general characteristics
The main cation of the extracellular space. Sodium maintains osmotic pressure and pH inside the cell and in the extracellular space, affects the processes of nervous activity, the state of the muscular and cardiovascular systems. The concentration of sodium in plasma (serum) depends on the balance of the following processes: sodium intake, its distribution in the body and excretion by the kidneys and sweat glands. The main regulators of sodium metabolism in the body are the renin-angiotensin-aldosterone system, ADH (vasopressin), and atrial natriuretic hormone.
People have long had a difficult relationship with salt. The most popular seasoning all over the world is not just that, but also vitally necessary for humans. According to L. Dahl, perhaps salt is the most important nutritional factor affecting the control of blood pressure (BP) [1]. Moreover, the consumption of table salt is such an important component of nutrition that eliminating salt from the diet can lead to an irreversible catastrophe, namely death. After all, without salt, or rather without sodium chloride (NaCl), our body simply would not be able to perform its functions normally. It is sodium, which is mainly found in salt, that will be discussed. For your information, 100 g of salt contains 38.183 mg of sodium.
The main physiological functions of sodium are as follows:
— ensures the penetration of amino acids and carbohydrates into cells;
— stimulates the activity of digestive enzymes;
- participates in the passage of impulses along the nerve fiber along with potassium;
- accumulates fluid in the body.
The most important property of sodium from a physiological point of view is its ability to bind water. Thus, 1 g of salt is able to retain up to 100 ml of water in the body. When tissues and blood vessels are oversaturated with salt, an excess of water occurs in the body, which leads to an overload of the activity of all organs involved in a particular process. For example, the heart is forced to work harder, and the kidneys are forced to remove excess amounts of both water and salt from the body.
Currently, in many countries, salt intake ranges from 9 to 15 g per day [2]. Women consume slightly less salt than men. In our country, according to data collected in Moscow, they consume an average of 12 g of salt per day [3]. However, this amount of salt, according to modern researchers, is excessively high and harmful to health, since the human body needs and only needs 2-3 g of sodium per day, and in the case of increased sweating and significant loss of water - a little more. For a healthy person, 5-7 g of table salt per day does not pose any risk. However, continually exceeding this limit has consequences. For those suffering from arterial hypertension (AH) or prone to this disease, salt can be harmful. Why did salt receive such an unattractive status?
Salt intake and hypertension
Although salt is highly regarded by many people as a versatile seasoning, its intake has long been associated with elevated blood pressure and, more recently, with other health indicators [1–3].
Mechanisms linking salt intake and increased blood pressure include increased extracellular volume and peripheral vascular resistance due in part to increased sympathetic nervous system activity.
The results of epidemiological studies show that the development of hypertension is associated with salt consumption, there is a close relationship between sodium intake and the incidence of hypertension, and in addition, limiting sodium intake contributes to a significant reduction in blood pressure [4]. The authors of a meta-analysis of several randomized trials lasting from 1 month showed that a moderate reduction in salt intake caused a significant decrease in blood pressure in both individuals with and without hypertension: a reduction in salt to 6 g per day led to a decrease in blood pressure by 7/4 mmHg. in hypertensive patients and by 4/2 mm Hg. in normotensive patients [5]. One well-controlled, double-blind, crossover study examined three levels of salt intake in 20 participants with untreated hypertension in whom salt was reduced from 11.2 to 6.4 and 2.9 g per day. Before the study, blood pressure was 163/100 mmHg, salt intake was 11.2 g/day; when salt intake was reduced to 6.4 g/day, blood pressure decreased by 8/5 mmHg. and reached 155/95 mm Hg. With a further reduction to 2.9 g/day, blood pressure decreased by 8/4 mmHg. - up to 147/91 mm Hg. 19 out of 20 participants were observed for 1 year, their blood pressure did not exceed 145/90 mm Hg. at the lowest salt intake (up to 3 g/day).
According to H. Blackburn, who devoted his population-based work to the study of hypertension: “...a decrease in blood pressure among the population by 1-3 mm Hg. will have the same effect as all antihypertensive drugs taken together that are currently prescribed to patients with hypertension” [6]. And according to S. McMahon, expressed on the basis of an analysis of the results of numerous population studies, “...a decrease in diastolic blood pressure by 2 mm Hg. reduces the risk of death from stroke by 13%, and by 6 mm Hg. - by as much as 43%" [7].
