08/31/2020 Dental treatment with anesthesia during breastfeeding
Dental problems can occur at any age. Everyone is familiar with unbearable toothache that prevents us from living normally. Attempts to remove it provide only temporary relief, but a dentist can truly help. Our article will discuss whether teeth are treated during breastfeeding, how to do it so as not to harm the baby. From it you will learn the causes of dental diseases, whether you can visit the dentist during breastfeeding, and most importantly, whether you can continue feeding breasts while visiting the dentist.
Causes of dental diseases
Tooth enamel is one of the strongest materials in the human body, but under the influence of various factors, even it begins to break down. The main cause of dental disease is the activity of bacteria that cause caries. They absorb carbohydrates and in return release lactic acid, which destroys teeth. A “hole” in a tooth is formed when, in a small space of the tooth, food that has entered there is processed by many bacteria, thereby releasing a large amount of acid.
This is not the only cause of dental disease. The causes are divided into congenital and acquired. In the first case, we are talking about teeth that have not yet grown. If the child’s mother suffered a serious illness during pregnancy or received insufficient nutrition, then the child’s teeth will be weak and susceptible to disease. Heredity can also be included in this category.
In the second case, we are talking about factors affecting dental health, such as:
- absorption of excess fluoride;
- mechanical damage;
- insufficient oral care;
- taking medications;
- lack of calcium or vitamin D.
Is it possible to visit the dentist during breastfeeding?
Often women encounter dental problems even during pregnancy, this is due to the fact that all valuable microelements are spent on the formation and development of the fetus, and calcium deficiency begins in the mother’s body. Lactation continues to aggravate the situation, but the woman is afraid to go to the dentist so as not to harm the child. In fact, it is not only possible to treat teeth, but also necessary! Here are several reasons for this.
Constant pain affects a person’s psycho-emotional state. The mother becomes nervous and irritable, which can directly affect the amount of milk, up to its complete disappearance.
How to prepare for treatment?
The main problem that arises before going to the dentist is fear. The best preparation is to find a good doctor whom the woman can trust. Treatment requires a positive attitude, as increased emotional irritability can affect the effect of anesthesia.
Be sure to feed your baby before going to the doctor, as the first milk after treatment should be expressed.
If serious treatment is planned, you must consult with the doctor who is observing you. He may advise you to stop breastfeeding, but do not stop without your doctor's advice.
If you had to stop breastfeeding, do not use a pacifier; the baby may get used to it and not take the breast. Also, to maintain lactation, milk must be expressed.
How often can an x-ray be taken?
In this case, we are talking about preventive examinations. When we mean treatment, the permissible dose will be higher. How to understand what these dosages are? What can these 1000 μSv be compared to? This indicator is equal to the radiation of 500 images on a computer radiovisiograph or 100 images on high-quality X-ray equipment. One thousand microsieverts is 80 digital photographs. Which of us exposes our body to so much radiation per year?
Any radiation is harmful to the body. But the development of diseases occurs only with a high dose of radiation. A dental X-ray affects a person in such small doses that it cannot provoke pathological processes. If the patient has doubts, it is necessary to consult a doctor. However, you should understand how important such a diagnosis is, and what health problems may arise if you refuse it.
https://www.youtube.com/watch?v=kQ3GeFSIB1s
From all of the above, we can conclude: do not be afraid to take an x-ray if the dentist sends you for an x-ray.
Basic principles
The main principle that guides the attending physician is to determine the optimal interval between feeding and removal of the anesthetic from the mother’s body.
The half-life of a modern anesthetic is at least 20 minutes. After two hours, the concentration of the drug in the body is no more than 1-2%, the risk of exposure to the child is minimized.
It happens that a tooth needs not only to be treated, but to be removed. If you have inflammatory diseases such as tonsillitis, stomatitis, oral candidiasis, gingivitis, colds, flu, tooth extraction is contraindicated!
