General analysis
It is one of the basic tests required when visiting many specialists.
General analysis among specialists may also be referred to as “clinical”, or bear the abbreviation KLA. It is a whole set of tests aimed at determining both the quantity and parameters (size, etc.) of various blood cells.
The test allows blood sampling from both a vein and a finger (capillary).
Indications for use, preparation for the study
This is one of the most common laboratory tests performed to assess the general health of a patient. Prescribed for routine medical examinations, preparation for surgery, and included in the medical commission.
Symptoms for which a doctor may prescribe OAC: complaints of fatigue, weakness, apathy, signs of an infectious disease or inflammation, and elevated body temperature. A timely test allows you to diagnose and promptly treat a whole range of serious diseases.
The results of your analysis will be as reliable as possible if, before taking it, you:
- the day before your visit to the clinic, exclude alcohol and medications from your diet (in consultation with your doctor);
- You will not take it for 8 hours before the test (you can drink still water);
- Half an hour before donating blood, it is advisable not to overexert yourself physically and emotionally. Try not to smoke either.
General blood test indicators
The blood test includes a number of parameters. First of all, this is the calculation of the number of red blood cells (oxygen transport), leukocytes (ensure the fight against bacteria and viruses), platelets (blood clotting) per microliter or liter of blood. This also includes other indicators that describe the shape, volume and other characteristics of the cells being studied.
The basic table with blood sampling results includes:
- hemoglobin level
- hematocrit
- average red blood cell volume
- average hemoglobin content in an erythrocyte
- average hemoglobin concentration in erythrocytes
- platelets
- white blood cell count
- red blood cell count
In addition to basic indicators, the doctor may prescribe a leukocyte formula (the ratio of different forms of leukocytes as a percentage) and a calculation of the erythrocyte sedimentation rate (ESR). Professionals call such a comprehensive study a “clinical blood test.”
Blood chemistry
It is a laboratory test that allows you to diagnose the condition and performance of internal organs: liver, kidneys, pancreas, gall bladder, etc. The method also makes it possible to collect information about metabolism and identify the need for microelements.
Indications for prescription by a doctor
Our clinic’s specialists recommend undergoing blood biochemistry at least once a year, even for those people who have no health complaints. Thus, you can always detect problems in time and prevent the formation of chronic diseases. Biochemical analysis is prescribed by a doctor for infectious and somatic diseases.
Diagnosis of diseases based on deviations from the norm
The results of the study provided to the patient contain the established values of the studied indicators, as well as the acceptable norm (corridor of indicator values in a healthy person). When the set values leave this corridor, we can talk about the presence of problems with the patient’s health.
A biochemical blood test is the best way to timely diagnose a whole range of serious diseases. It is better to cope with the disease at an early stage, to prevent the disease from becoming chronic.
Potassium (K+, Potassium), Sodium (Na+, Sodium), Chlorine (Cl-, Chloride)
Interpretation of study results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc.
Potassium Units of measurement in the INVITRO laboratory: mmol/l.
Reference values
| Age | Potassium level, mmol/l |
| 1 day - 4.3 weeks | 3,7 — 5,6 |
| 4.3 weeks - 24 months | 4,1 — 5,3 |
| 24 months - 14 years | 3,4 — 4,7 |
| 14 years | 3,5 — 5,1 |
Increased potassium levels (hyperkalemia):
- excessive intake of potassium into the body: rapid infusion of potassium solutions;
- release of K+ from cells into the extracellular fluid: with massive hemolysis, rhabdomyolysis, tumor disintegration, severe tissue damage, deep burns, malignant hyperpyrexia, acidosis;
- decreased release of K+ by the kidneys: acute renal failure with oligo- and anuria, acidosis, end-stage chronic renal failure with oliguria, Addison's disease, pseudohypoaldosteronism, hypofunction of the renin-angiotensin-aldosterone system, shock conditions, tissue ischemia;
- decrease in the volume of extracellular fluid - dehydration;
- taking medications such as amiloride, spironolactone, triamterene, aminocaproic acid, antitumor agents, digoxin, non-steroidal anti-inflammatory drugs, trimethoprim-sulfamethoxazole.
