissue or mucus (sputum);
- to determine the degree of lung cancer;
- to remove foreign bodies that block the airways;
- for brachytherapy;
- for the diagnosis of bronchial tuberculosis (bronchoscopy is performed for differential diagnosis with other diseases).
Types of bronchoscopy
If we talk about what the procedure might be, we need to start from the goals of its implementation. And this goal happens:
- Diagnostic;
- Therapeutic.
During diagnostic testing, the doctor examines the respiratory tract and takes a biopsy sample for study. This view is indicated for detection:
- Pathologies of the development of the respiratory system;
- Diseases of an infectious and inflammatory nature;
- Tumors;
- Causes of hemoptysis.
The main goal of the therapeutic procedure is to carry out such manipulations as:
- Stop bleeding;
- Removal of tumors;
- Removal of foreign bodies;
- Targeted administration of drugs, etc.
Testicular biopsy
What complications and consequences can occur after bronchoscopy?
With bronchoscopy, the risk of complications increases with the patient's age. Therefore, before prescribing the procedure, the doctor carefully assesses the health status of each patient, weighs the benefits and possible risks.
After bronchoscopy, the patient may experience a sore throat and hoarseness for several days. Often the day after bronchoscopy, there is a desire to cough. These phenomena go away on their own.
In rare cases, a bronchoscope can injure surrounding tissues, which causes a sore throat, difficulty swallowing, can cause hoarseness or coughing, provoke nosebleeds, and extremely rarely, injury to the larynx occurs.
If the patient has had a biopsy, coughing up a small amount of blood may occur in the first couple of days after bronchoscopy. If severe bleeding occurs, consult a doctor immediately. Stopping such bleeding is done using an endoscope.
Rigid and flexible devices
Today, both rigid and flexible bronchoscopes are used in medical practice. Both have their own advantages, as well as areas of application.
Bronchoscope rigid:
- It is mainly used for therapy. Unlike a flexible device, it expands the lumen of the bronchi and can be used to remove foreign bodies;
- A flexible bronchoscope can also be inserted through the device, which is important for examining thinner bronchi;
- Using the device, the doctor can eliminate detected pathologies;
- Widely used for resuscitation purposes, for example, in case of drowning;
- General anesthesia is required, then the patient has no fear or discomfort.
Flexible bronchoscope:
- Less traumatic;
- Reaches parts of the bronchi that are inaccessible to the rigid apparatus;
- Used in pediatrics;
- General anesthesia is not required.
Manipulations with flexible apparatus
Today, a flexible bronchoscope is used more often, especially for diagnostics.
Six hours before the procedure you should not drink or eat.
The procedure is carried out in compliance with high sterility.
A patient who is in a supine or sitting position. For relaxation, a drug is administered, for example, Eufilin. Relaxation of the patient's body is important for the advancement of the device.
The patient should breathe shallowly, often: this neutralizes the gag reflex.
The device is inserted through the mouth or nostril. At the moment of deep inspiration, it is carried out through the glottis. Then they are moved into the bronchi by rotation.
The patient may feel pressure in breathing, but not pain.
First, the larynx and glottis are examined, then the trachea and bronchi. Thin bronchioles and alveoli of the lungs are inaccessible to the device.
The doctor gets the opportunity:
- Rinse the bronchi;
- Delete their contents;
- Carry out a biopsy, etc.
The patient feels numb for half an hour after the procedure. For the next two to three hours, he should not smoke or eat, nor should he drive a vehicle for eight to ten hours.
Ultrasound during pregnancy
- No preparation required.
Ultrasound of the abdominal organs (liver, gall bladder, pancreas, spleen)
- Remove from your diet foods that cause increased gas formation (legumes, black bread, cabbage, milk, eggs, carbonated drinks, including beer, champagne).
- For flatulence, recommend chamomile infusion 2 times a day or activated carbon 1-2 tablets x 4 times a day. The study is carried out strictly on an empty stomach.
Ultrasound of the pelvic organs (bladder, uterus, appendages)
- Eliminate gas-causing foods (legumes, brown bread, cabbage, milk) from the diet 2-3 days before the test.