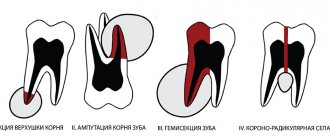
Before removal, the following procedures must be carried out:
- the doctor collects anamnesis;
- takes x-rays;
- identifies contraindications;
- collects tests.
After removal, the doctor will tell you how long not to feed the child. The hole will hurt on the first day; you can take painkillers, but only after the recommendation of a doctor. If the removal is accompanied by a purulent process, the doctor will prescribe antibiotics, and the doctor will decide whether breastfeeding can be continued or should be interrupted .
If treatment with painkillers is safe, then bleaching is not such a harmless method. Whitening is more of a cosmetic than a medical procedure, but many mothers wonder whether it is safe to do it during lactation. The procedure is harmful not so much because of the drugs used for whitening, but because the teeth are already weakened during this period.
After bleaching, it takes time to restore the enamel, and since insufficient amounts of calcium enter the mother’s body during breastfeeding, the process may be delayed. The whitening procedure during this period can harm the teeth and lead to caries.
Impact of X-rays on lactation
If the doctor ordered an x-ray, then do not be alarmed:
- During the procedure, only the jaw and a little face are irradiated;
- protective elements are put on the chest that do not allow rays to pass through;
- The radiation dose is too small to affect the body as a whole and the quality of milk in particular.
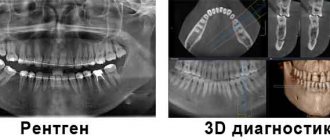
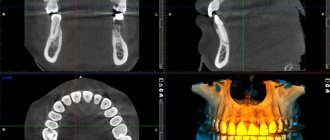
When X-rays, OPTG and CT may be required
An x-ray is a targeted photograph of one or more teeth. OPTG or orthopantomogram is a panoramic image that captures both jaws. CT is a computer tomogram. It allows you to obtain three-dimensional or volumetric images of the entire human jaw system. Each of these types of diagnostics is used for certain indications:
- X-rays are performed when treating a specific tooth: in the presence of caries, pulpitis, periodontitis, suspected cyst or granuloma. Allows you to determine the extent of tooth damage, as well as the condition of the tissues around the root,
- An orthopantomogram is indispensable in the presence of inflammatory processes in periodontal tissues and jaw bone. It is carried out both during multiple dental treatment and in preparation for orthopedic, orthodontic treatment or dental implantation. Allows you to assess the condition and volume of bone tissue, clarify the position of the maxillary (nasal) sinuses of the upper jaw, nerves and other anatomically important elements,
- CT scan is performed for certain indications. Most often in the presence of tumors of the jaw system (to determine their volume in all dimensions), as well as before dental implantation, especially in complex cases.
Today in dentistry (and in medicine in general) digital devices are used instead of film ones. They have a much lighter load, and they also use shorter shutter speeds to create a photo. For comparison: a modern digital visiograph takes up to 0.3 seconds to take an image, a film X-ray machine requires up to 1.5 seconds.
The Smile-at-Once clinic uses the latest generation CT-Scan tomograph. It allows you to get both a targeted or panoramic, and a three-dimensional digital image. Thanks to minimal radiation exposure, the equipment is completely safe and allows repeated diagnostics without harm to the human body.
Komarovsky's opinion
The famous pediatrician Evgeniy Olegovich also touched upon the topic of dental treatment during pregnancy and lactation. He is sure that if the mother took insufficient amounts of calcium-containing medications, then the dental problem will worsen during lactation.
It is necessary to treat teeth, especially if a woman is overcome by severe pain, it promotes the production of adrenaline, which can adversely affect the fetus and the availability of milk. Komarovsky also draws attention to the need to inform your attending physician about your situation.
Orthopantomogram - panoramic image of teeth
Obtaining images during X-ray diagnostics is based on the fact that different human tissues and organs absorb X-ray radiation with different intensities. The image is formed either on a specially prepared film similar to that used in photography, or on a sensor connected to a computer.