Low potassium levels (hypokalemia):
- insufficient intake of potassium into the body: with chronic fasting, diet poor in potassium;
- loss of potassium by the body with intestinal secretions with frequent vomiting, profuse diarrhea, intestinal villous adenoma, intestinal fistulas, suction of stomach contents through a nasogastric tube;
- loss of potassium in the urine due to renal tubular acidosis, renal tubular failure, Fanconi syndrome, Conn's syndrome (primary aldosteronism), secondary aldosteronism, Cushing's syndrome, osmotic diuresis (diabetes mellitus), alkalosis, administration of ACTH, cortisone, aldosterone;
- redistribution of potassium in the body (increased entry of potassium into cells): during treatment with glucose and insulin, familial periodic paralysis, alkalosis;
- sweat loss in cystic fibrosis;
- treatment of megaloblastic anemia with vitamin B12 or folic acid;
- hypothermia;
- taking corticosteroids, diuretics (except potassium-sparing), beta-blockers, antibiotics;
- administering large amounts of low-potassium fluid;
- VIPoma (tumor of pancreatic islet cells that secretes vasoactive intestinal polypeptide - VIP);
- Magnesium deficiency.
Sodium
Units of measurement in the INVITRO laboratory: mmol/l.
Reference values
| Age | Sodium level, mmol/l |
| 1 day - 4.3 weeks | 133 — 146 |
| 4.3 weeks - 24 months | 139 — 146 |
| 24 months - 14 years | 138 — 145 |
| 14 – 90 years | 136 — 145 |
| 90 years old | 132 — 146 |
Increased sodium levels (hypernatremia):
- hypertensive dehydration: a) loss of fluid through the skin with severe sweating, b) loss of fluid through the lungs with prolonged shortness of breath; c) loss of fluid through the gastrointestinal tract with frequent vomiting and severe diarrhea; d) with high fever (typhoid fever, paratyphoid fever, typhus, etc.);
- insufficient intake of water into the body;
- sodium retention in the kidneys (reduced urinary excretion) with primary and secondary hyperaldosteronism, Cushing's syndrome (excess of corticosteroids);
- excessive administration of sodium salts, for example, hypertonic sodium chloride solution;
- taking medications such as ACTH, anabolic steroids, androgens, corticosteroids, estrogens, methyldopa, oral contraceptives, sodium bicarbate.
Low sodium levels (hyponatremia):
- insufficient sodium intake into the body;
- loss of sodium due to vomiting, diarrhea, severe sweating with adequate water and inadequate salt replacement;
- overdose of diuretics;
- adrenal insufficiency;
- acute renal failure (polyuric stage);
- osmotic diuresis;
- hypotonic overhydration: a) excessive parenteral fluid administration; b) reduced excretion of water in renal failure, increased secretion of vasopressin, deficiency of corticosteroids;
- dilution hyponatremia with edema and ascites in chronic heart failure, liver cirrhosis, liver cirrhosis, liver failure, nephrotic syndrome;
- taking medications such as furosemide, aminoglycosides, hypertonic glucose solution, non-steroidal anti-inflammatory drugs, amitriptyline, haloperidol;
- hypothyroidism
Chlorine
Units of measurement in the INVITRO laboratory: mmol/l.
| Age | Chlorine level, mmol/l |
| 1 day - 4.3 weeks | 98 — 113 |
| 4.3 weeks - 90 years | 98 — 107 |
| 90 – 120 years | 98 — 111 |
Increased chlorine levels (hyperchloremia):
- dehydration due to insufficient water intake4
- acute renal failure (when the consumption of chlorides exceeds their excretion during anuria, oliguria);
- diabetes insipidus;
- corticosteroid therapy;
- respiratory alkalosis;
- hyperfunction of the adrenal cortex.
Decreased chlorine levels (hypochloremia):
- increased sweating (with secretory dysfunctions and hormonal imbalance);
- overdose of diuretics;
- respiratory and metabolic acidosis;
- dehydration due to fluid loss due to vomiting, diarrhea;
- aldosteronism;
- polyuric stage of renal failure;
- head injuries;
- water intoxication with an increase in the volume of extracellular fluid;
- taking laxatives.