- The study is carried out on an empty stomach.
- If the ultrasound is performed transabdominally, then on the day of the examination, 2-3 hours before the ultrasound, the patient should drink about 1.5 liters of non-carbonated liquid (tea, water, juice), and not urinate before the examination.
Ultrasound of the prostate
- The day before, do not eat raw vegetables, fruits, or milk.
- If there is bloating in the abdomen, for better visualization, it is advisable to take espumisan 5 capsules 3 times a day and 6 capsules in the morning on the day of the study. If you did not take espumizan the day before the test, then take 10 capsules at once 3 hours before the test.
- Come with a full bladder (drink 0.3 liters of liquid 2 hours before the examination).
Ultrasound of the rectum
- On the eve of the study, drink any laxative, 2 cleansing enemas in the evening and in the morning.
- An hour before the test, drink 500-600 ml of liquid to fill the bladder.
Ultrasound of the renal arteries
- It is carried out on an empty stomach.
- It is advisable not to eat gas-forming foods (legumes, brown bread, cabbage, milk) the day before.
X-ray examination of the kidneys (excretory intravenous urography):
- Eliminate from the diet foods that contribute to gas formation (vegetables, fruits, sweets, milk, brown bread). As prescribed by a doctor, carbonene, activated carbon.
- Limit fluid intake to 1 liter from the afternoon before the test.
- Cleansing enemas morning and evening.
X-ray examination of the urinary tract:
- Three days before the test, exclude from food: vegetables, fruits, brown bread, dairy products. Stool should be regular (if there are problems with stool, correct it by taking laxatives).
- Limit fluid intake the day before the test to 1.0-1.5 liters. Espumisan 2 days before the study according to the regimen, see the annotations.
- On the day of the study, have a light breakfast in the morning.
Computed tomography with contrast
When performing computed tomography with contrast or with bolus contrast, the following examinations are necessary:
- Blood biochemistry (creatinine, urea)
- Consultation with an allergist (allergy to iodine-containing drugs)
When conducting an examination of the pelvic organs, first contact a doctor for consultation.
Computed tomography of the abdominal cavity, retroperitoneal space
- Be sure to eat before the test.
- 15 minutes before the examination, the patient is asked to drink an iodine-containing non-ionic contrast agent, after which the contrast is administered intravenously.
- If the patient underwent an X-ray examination of the digestive tract with barium contrast, a computed tomography scan can be performed no earlier than 7 days.
Bronchoscopy
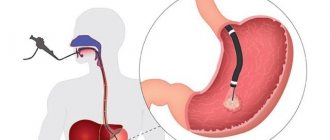
Bronchoscopy (from the ancient Greek βρόγχος - windpipe, trachea and σκοπέω - look, examine, observe), also called tracheobronchoscopy, is a method of direct examination and assessment of the condition of the mucous membranes of the tracheobronchial tree: trachea and bronchi, if indicated, and the larynx using a special device - fiber bronchoscope or video bronchoscope - the latest generation of endoscopes. A modern bronchoscope is a complex device consisting of a flexible rod with a controlled bend of the far end, a control handle and a lighting cable connecting the endoscope to a light source, equipped with a video camera, as well as manipulators for performing a biopsy and removing foreign bodies.
It is one of the most informative instrumental methods for studying the trachea and bronchi, and, if necessary, the larynx, and is used to visually assess the condition of the tracheobronchial tree, identify endoscopic symptoms of lung diseases, and obtain material for laboratory research. Bronchoscopy is performed: on patients in preparation for lung surgery, during treatment of bronchopulmonary diseases to clarify the diagnosis, develop treatment tactics, and monitor the effectiveness of treatment. For bronchitis with abundant sputum, therapeutic BS is used to remove contents from the bronchi and administer medications. Bronchoscopy is important in the diagnosis of early forms of cancer of the larynx, trachea, and bronchi; it is actively used to identify and remove foreign bodies from the bronchial tree if they are accidentally inhaled (aspirated).