The relationship between salt intake and hypertension has changed several times. The idea of the dangers of excess salt consumption was expressed in ancient Egypt. And in 1948, W. Kempner hypothesized that excess salt can increase blood pressure and proposed a rice-fruit-sugar diet with a limited amount of salt (less than 0.5 g per day) [8]. This diet helped reduce blood pressure in 64% of patients with hypertension and normalize blood pressure in 25% of patients with heart failure. More recent work proves that the main reason for the decrease in blood pressure when following the Kempner diet was precisely the sharp restriction of salt intake [9].
In 2007, the normal daily sodium intake for humans was determined to be from 2.6 to 4.8 g per day [10]. These figures, according to the study's authors, have remained unchanged in 45 countries for 50 years.
Salt consumption peaked in the 1870s, and after the invention of the refrigerator and freezers, the importance of salt as a preservative declined, but recently there has been a resurgence in salt consumption with more salty or processed foods [2].
However, not all people with regular high salt intake develop A.G. The whole point, as it turned out, is individual “sensitivity” to salt. The concept of salt sensitivity was originally proposed in the late 1970s, but the phenomenon is the subject of modern research that supports this theory. Some people may have increased sensitivity to salt, and when they consume it in excess, they develop hypertension. In others who are not sensitive, blood pressure remains normal even when consuming foods high in sodium. Salt sensitivity, as the author further notes, is a common biological phenomenon in human society. Depending on the method of determination and measurement, increased sensitivity to salt was noted in 25-50% of people with normal blood pressure and in 40-75% of patients with hypertension [11].
Active study of salt intake and its relationship with health began in the 1960s, when L. Dahl published the results of cross-population studies in the form of a now well-known graph (Fig. 1),
Rice. 1. Linear relationship between salt intake and blood pressure in different populations. which represents the entire spectrum of salt consumption around the world. The graph shows the influence or direct dependence of the spread of elevated blood pressure on the amount of salt consumed, which makes an important contribution to the salt hypothesis of increased blood pressure. The presented data leave no doubt that high blood pressure does not occur or is extremely rare in those regions where the population consumes small amounts of sodium throughout their lives (for example, Eskimos), and is often observed in areas where they consume a lot of salt (more than 20 g/day), as, for example, in the North of Japan, where elevated blood pressure is observed in 40% of the population. Differences in the prevalence of hypertension in countries or regions with high salt consumption were proven in more recent studies, which confirmed the assumption that it is the sodium content in food that is the main factor determining the incidence of hypertension in the population. It is possible, as the authors of more recent studies note, that other factors, such as obesity, race, constitutional characteristics, and dietary patterns, also affect blood pressure levels, as well as the amount of sodium consumed [12]. The results of a prospective 3-year study conducted in Russia showed that when salt intake was reduced from an average of 12 to 6 g per day, a statistically significant decrease in blood pressure in women with high normal blood pressure over 3 years was 3.27 mmHg. for systolic blood pressure (SBP) and 2.09 mm Hg. for diastolic blood pressure (DBP) [3]. In men, a more modest decrease in blood pressure was noted: SBP decreased by 1.92 mm Hg, and DBP by 1.91 mm Hg. With an increase in salt intake, blood pressure, on the contrary, increases. The Intersalt study estimated that salt intake greater than 6 g/day over 30 years would increase SBP by 9 mmHg. [13].
How much salt does the body need?
In the Stone Age, people consumed a minimal amount of salt; their diet consisted of natural, fresh foods. Currently, in North America there are surviving tribes of Indians leading a primitive way of life. Their daily sodium intake turned out to be 20 times less than that of people living in developed countries and eating mainly processed, refined foods. It is noteworthy that the blood pressure in Indians averaged 96/60 mmHg. and did not increase with age, which is not typical for modern civilizations.
The results of epidemiological studies around the world show that the optimal daily requirement for salt is 6-7 g, the so-called. approximately half of the amount consumed in modern society [13].
It is extremely difficult to accurately estimate the amount of sodium consumed daily, since even 24-hour urinary sodium excretion (the method considered the gold standard for determining daily salt intake) varies widely among individuals. M. Alderman [14] believes that there is no evidence that reducing salt intake to 3.5 g per day will improve health outcomes. And in 2013, the Institute of Medicine recognized sodium intake of up to 1.5 g per day as adequate [15].
The mechanism by which blood pressure increases with excess sodium intake remains unclear. It has been shown that in hypertension the flow of sodium and potassium through the erythrocyte membrane is disrupted. Due to disturbances of the potassium-sodium pump in hypertension, the sodium content in the intercellular space of smooth muscle tissue increases. This leads to increased excitability of the latter, which can cause an increase in blood pressure [16].