Blood clotting test
A coagulogram is a laboratory test of blood for clotting (coagulation). Screening combines the study of both indicators of coagulation and anticoagulation blood systems. In the medical environment, the following synonyms are also allowed: hemostasiogram, hemostasis analysis or blood clotting test.
Let's consider how the process of transformation of blood into a stopping clot occurs. When the wall of any vessel is damaged, special proteins are released, triggering a protective mechanism. During its process, the closest platelets change their shape, becoming rounded and becoming like balls covered with hook-like processes. With their help, the cells adhere and clog the damaged area. This achieves two important effects:
- due to an obstacle in the form of a clot, blood can no longer leave the vessel through the rupture;
- a blood clot prevents viruses, bacteria and other substances from entering the body from outside.
In the medical community, in addition to the described phenomena, it is customary to include the subsequent dissolution of the protective thrombus in the process of hemostasis.
Indications for the purpose of analysis, preparation for the study
Various factors can influence the effectiveness of blood clotting. There are a number of pathologies that affect blood clotting:
- malfunctions of the hematopoietic organs: liver, bone marrow
- side effect from the action of certain medications: antibiotics, aspirin, etc.;
- vitamin deficiency;
- immunity disorders
- hemophilia is a genetic disease that is transmitted through the male line.
Coagulation tests will help identify problems with the blood's ability to clot. The coagulogram (analysis result) includes the findings of several tests that can collectively record even the most minor disturbances in the process of hemostasis.
A clotting test can be prescribed after obtaining data from a general blood test - if the platelet count is outside the normal range (150-400 thousand cells per microliter). It is important to understand that a deviation can be a marker of both serious diseases (inflammatory processes, anemia, oncology, etc.) and completely harmless conditions (lack of vitamins or a consequence of serious physical activity). That is why we recommend contacting the appropriate specialists to prescribe additional examinations.
Blood plasma is subject to research. Blood is taken from a vein in the morning (a prerequisite is a preliminary fast of at least 8, maximum 14 hours).
If you take any medications on a regular basis, consult your doctor before the test to see if you need to stop taking any medications.
Indicators of blood tests for coagulation, diagnosis of diseases
A coagulogram reflects a complete picture of the body’s ability to independently fight bleeding. It includes a number of indicators that reveal various aspects of blood clotting. The cost of a coagulogram will depend on the tests included in it. You can view the price list here on the REAL MED company website, or by calling the contact numbers.
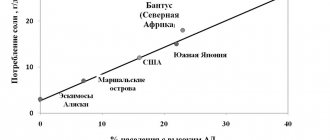
Study of the level of potassium, sodium, chlorides in the blood
Sodium, potassium and chlorine are the body's main electrolytes. Electrolytes are mineral compounds that are capable of conducting electrical charge. Being in tissues and blood in the form of salt solutions, they help move nutrients into cells and remove metabolic products from cells, maintain water balance and the required level of acidity in them. The main electrolytes in the human body are sodium (Na+), potassium (K+) and chlorine (Cl-).Sodium (Na+) is the main cation in the extracellular space. Sodium (Na+) is the most important osmotically active component of the extracellular space, which is associated with the regulation of the volume of extracellular fluid. 96% of the total sodium in the body is found outside cells. It is involved in the conduction of excitation in nerve and muscle cells, in the formation of an alkaline blood reserve and the transport of hydrogen ions. The concentration of sodium in plasma (serum) depends on the balance of the following processes: sodium intake, its distribution in the body and excretion by the kidneys and sweat glands. The main regulators of sodium metabolism in the body are the renin-angiotensin-aldosterone system, ADH (vasopressin), and atrial natriuretic hormone.