Preparing for the study:
Before bronchoscopy, an X-ray examination or computed tomography of the chest organs, or fluorography, ECG must be performed - bring these tests and an outpatient card with you. The endoscopist must be aware of the presence of diseases in the patient being examined (for example, diabetes mellitus, coronary heart disease, a history of heart attack, hormone therapy, treatment with antidepressants) and the presence of allergies to medications. Bronchoscopy is performed strictly on an empty stomach to avoid accidental release of food or liquid into the respiratory tract during vomiting or coughing, so the last meal should be no later than 19.00 on the eve of the study. On the day of the study, do not drink water. You should consult the doctor who prescribed bronchoscopy about taking mandatory medications (heart medications, to lower blood pressure), and warn the endoscopist about this. Bronchoscopy is performed in rooms specially designed for this purpose. It is recommended to take a towel with you, as you may expect to cough up mucus after the procedure.
During the study:
- Everything possible will be done to ensure that the Patient endures it as easily as possible.
- It is necessary to remove dentures and piercing jewelry.
- Patients with a bronchospastic component (chronic obstructive bronchitis, bronchial asthma) immediately before the start of anesthesia, if necessary, are allowed to inhale an aerosol (salbutamol) from an individual dispenser.
- it is necessary to remove outer clothing or loosen the collar (unfasten the buttons).
- Local anesthesia is performed on the nasal mucosa and oropharynx to eliminate pain when passing the endoscope through the nose and suppress the cough reflex. Bronchoscopy is performed in a sitting position. The doctor inserts an endoscope into the airways under visual control, gradually examining the underlying sections of the tracheobronchial tree on both sides. The device is usually inserted through the nasal passage, but in some cases it can be inserted into the respiratory tract and through the mouth. The diameter of the endoscope is significantly smaller than the lumen of the trachea and bronchi, so there should be no breathing difficulties. The doctor examines the surface of the pharynx, larynx, trachea and bronchi. The bronchoscope is then removed.
Possible complications:
- The examination ahead of you is an invasive instrumental intervention and, despite the relatively low level of side effects and the most gentle execution, it still carries the risk of some complications: among them are damage to the bronchial wall, pneumothorax, bleeding after a biopsy, bronchospasm, pneumonia, allergic reactions .
If the above complications occur, hospitalization and surgical treatment may be required.
After the end of the intervention:
- There remains a feeling of numbness, slight nasal congestion, a feeling of a “lump” in the throat and a slight difficulty in swallowing saliva that occurs as a result of anesthesia. These sensations pass within an hour.
- You can eat after the sensation of numbness in the tongue and throat has completely passed to prevent food and liquid from entering the trachea. If a biopsy was performed, the doctor will determine the timing of meals.
Fibercolonoscopy
Colonoscopy is the most accurate and reliable method for diagnosing changes in the mucous membrane of the colon using an endoscope - video colonoscope; the true nature of the pathological process is established in almost 100% of cases. A colonoscope is a flexible long probe with a built-in video chip that allows you to transmit a color image from inside the intestine to a monitor, makes it possible to see changed areas of the mucous membrane, examine and evaluate their structure in detail, give an opinion on the presumptive diagnosis and, if necessary, take a piece for histological examination (biopsy ). The study is carried out according to indications determined by the attending physician or consultant physician.
Indications:
- detection of inflammatory changes, diverticula, polyps
- suspected colon tumor
- diagnostics (for screening purposes) in the absence of complaints
- as preoperative preparation
- for the purpose of monitoring over time - after conservative or surgical treatment.
Preparing for the study:
Colonoscopy is the leading method of examining the colon, so bowel preparation for colonoscopy plays a key role in the examination, along with the technique of inserting the endoscope and examination. Only with good preparation of the intestines for examination during the procedure, it is possible to identify the smallest, barely noticeable changes in the mucous membrane and make a diagnosis at an early stage, which contributes to a complete cure for the most serious diseases.
2-3 days before cleansing the colon, a slag-free diet is prescribed: fiber-rich plant foods and poorly digestible foods should not be taken; you can - refined and easily digestible low-fat protein products, clear liquid in unlimited quantities (broths, juices without pulp, tea, jelly without berries)
1. Preparation on the eve of the study is possible: in 2 ways
- A modern method of cleaning by taking one of the drugs:
- Fortrans - 1 packet per 20 kg of weight, dilute 1 packet in 1 liter of drinking water. take 1 hour in fractions, you can with citrus juice; if the study is after 12 noon, then 2l in the evening, 2l in the morning; if the study is before 12 noon, then the entire volume should be taken from 16 to 20 hours. Read the instructions carefully.