In the introduction to their work, L. Dahl et al. [1] state that salt is harmful and that the need for salt is less than the actual consumption. It's right. Most people eat more salt than necessary.
How to reduce salt intake?
For several million years, the ancestors of modern humans, like all mammals, ate foods low in salt. In table 1 presented
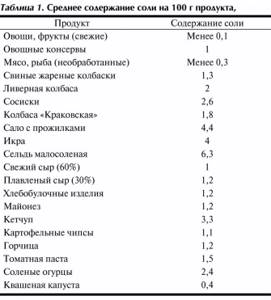
Table 1. Average salt content per 100 g of product, salt content in basic foods. From the data in table. 1 shows that the least amount of salt (and therefore sodium) is found in fresh vegetables and fruits.
In 2003, WHO recommended limiting salt intake in adults to 5 g per day (or 2 g sodium per day) [17]. Since then, these figures have been repeated in all the recommendations that we use to this day, including for the prevention of cardiovascular diseases [18].
Patients with hypertension are advised to sharply limit salt intake. This is achieved by following several rules proposed in 2000 and thanks to which you can reduce your daily salt intake by almost 2 times [14]:
- reduce the addition of salt when cooking by 50%,
- replace canned food with natural products,
- do not add salt to food while eating,
- reduce consumption of pickles,
- use unsalted seasonings,
- Avoid taking antacids due to the sodium they contain.
It seems so easy to reduce your salt intake by following these simple rules, but our contemporaries continue to eat more salt than is recommended by the medical community.
Why do we eat a lot of salt?
Although WHO recommended reducing salt intake for all adults back in 2003, actually reducing salt intake is difficult to achieve. Here's why: Due to sodium deficiency over a long period, from the Stone Age to the present day, people have developed a powerful salt appetite. This innate desire for salty foods makes it difficult in practice to reduce salt in the diet. However, when salt consumption is reduced (particularly in older people), due to a sharp change in taste habits, a person may lose his appetite altogether.
Humanity uses salt as needed to preserve food to avoid food poisoning, as salt is known to be a natural, effective and safe preservative. The fact is that 80% of salt consumed (Fig. 2)
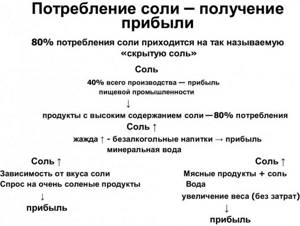
Rice. 2. “Hidden salt” in food. Adapted from F. He and G. MacGregor, 2009 accounts for the so-called “hidden” salt that is found in all industrially processed foods where salt is added for longer storage. The review authors blame manufacturers for adding too much salt to make a profit [19]. When salt is added to meat products, their weight increases, since salt is capable of retaining water, and as a result, manufacturers make a profit without special costs. It is estimated that the mass of a product can be increased by 20% completely free of charge using salt and water. The amount of salt in industrially processed foods is mainly due to the fact that it makes cheap, unpretentious food edible at no cost. Heavily salted foods are in high demand due to the salty taste habit - and this also increases the profits of producers. With the constant consumption of salty food, thirst arises, which contributes to the consumption of soft drinks and mineral water, which also cause thirst, i.e., a vicious circle arises for buyers and increased profits for producers. Food manufacturers attribute the addition of too much salt to consumer preference and report that if the salt content is reduced, consumers will avoid purchasing. However, this does not take into account a very important factor: only 1-2 months pass from a change in the sensitivity of taste buds in the oral cavity to a decrease in salt concentration [20]. This means that a lower concentration of salt will still be perceived as salty. There is evidence that if salt intake is reduced, people will prefer foods with less salt and may be able to avoid the highly salty foods they previously ate [21]. In the experience of UK consumers, reducing the salt in a particular brand's staple products did not reduce sales and there were no complaints from customers regarding taste. Therefore, it is unlikely that reducing the salt concentration in food products will lead to abstinence from purchases. But salt is a major contributor to thirst, and any reduction in salt intake will reduce fluid intake with a consequent reduction in sales of soft drinks and mineral water, and some of the world's largest salty snack companies are part of soft drink companies.
Less is better?
Do I still need to reduce my salt intake? The main focus of the study of salt intake has been on its beneficial effects on blood pressure. Currently, there is growing evidence of another, negative effect of reducing salt on health, which is in no way related to blood pressure. By 2013, the results of studies on the impact of salt reduction on health indicators and the idea of an additional reduction of salt in the diet of all adults, including those who do not suffer from or are at risk of developing hypertension, were published. In the same year, a special committee of the Institute of Medicine, after analyzing the research results, published a report in which it expressed its opinion on this matter [15].