A panoramic photograph of the jaw is performed using a special X-ray machine - an orthopantomograph - which can be either film or digital. After dental x-rays, panoramic images can be printed using a digital orthopantomograph. At Dial-Dent, a panoramic image of the teeth is taken digitally, the image is entered into the patient’s computer record, and any clinic specialist can quickly view it to clarify the diagnosis and plan treatment.
There is no need to develop films, which ensures fast image acquisition, eliminates the need to work with chemicals, and also eliminates the need for repeated x-rays in case of poor-quality development.
It becomes possible to further examine the resulting images by enlarging individual areas using software.
Possibility of convenient archiving and quick access to the database with images.
Immediate transfer to the attending physician located outside the clinic.
Convenient storage in the form of files.
Prevention
It is easier to prevent any disease than to treat it later, this is especially true for nursing mothers who are prohibited from a number of medications. Measures to prevent dental diseases:
- Oral hygiene is the key to health;
- see your dentist regularly; pregnant and lactating women need examinations more often, as their bodies are weakened and susceptible to diseases;
- use floss and mouth rinse after every meal;
- choose pastes with fluoride;
- take vitamin complexes containing calcium and vitamin D, but strictly on the recommendation of a doctor;
- eat foods containing calcium and vitamin D;
- change your toothbrush at least once a month;
These are basic tips and recommendations for preventing oral diseases.
To summarize, we can say that you need to treat your teeth even if you are a nursing mother, especially if you are experiencing unbearable pain. If the tooth does not yet hurt, you should not allow caries to destroy the deep tissues of the tooth, especially since modern anesthetics are low-toxic, are quickly eliminated from the body and do not affect milk.
The main thing is to coordinate all actions with your doctor, be sure to inform the dentist that you are breastfeeding and get ready for treatment. Stress is harmful to the mother and has a negative effect on her milk, and can also reduce the effectiveness of pain medications. Prevention is the best cure for disease!
Dental treatment during lactation
The lactation period is not a contraindication for dental treatment. Without treating emerging caries or ignoring the pain, you can start irreversible processes in the oral cavity. Dental treatment while breastfeeding involves some prohibitions (taking antibiotics, implantation), but most often it is absolutely harmless. Otherwise, there is a risk of early tooth loss and the appearance of severe inflammatory processes, as a result of which lactation will have to be stopped urgently.
Having taken care of the oral cavity during pregnancy and getting rid of caries and other problems, you can forget about it during lactation. The well-known doctor Komarovsky recommends that you undergo treatment in the second trimester.
What can and cannot be done during breastfeeding?
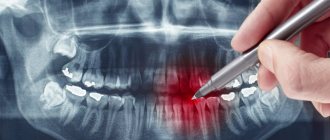
X-ray of a tooth
Dental X-rays are not contraindicated for nursing mothers. Doctors use a special protective apron that will save the baby from getting harmful compounds into the body through milk. After the procedure is completed, you need to express all the milk and pour it out, and at the next flush you can feed the baby. There is no need to worry if your milk supply decreases slightly after the x-ray. This is normal, so lactation will resume after some time.
Treatment of caries or pulpitis
Treatment of caries, and even more so pulpitis, during breastfeeding is a necessary measure. Mechanical impact on the teeth of a nursing mother is not recommended in only one case: if she is in an unstable mental state caused by severe fatigue.
- To eliminate pain, it is not prohibited to use anesthesia (Lidocaine, Ultracaine). It is worth remembering that modern drugs not only have a short half-life, but also do not affect the child in any way, since they pass into milk in small quantities.
- If further treatment requires antibiotics, you should consult your doctor. Antibacterial drugs can affect the baby's health, so breastfeeding will most likely have to be stopped.
Wisdom tooth removal
During breastfeeding, tooth extraction, including wisdom teeth, is allowed. As a rule, for such dental interventions the same type of anesthesia is used as for filling. Modern drugs relieve the patient of pain and allow the tooth to be pulled out without discomfort.
Another question is if there is a need for antibiotics. The doctor must select the appropriate treatment and prescribe medications for the mother that are safe for her and the baby. The main thing is to warn the dentist about breastfeeding in advance.