- Moviprep - in a package there are 2 packages A and 2 packages B. Dilute 1A and 1B in 1 liter of drinking water, take 1 hour + 500 ml of any clear liquid, after an hour repeat the same with the remaining packages. Follow the instructions.
- Flit phospho-soda - in the morning and evening, 1 bottle of 45 ml of flit phospho-soda mixed with water, take at least 2 liters of clear liquid during the day, read the instructions carefully.
- Picoprep – 2 packets are dissolved in water (150 ml each) and washed down with a clear liquid, according to the instructions.
2. Traditional method of preparation with laxatives and enemas: at 15-16 hours 30-45 ml (no more than 70 ml) of castor oil or any other laxative (senna tablets, bisacodyl, 25% aqueous solution of magnesium sulfate (200 ml); in the evening after passing stool, do 2 cleansing enemas of 1.5-2 liters each, in the morning, no later than 2 hours before the examination, 2 more cleansing enemas of 1-2 liters each with an interval of 1 hour.
Attention! Taking mandatory medications (hormonal, to lower blood pressure, cardiac and others) should not be canceled! Discontinue iron supplements 3-4 days before the colonoscopy. For chronic constipation or after irrigoscopy, start a slag-free diet 5 days before the test!
You must have a sheet with you, an outpatient card (required extracts, an irrigoscopy report if done.
The average duration of the examination is 30 minutes, but its duration depends on many factors, such as the quality of preparation of the colon, the anatomical features of the organ, previous operations, and individual intolerance to the examination. The procedure time may increase due to additional interventions - diagnostic or therapeutic.
Colonoscopy begins in a lying position on the left side; during the examination, it is possible to change the position of the body - turning on the back or on the right side. The device passes through the anus into the rectum, then into the colon and blind. During the examination, air is pumped into the intestinal lumen, this ensures straightening of the lumen and folds of the colon, clear visibility of the relief of the walls, mucous membrane, vascular pattern, etc. Inspection of the colon is performed both during the insertion of the device and during its removal. Sometimes during the procedure, unpleasant pain may occur. This can be caused by a number of reasons: previous operations on the abdominal cavity and the presence of adhesions, anatomical features of the intestine - the presence of “sharp” bends and additional loops, elongation of the organ (dolichosigma, dolichocolon).
Possible complications: the endoscopic examination you are undergoing is an invasive instrumental intervention and, despite the relatively low level of side effects and the most gentle execution, it still carries the risk of some complications, among them are:
- traumatic damage to the intestinal wall (perforation) with possible secondary infection;
- diverticulum rupture due to diverticulosis (possible both during preparation and during the study);
- bleeding;
- from the cardiovascular system (palpitations, ↓ or ↑ blood pressure, shortness of breath, numbness of the hands, dizziness);
- bloating, belching air;
- inversion of the apparatus with retrograde implementation into the wall of the organ;
If the above complications occur, hospitalization with possible surgical intervention may be required.
After completing the study:
- You may feel bloated for some time;
- You can drink and eat after 30 minutes;
- if a biopsy was performed, then exclude physical activity during the day;
- after intravenous anesthesia, you cannot operate the machine or mechanisms for 24 hours;
- If unusual symptoms or any circumstances that worry you appear during the first hours or days after a colonoscopy, you must contact a doctor at the institution where the examination was performed.
The doctor issues a colonoscopy report on the same day; if a biopsy was taken, the result will be ready in 2 weeks, the staff will explain when and where to pick up the result.
Esophagogastroduodenoscopy (EFGDS)
Esophagogastroduodenoscopy, endoscopy or gastroscopy is one of the types of endoscopic examination - examination of the esophagus, stomach cavity and duodenum using a special device - a fiber gastroscope, inserted into the stomach through the mouth and esophagus. During the examination, possible pathological changes in the mucous membrane are identified.