1. There is no evidence of an effect of modest reductions in blood pressure with reduced salt intake on cardiovascular morbidity and mortality.
2. The benefits of reducing salt for the entire population have not been proven.
3. There is a safe range (just a range, not a 5 g point) for salt intake.
4. The benefits or harms of sodium intake less than 2300 mg/day (5 g salt) have not been established, but there are concerns about sodium intake below 1.5 g/day (3 g salt).
Before changing recommendations to an even lower salt intake due to proven effective lowering of blood pressure, it is necessary to understand that a person may suffer not only from increased blood pressure, but also from other diseases, metabolic disorders, or, finally, just be healthy [7]. Thus, in a study involving patients with heart failure (HF), a deterioration in the course of the disease was noted in the group with salt restriction to 1-1.7 g per day: re-hospitalization was more often required and an increase in mortality was observed within 6 months from the start of the study compared with group consuming 2-4.7 g per day. Therapy S.N. was the same in both groups. A deterioration in the course of diabetes mellitus types 1 and 2 was also noted [22]. A recently published review demonstrated a decrease in blood pressure by 1% in normotensive patients and by 3.5% in patients with hypertension, while at the same time a significant increase in plasma hormones (Table 2):

Table 2. Increase in hormone levels with decreased salt intake (adapted from N. Graudal et al., 2012) Note. Here and in the table. 4: *p<0.05 – statistically significant values. renin, aldosterone, adrenaline, norepinephrine. The demonstrated increase in adrenaline and norepinephrine is statistically insignificant, since, as can be seen from the data in table. 2, there was an insufficient number of participants and the studies themselves. From the data in table. 3 is visible
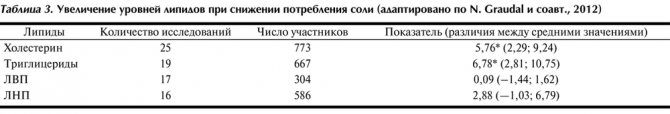
p
< 0.05), and high-density lipoproteins (HDL) and low (LDL) - statistically unreliable for the same reason (insufficient participants and studies to detect statistical significance) [23]. Moreover, as noted by F. He et al. [5], the adverse effects on lipids, especially triglyceride levels, are not simply an acute effect on salt reduction, as previously thought, but are persistent and long-term.
How does the ancient health science of Ayurveda evaluate salt? The salty taste will help drive away melancholy and allow you to feel the joy of life, no matter what it is.
In this regard, we can note a study on the effect of salt reduction on psychological status. In 2015, Japanese scientists published the results of a study in which 1,014 adult men reduced their salt intake from 10.8 g per day (4.3 g sodium) to 7 g salt, or 2.8 g sodium, per day, which caused development of depression [24].
Reducing dietary salt intake leads to a decrease in blood pressure, but the possibility of a negative effect of low salt intake on health cannot be ignored, excluding A.G. To recommend salt restriction for all healthy adults below 3 g of sodium (i.e., less than 6 g of salt or less than 1 teaspoon) requires a comprehensive weighing of the benefits and risks of this measure, which requires studies involving large populations. Although there are doubts about the benefits of reducing salt intake for all people, reducing salt intake is now an adjunct to drug treatment of hypertension and contributes to improved BP control, which reduces the need for medications. In table 4 indicated
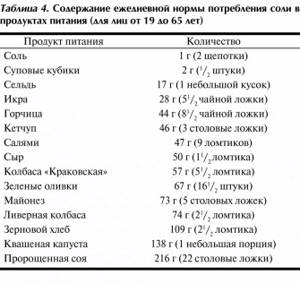
Table 4. Contents of daily salt intake in food products (for persons from 19 to 65 years old) a list of products that cover the daily salt requirement.
It is necessary to consider the impact of reducing salt in the diet (in addition to lowering blood pressure) on other health indicators. So, in Fig. 3 shown
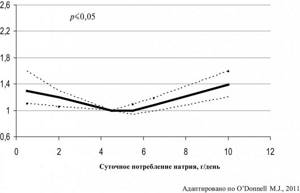
3. Salt intake and mortality from stroke, heart attack and hospitalization for HF. U
-shaped curve that shows that both high and low salt intake increases cardiovascular disease (CVD) mortality rates, stroke, myocardial infarction, and hospitalizations for congestive heart failure.