Enamel whitening
A nursing mother should not endure toothache and caries. However, it is completely different when it comes to a cosmetic procedure such as whitening. It is not recommended to do it during lactation, since the recovery period after enamel whitening takes much longer than in non-breastfeeding women. There is a risk of complications and caries on bleached teeth due to insufficient amounts of calcium absorbed by the mother's body.
Whitening using special equipment can be replaced with toothpastes and professional gels designed for this purpose. Chewing gum is not prohibited. More serious intervention can damage tooth enamel, so you should forget about the Hollywood smile for a while.
X-ray of a tooth while breastfeeding
Severe weakness, headache, high temperature...I feel so bad! The baby immediately began to cry - it’s time to feed... is it possible, what if it’s dangerous?
No matter how wonderfully breastfeeding is organized, no matter how well it turns out, many are faced with such a problem as illness of the nursing mother. It is no secret that just 20 years ago, the recommendations of our doctors in these cases were unambiguous - you should not breastfeed if you are ill! However, since the mid-80s, attitudes towards breastfeeding have undergone dramatic changes. The composition of breast milk and its protective properties were practically re-examined. At the same time, all methodological omissions of previous years were taken into account. By 1989, modern views on feeding children, including those for various maternal diseases, were set out in the WHO Bulletin “Feeding children in the first year of life: physiological basis.” For more than 10 years, doctors around the world have been guided by these principles. Our mothers are sometimes not always familiar with these principles and find themselves captive to outdated ideas. What should a modern woman know about breastfeeding when her mother is ill?
First, let's try to identify different situations in which a nursing woman can get sick. This could be an exacerbation of a chronic disease that the woman has been suffering from for a long time, it could be an accident or injury, and finally, the woman could become infected with some kind of viral or bacterial infection.
Forewarned is forearmed
Let's first consider a case of exacerbation of a chronic disease.
It would not be amiss to remind you that such diseases do not fall from the sky, and a breastfeeding woman was probably faced with the need to do something about it already during pregnancy. It is pregnancy, or even better, the period before its onset, that should be used to develop behavioral tactics during exacerbation of attacks.
If the disease is serious, then first of all it can complicate the course of the pregnancy itself. With some diseases it becomes simply impossible. If a woman has found the opportunity to become pregnant, then she will be able to breastfeed with this disease. So, if you are sick with something, but are going to feed, remember the first rule
Chronic diseases do not interfere with lactation. Most known diseases are compatible with breastfeeding.
Only very severe conditions of the mother that threaten her life require stopping breastfeeding. And most often - for a while. I will quote the WHO bulletin on feeding children in the first year of life: “It is amazing how reliably lactation continues, despite the numerous problems associated with the mother’s health. Breastfeeding is contraindicated only in cases of severe maternal illness, for example in cases of heart failure or serious kidney, liver or lung disease..."
The question then arises, how to treat exacerbations or attacks? If a woman takes her health seriously, then certain treatment tactics have already been developed during pregnancy. Doctors helping a pregnant woman do not always expect her to breastfeed for a long time. Treatment is often delayed until after delivery, only to be resumed when the woman gives birth. You should discuss the possibility of treatment during lactation with your doctor in advance. Some of them expect that a woman will breastfeed for only a few months and do not take this into account. Explain to your doctor that you are going to breastfeed for a long time, at least 2 years, therefore treatment tactics throughout pregnancy and lactation should be gentle.
Thus, we can formulate a second rule for those who get sick while breastfeeding:
Most commonly used medications are safe for the baby and can be taken during breastfeeding, but it is better to choose the drug in advance to be sure.
Counting on a long term of gentle treatment, it would not be amiss to take advantage of the possibilities of physiotherapy, homeopathy, acupuncture, etc. In particular, the competent use of complex homeopathic medicines can prevent or significantly alleviate the course of attacks in many diseases. Even if the mother lives in a city where there is no homeopathic pharmacy, complex preparations can be ordered in the online store or by mail. And if you take care of this in advance, then by the time such a situation arises you will always have a safe and reliable drug at hand. Let's formulate the third rule:
Non-drug treatment methods and homeopathy should be used as widely as possible - this is much safer for both mother and child.