Endoscopy of internal organs is one of the most accurate and objective research methods and is widely used in the work of specialists in all major areas. Unlike other diagnostic methods, it allows you to see what hollow organs look like from the inside. These are the places where neoplasms can develop, which at the initial stage occur without specific symptoms. For a tumor to appear on an x-ray or ultrasound machine screen, it must already be large enough. And endoscopic diagnosis allows you to notice suspicious signs of a serious pathology at the initial stage, and if necessary, take a piece for examination under a microscope (biopsy).
Preparation:
- It is carried out strictly on an empty stomach - eating and smoking are completely excluded 8-10-12 hours before the test.
- If you are constantly taking vital medications that cannot be interrupted, do not break the regimen, but warn your doctor about this.
- We ask you to arrive for the procedure at the appointed time with medical documents (extracts, previous reports), a towel.
You will be met at the department by a nurse and a doctor; they will help you prepare for the study and will carry it out competently.
During the study: everything possible will be done to ensure that the Patient endures it as easily as possible. Dentures and piercing jewelry must be removed. To reduce sensitivity when swallowing, the Patient may have a local anesthetic solution sprayed into the throat (if tolerated). The patient will be asked to hold a mouthpiece between his teeth, through which the endoscope is passed. The patient will be asked to relax their throat, then take one sip, during which the doctor, under visual control, will insert the device into the esophagus. The doctor will carefully examine the inner surface of the stomach and, if necessary, take a piece of the mucous membrane for further examination (biopsy). This is also a painless procedure. The endoscopist must be aware of the presence of diseases in the patient being examined (for example, diabetes mellitus, hypertension) and allergies to drugs.
Possible complications:
The endoscopic examination ahead of you is an invasive instrumental intervention and, despite the relatively low level of side effects and the most gentle implementation, still carries the risk of some complications:
- organ perforation - traumatic damage to organs with secondary infection;
- bleeding;
- functional disorders of organs and systems (difficulty breathing, cardiac arrest);
- cardiovascular disorders;
- allergic reaction, development of anaphylactic shock;
- tooth damage;
- phlebitis; exacerbation of a chronic disease;
- looping of the endoscope and retrograde insertion of its end into the organ being examined;
- others described in special medical literature;
If the above complications occur, hospitalization and surgical treatment may be required.
After the end of the intervention: you should not eat or drink anything for 30 minutes; If a biopsy was performed, eat refrigerated food during the day. It is not recommended to drive a car or operate any machinery for 1 hour. Inform your doctor about the appearance of unusual symptoms and any circumstances that worry you in the first hours and days after the study. The unpleasant sensation in the throat that occurs in some patients usually goes away within 24-48 hours.
Spirography
- It is recommended to refrain from smoking and drinking coffee at least an hour before the test.
- 8-10 hours before the test you should refrain from taking bronchodilators.
- The examination is carried out in the morning on an empty stomach, after 15-20 minutes of rest.
Bicycle ergometry
- You must refrain from eating at least 3 hours before the test.
- Bicycle ergometry is not performed after stressful situations and heavy physical exertion.
ECG
- Hygienic shower before the examination.
- For men with significant chest hair, it is necessary to shave the hair (check with your doctor).
- A heavy meal is not recommended before an ECG.
- The examination is carried out after 15-20 minutes of rest.
Daily monitoring
- It is recommended to take a shower, because... After installing the electrodes, you will not be able to take water procedures for 24 hours.
- For men, remove (if necessary) hair from the front of the chest.
Biochemical blood test
Blood is drawn on an empty stomach. 12 hours before the test, you must refrain from eating, drinking alcohol and smoking; taking medications is discussed with your doctor. Limit physical and emotional activity for 20-30 minutes. It is not recommended to take blood for research immediately after physiotherapeutic procedures, X-ray examinations, after taking alcohol, drugs (with the exception of a special examination for the presence of these components in the blood). It is very important that you follow these recommendations exactly because... Only in this case will reliable results of blood tests be obtained.