Potassium (K+) is the main cation in intracellular fluid, but a small but vital amount is found in plasma, the liquid part of the blood. Potassium (K+) is involved in the creation and maintenance of the electrical membrane potential of cells. Regulates intracellular osmotic pressure, stimulates the activity of glycolytic enzymes, participates in the metabolism of proteins and glycogen, plays an important role in the formation of the action potential in nerve and muscle cells and the conduction of nerve impulses, and has immunomodulatory activity. Monitoring potassium levels is very important. Even minor changes can affect the heart rate and the heart's ability to contract. The concentration of potassium in plasma (serum) depends on the balance of the following processes: potassium intake from the outside, distribution in the body and excretion (by the kidneys, sweat glands, through the intestines, etc.). There is no potassium depot in the body. Therefore, even with small changes in the concentration of potassium inside cells, its concentration in the plasma changes significantly. Changes in blood pH lead to changes in the K+ content in cells: during acidosis, it leaves the cells into the plasma; during alkalosis, it enters the cells. With hyperkalemia, ventricular tachycardia, ventricular fibrillation and even asystole are observed. With hypokalemia, muscle weakness, decreased reflexes, hypotension, disturbances in the conduction system of the heart, intestinal obstruction, and polyuria develop.
Chlorine (Cl-) is the main anion of extracellular fluid and gastric juice. Chlorides migrate through the membrane either inside or outside the cell and thereby maintain its electrical neutrality. Chloride levels usually correspond to sodium levels. Chlorine ions play an important role in maintaining the acid-base state, osmotic pressure and water balance in the body. In biological media it is found predominantly in the state of the chloride anion Cl-. Contained in plasma, lymph, cerebrospinal fluid. The balance of chlorine ions in the body is carried out by the presence of a balance between the processes of chlorine intake from food, distribution in the body and its excretion in urine, sweat and feces. A change in the concentration of sodium ions leads to a change in the concentration of the chloride anion. With the loss of chlorides, alkalosis develops; with excess consumption, acidosis develops.
Sodium, potassium and chlorides enter the body with food, while the kidneys are involved in removing them from the body. The balance of these chemical elements is an important indicator of human health, particularly how the kidneys and heart function. Measuring the levels of sodium, potassium and chloride together allows you to determine the anion “window” - the difference in the content of anions and cations in the blood. Its abnormal value is not a specific indicator, but suggests the presence of toxic substances in the body (oxalates, glycolates, aspirin) or the likelihood of metabolic abnormalities caused by fasting or diabetes. Because electrolyte and acid-base imbalances are associated with a wide range of acute and chronic diseases, electrolyte testing can be ordered for both hospitalized patients and those newly presenting to emergency departments.
What is the research used for?
- As part of a general medical examination or as a stand-alone test for metabolite testing.
— For screening electrolytes and studying acid-base imbalance.
— To monitor the effectiveness of treatment of imbalances affecting the functioning of certain organs.
When is the study scheduled?
— When diagnosing a disease with symptoms such as swelling, nausea, weakness, clouding of consciousness, cardiac arrhythmia.
— When examining patients suffering from acute and chronic diseases.
— If necessary, monitor the effectiveness of treatment of hypertension, heart failure, liver and kidney diseases.
- If the level of one of the electrolytes, such as sodium or potassium, is low, a repeat test is subsequently prescribed to monitor the dynamics of the imbalance until the normal level of this electrolyte is restored.
Indications for use:
Potassium
— Study of kidney function in their pathology.
— Cardiovascular pathology.
- Cardiac arrhythmias, arterial hypertension.
- Adrenal insufficiency.
— Monitoring the potassium content in the blood when prescribing diuretics and cardiac glycosides.
Sodium
— Gastrointestinal disorders: vomiting, diarrhea.
- Adrenal insufficiency.
- Kidney diseases.
- Dehydration, increased fluid loss.
Chlorine
— Monitoring and dynamic observation of acid-base disorders in various diseases.
- Kidney diseases.
- Diabetes insipidus.
— Pathology of the adrenal glands.
Analysis for tumor markers
Today, comprehensive cancer screening is not possible without laboratory tests, in particular, blood tests for tumor markers. Regular testing allows you to detect a serious disease at an early stage.
Indications for passing
The test is prescribed by a doctor both during a course of treatment to assess its effectiveness and to prevent relapses.
If you conduct an examination yourself, without a doctor’s prescription, its results should be provided to specialists for correct interpretation!
Analysis results
It is important to understand that diagnosing cancer cannot be based solely on the results of laboratory blood tests, since benign neoplasms and inflammatory processes can also provoke an increase in the level of tumor markers.
Only a comprehensive study under the supervision of experienced doctors will help you reliably identify a malignant tumor at an early stage.
Our clinic specialists will provide you with a sufficient set of examinations to monitor your health.