Trouble came suddenly
Indeed, no one is immune from the unexpected: accidents, injuries, the need for urgent surgery. Well, my mother didn’t know, she didn’t notice that her tooth was being destroyed or her appendicitis was getting worse! When caring for a child, it is sometimes difficult to notice that something is wrong with health.
Don't give up and tell your doctor right away that you are breastfeeding. Also ask how compatible the products he uses are with lactation and how long it takes for them to be removed from the body.
Most often, even with such a sudden misfortune, it is not necessary to wean the child from the breast. In extreme cases, he may miss feedings for several hours. If the mother was not prepared for this situation, then, of course, she may not have expressed milk to feed the baby in her absence. Allow your relatives to feed the child with formula milk several times and try to solve all your problems as soon as possible.
During mini operations, even after using general anesthesia, you can feed the child 6-12 hours after the end of the operation. After tooth extraction, mini-abortion, opening of ulcers and abscesses, you can feed after 6 hours. It is better to express the first portion of milk. For longer operations - after 12 hours. In this case, you should express about 3 times.
Consult your doctor in advance about post-operative antibiotic therapy and choose ones that are compatible with breastfeeding. There are such antibiotics and there are quite a lot of them (for example, penicillin antibiotics, many first and second generation cephalosporins , many macrolides ). Antibiotics that affect bone growth or hematopoiesis (for example, fluoroquinolone derivatives, chloramphenicol ) are strictly contraindicated during breastfeeding. Almost always you can find a suitable substitute for them. Let's formulate the following rule for such situations:
When using a medicine once, the mother is not sure is safe for the child, you should consult a doctor or pharmacist. If this is not possible, you can not feed for 12 hours; during this time, most of the medications are eliminated from the body.
Unfortunately, not all diseases can be cured by using the drug once or by performing a simple operation. There are situations when the mother requires urgent hospitalization, serious chemotherapy and, alas, this takes more than one day. Many mothers, having heard about this, try to immediately stop feeding, and after their return from the hospital, the child becomes a complete artificial child. However, there is no need to wean your baby forever. Here is what the WHO bulletin recommends in these cases: “If there is an urgent need for a medicine that is harmful to the breast-fed baby, feeding should be temporarily interrupted while lactation is maintained.” It is much easier to organize temporary weaning of a child from the breast than to permanently deprive him of the benefits that breast milk brings . For 2-3 weeks, the child is fed with formula, preferably using not a bottle with a nipple, but any other method - a spoon, a small cup, using a penicillin bottle or a plastic syringe without a needle. During temporary weaning, it is better for the mother not to take part in caring for the child, so as not to mislead him - he will not be able to understand why the mother, who is nearby, does not put him to the breast.
If the mother is really seriously ill, then to maintain lactation it will be enough for her to express her breasts 3-4 times a day , since milk production with serious ailments and lack of sucking is significantly reduced. In situations where the mother’s well-being does not suffer much, she needs to express more often, but 6 times a day is enough. It is not such a big sacrifice, for the sake of happiness, to put the child to your breast again after the end of treatment. After completion of therapy, the baby quickly returns to the breast and the volume of lactation is restored within 1-3 days. Therefore, the following rule for treatment during breastfeeding will look like this:
If it is necessary to use medications that are incompatible with breastfeeding, use temporary weaning of the child.
These ubiquitous infections
If it is impossible to infect a child with a toothache or an injured finger, then when it comes to an infectious disease, many are still confident that the mother will definitely infect the child and he should definitely be weaned. There is also an idea that such an infection can be prevented by putting a gauze bandage on the mother and giving the milk to the baby after preliminary boiling. For modern ideas about breastfeeding, such behavior seems simply ridiculous.