Urine examination In the morning, you need to wash the external genitalia and perineum with warm water and soap in a certain sequence (pubic area, external genitalia, perineum, anus) and wipe the skin dry in the same order. After the hygiene procedure, the patient must release an initial portion of urine into the toilet, and then collect 150-200 ml of urine in a jar (the so-called average portion of the urine stream). The most informative is the analysis of urine collected in the morning after sleep, since the first morning portion of urine is usually the most concentrated. Containers with a lid for collecting urine must be prepared in advance: washed with a detergent solution or soap, rinsed at least 3 times to remove residual detergent and dried thoroughly. Urine collected for research must be delivered to the laboratory no later than 1 hour after collection. Storing urine before analysis is only allowed in the refrigerator for a maximum of 1.5 hours. Features of urine collection using various research methods:
- General urine analysis: after the hygienic procedure, an average portion of urine (150-200 ml) is collected in a clean container.
- Test according to Nechiporenko: after the hygienic procedure, an average portion of urine (40 ml) is collected in a clean container.
- Zimnitsky test: The patient must urinate in the toilet at 6 a.m., then sequentially collect urine in numbered containers, changing them every 3 hours. If there is no urine within 3 hours, the container remains empty. All eight containers must be labeled indicating the portion number and time of urine collection:
- 06.00-09.00;
- 09.00-12.00;
- 12.00-15.00;
- 15.00-18.00;
- 18.00-21.00;
- 21.00-24.00;
- 24.00-03.00;
- 03.00-06.00.
- Bacteriological examination of urine: after the hygienic procedure, collect 10-15 ml of urine from the middle portion into a sterile test tube and immediately close it with a stopper.
- Collection of daily urine: the patient must urinate in the toilet at 8 a.m., then collect urine in a graduated container or three-liter jar for 24 hours until 8 a.m. the next day inclusive. If you plan to analyze 24-hour urine for glucose, protein, etc., after collecting urine, you need to measure the total amount of urine and indicate it in the direction, then thoroughly stir all the urine with a wooden stick and pour 100-150 ml of urine into a bottle for the laboratory.
Examination of sputum Sputum is a pathological secretion released from the respiratory tract when coughing. To collect sputum, the patient should brush his teeth at 8 a.m. on an empty stomach and rinse his mouth thoroughly with boiled water. Then you need to take a few deep breaths or wait for the urge to cough, then cough up the sputum (in a volume of 3-5 ml) into a previously prepared clean, dry, graduated jar and close it with a lid. To collect sputum for the purpose of bacteriological examination, a sterile container is provided; in this case, the patient must be warned not to touch the edges of the dishes with his hands or mouth. When collecting sputum for atypical cells, it is necessary to immediately deliver the material to the laboratory, since tumor cells are quickly destroyed.
Stool is collected in clean, dry plastic or glass containers with hermetically sealed lids. It is unacceptable to deliver feces for examination in matchboxes or cardboard boxes. Rules for collecting feces Feces should not contain foreign impurities (urine, discharge from the genitourinary organs). You should not collect feces after enemas. If it is necessary to know the exact amount of feces, then the empty container is weighed before and after collecting the material. The patient is advised to urinate into the toilet, then by natural defecation, feces are collected in a bedpan or pot (be careful not to get any urine). For the study, 10-15 g of feces is enough. Feces taken from different places, in the amount of 1 g, are collected in a clean, dry container. No special preparation is required for parasitological studies of feces. 10-15 grams are collected with a spoon. warm stool taken from different places. Feces should be delivered to the laboratory within 8 hours after collection (in a hospital setting - within 1 hour). Stool is examined no later than 8-12 hours after its excretion, and before that it is stored at a temperature of 3 to 5 °C. The most accurate idea of the functional state of the digestive tract is provided by a three-time examination of feces.
Contraindications
They are related to the general condition of a person. If it is severe, the procedure is postponed.
The procedure cannot be performed if:
- Serious arrhythmia that cannot be corrected;
- Acute respiratory failure.
The procedure is performed with careful caution in patients with:
- Pulmonary hypertension;
- Vena cava syndrome;
- Severe uremia;
- Problems with blood clotting.
There are practically no obvious complications after the procedure. However, they can occur in older people, as well as in people with serious illnesses.