If the mother gets sick, then much earlier than any clinical signs of the disease begin to appear, the child already receives, with milk, the pathogen itself, specific antibodies to this pathogen, split fragments of the pathogen to produce its own antibodies to it, plus full-fledged immune protection against possible accompanying complications . When the mother or the doctors treating her discover that she has the disease, the child is either already sick or actively immunized. Exclusion of breastfeeding in this case leads to the deprivation of the child of the only unique medicine intended for him personally, which he receives with mother's milk. Boiling milk will destroy not only the pathogen, but also all the protective factors of the milk. And a gauze bandage worn after the disease is discovered will not protect against pathogens in milk.
It is not worth weaning either a child who is already sick or one who is still healthy. It is mother's milk that provides the child with the opportunity to be effectively immunized and avoid disease, despite the fact that he received pathogens every day. Weaning a healthy baby when the mother is ill exposes him to the risk of getting sick, while depriving him of effective immune protection. In clinical studies, using the example of influenza, measles, chickenpox, etc., it has been shown that a child who is without immune protection gets sick more often and recovers more slowly than a child who is not weaned.
Weaning an already sick child, as shown by studies of children infected with staphylococcus, streptococcus, mumps, influenza, etc., will deprive him of many antimicrobial factors of breast milk, and feeding substitutes will cause the growth of intestinal pathogens. Neither is desirable for a child already at risk. In addition, both mother and child should receive adequate treatment, which is easier to organize when the child receives the medicine directly through mother's milk.
In some cases, early infection of a child with microorganisms carried by the mother plays an important role in the formation of his immune defense. In particular, Staphyloccocus aureus (staphylococci) is found in mother's milk in most cases of postpartum mastitis. These are common microorganisms that live on the mother's skin and mouth. A few hours after birth, the mother gives them to the child, without any negative consequences for him, so if mastitis happens, they are no longer dangerous to the child. Detection of CMV (cytomegalovirus) in a nursing mother does not lead to illness in the child, but, on the contrary, serves as primary immunization against this viral disease.
Thus, the following rule can be formulated for breastfeeding mothers when an infection is detected:
There is no reason to wean a child from the breast if an infection is detected in the mother, regardless of what pathogen caused it. Moreover, weaning a child in this situation exposes him to the risk of contracting the same disease that his mother has.
How to treat a nursing mother for infection? Depending on the situation, which depends on the type of pathogen and the condition of the mother.
A high temperature can and should be reduced if the mother does not tolerate it well. It is worth remembering that high temperature is one of the body’s ways of protecting itself. To reduce the temperature, you can use any remedy found in the house once, however, if you need to repeat the drug, it is better to stick to paracetamol. Conventional remedies for runny nose, cough, sore throat, etc., so-called symptomatic remedies are safe for use during lactation.
For the treatment of viral infections
(colds, flu, etc.) in addition to antipyretic and symptomatic drugs, special
antiviral drugs based on interferon preparations can usually be used.
It is better for such drugs to be prescribed by a doctor, although some of them, for example “influenza ferron”, can be used independently. Most of them are also compatible with lactation. To treat a bacterial infection
(otitis, tonsillitis, pyelonephritis, mastitis, etc.)
antibiotics .
Using the same principles as described above, you can always choose antibiotics that are compatible with breastfeeding. If a nursing mother knows that by continuing to feed her baby even during illness, she can provide him with immune protection, this will not only help her continue feeding, but will also be a good incentive for a speedy recovery. Therefore, summing up the above, we can once again say to all nursing mothers - do not stop breastfeeding during illness! If doctors insist on this, consult several. Another source of information is lactation consultants; we have accumulated a huge amount of statistical material on breastfeeding in different situations.
Mayorskaya M.B., lactation consultant.
=============================================================================
Since not all doctors know about the possibility of combining therapy with breastfeeding, many nursing mothers unjustifiably wean their children from breastfeeding in order to undergo the course of treatment necessary for their health. Taking medications while breastfeeding Fortunately, many women are also now aware of all the benefits of breastfeeding and therefore refuse to strictly follow the advice of the attending physician, who only reads the instructions on the packaging of the drug, without bothering to search for special literature. They themselves look for information on the Internet or in special reference books and often it turns out that the prescribed drug is compatible with breastfeeding. Indeed, most medication inserts contain information about contraindications during lactation and pregnancy. However, if you open a specialized reference book, you will see that the “dangerous” drug is safe and does not have a harmful effect on the child, passing through breast milk. Why such discrepancies? The fact is that only the information that is confirmed by research from the pharmaceutical manufacturer itself is printed on the insert. If such studies have not been conducted on a specific group of people, then the manufacturer is obliged to write in its instructions that the drug is contraindicated or should be used with special precautions. This way they abdicate all responsibility in case of side effects and undesirable consequences. Studies on pregnant women are carried out very rarely, and on breastfeeding women even less often. But there are scientists who are engaged in researching and collecting information about the penetration of various chemical elements into breast milk, processing and publishing such facts in special reference books. The most famous of the reference books in English is called “Medications and mother's milk”, where on 1262 pages the effect of drugs on a child during pregnancy and lactation is described. A similar reference book also exists in Russian, only much more subtle. For example, the reference book by Karpov and Zaitsev “Risk of using medications during pregnancy and lactation.” On the Internet, the compatibility of drugs can be viewed on the website of the Spanish hospital www.e-lactancia.org. By
Types of anesthesia and contraindications
Pain relief during treatment and tooth extraction is performed using topical medications. Most often, dentists use Lidocaine. It is harmless for nursing women and babies (with the exception of allergic reactions), because:
- side effects are rare;
- acts locally and for a short time;
- does not affect the functioning of internal organs;
- passes into milk in small quantities;
- has a short half-life.
The use of anesthesia during breastfeeding is possible at any stage. It will not harm the baby if you remember a few points:
- treat teeth after the 1st trimester of pregnancy;
- warn your doctor in advance about breastfeeding;
- do not use local anesthesia containing adrenaline;
- feed your child well before visiting the doctor;
- express and pour out the milk produced after the application of anesthesia (the drug is eliminated from the body in about 5-6 hours).
One of the most common questions is whether it is possible to treat teeth during pregnancy.
Both dentists and gynecologists answer: “Yes.” Caries is an infectious process and, therefore, a direct threat to the unborn baby. In addition, according to a number of doctors, infection of carious teeth can increase gestosis of the second half.
The second point is that a pregnant woman’s immunity is physiologically reduced, so complications often arise in the form of pulpitis, inflammation and even suppuration in the root area of the tooth.
The ideal period for filling or removal is the second trimester (from 14 to 20 weeks). In the first trimester, the baby develops internal organs and the neural tube, from which the brain and spinal cord and peripheral nerves develop. Therefore, the use of drugs is undesirable, and in the third case, it is difficult for a woman to remain in one position in the dental chair for a long time.
Dental problems after childbirth
It should be noted that it is during the postpartum period that many women begin to notice that the condition of their teeth has worsened. There is such a popular expression “teeth flew”, which describes how quickly dental problems arise in young mothers. And this is along with the fact that severe hair loss also begins, and sometimes skin problems.
Dental problems after childbirth are common
Indeed, such unpleasant changes are not uncommon. During lactation, the female body is significantly depleted - reserves of calcium, various vitamins and minerals are spent first on carrying a child and then on feeding him. This is why dental pathologies arise – caries, gum disease.
Usually the problem is noticeable already during pregnancy. But for some irrational reasons, expectant mothers are in no hurry to treat their teeth, postponing this moment until later. Meanwhile, if pregnancy gingivitis, serious gum inflammation, and the risk of premature birth are not treated, the risk of premature birth increases significantly. Therefore, teeth and gums can be treated during pregnancy; the most favorable period is the second trimester.
The hypertrophied form of gingivitis affects all gums
It has been noted that untreated teeth during pregnancy, a predisposition to dental problems, bleeding gums - all this around the middle of lactation becomes an imminent threat of urgent treatment. And in order not to lead to the removal of teeth or the formation of large carious cavities, you need to go to the doctor, without fear of either the treatment itself or anesthesia.