Results from several (but not all) observational studies have shown an increase in mortality not only at “higher levels” but also at levels below 2300 mg, indicating a U
-shaped relationship between sodium intake and mortality [25].
Randomized studies, carefully selected for statistical analysis, have shown the effect of sodium reduction on blood pressure not only in patients with hypertension, but also in healthy people with normal blood pressure (about 1 mm Hg) [25]. The immediate question is whether this effect is beneficial for the population as a whole in terms of morbidity, CVD prevention and mortality, and whether it is possible that these unproven assumptions about the benefits of salt restriction should lead to recommendations for reducing sodium intake in the entire population. The answer to this question can be found in the Institute of Medicine report cited above, one of the main points of which is to warn against further reduction of salt, i.e. below 3 g or below 1.5 g of sodium. The authors of several reviews are sincerely disappointed that the negative consequences of reducing salt intake in healthy people for the prevention of CVD, more precisely the deterioration of lipid and hormonal profiles, were ignored, and that recommendations for reducing salt in the diet remained the same [25–28]. To address the issue of reducing salt intake below 5 g per day, it would be advisable to conduct a large-scale, long-term, randomized clinical trial to determine whether such restrictions provide health benefits or not, and how this restriction affects survival and quality of life. Until the results of such a study are received, it is premature to talk about further reduction of salt in the diet. Many doubt whether it is even worth talking about reducing salt in the diet if the results of lowering blood pressure are so modest [9].
In most countries, more than ½ salt comes from industrially processed foods, including processed foods and sauces. In this regard, gradual, sustainable reduction of salt in processed foods is one of the easiest dietary changes to implement, as it does not require consumers to change their diet and still allows them to achieve the recommended 5 g per day [20].
In z
In conclusion, it should be noted that dietary recommendations for reducing salt must reflect the full variety of health consequences of this measure, including the impact on quality and life expectancy, and since we do not yet have such knowledge, no dietary recommendations can be scientifically justified [26 ]. There is no common point of view on additional reduction of salt in the diet of the population. Discussions are ongoing; the issue of reducing salt intake in order to prevent CVD for the entire population, including healthy people, has not yet been reached.
The authors declare no conflict of interest.
Author contributions:
Concept – O.M.
Collection and analysis of material - O.M., A.B.
Editing - O.M., A.B., E.P.
Interference:
- ACTH, anabolic steroids, androgens, carbenicillin, carbenoxalone, clonidine, corticosteroids, diazoxide, enoxolone, estrogens, guanethidine analogues, lactulose, mycorice, methoxyflurane, methyldopa, oral contraceptives, oxyphenbutazone, phenylbutazone, reserpine, sodium bicarbonate.
- Aminoglutethimide, aminoglycosides, ammonium chloride, amphotericin B, ACE inhibitors, captopril, carbamazepine, carboplatin, chlorpropamide, cholestyramine, cisplatin, clofibrate, cyclophosphamide, desmopressin, diuretics, fluoxetine, hypertonic glucose solution, haloperidol, heparin, indomethacin, ketoc onazole, lithium, lorcainide , miconazole, non-steroidal anti-inflammatory drugs, oxytocin, phenothiazines, thienylic acid, tolbutamide, tricyclic antidepressants, vasopressin, vinblastine, vincristine.
Clinical symptoms
Most patients with hyponatremia are asymptomatic. Symptoms usually appear when the plasma sodium level drops to below 120 mmol/l, and are often non-specific (for example, headache, diarrhea, boredom). In some cases, neurological and bowel symptoms dominate. In the world, the level of sodium in the world is growing, and the risk of guilt by the court of Tajikistan is growing. The onset of symptoms may also occur due to a rapid decrease in plasma sodium concentration. In case of low electrolyte levels, symptoms may appear at plasma sodium concentrations greater than 120 mmol/l. Before unfavorable prognostic factors for the development of hyponatremia in hospitalized patients, there may be the presence of similar symptoms, sepsis and respiratory failure.
Interpretation:
- Profuse sweating, prolonged hyperpnea, vomiting, diarrhea, diabetes insipidus, diabetic acidosis, hyperaldosteronism, Cushing's syndrome, dehydration, salt overload of the body.
- Salt-free diet, results of vomiting, diarrhea, excessive sweating with adequate water and inadequate salt replacement, diuretic abuse, polycystic disease and kidney medulla cysts, chronic pyelonephritis, renal tubular acidosis, osmotic diuresis, metabolic acidosis, primary and secondary adrenal insufficiency; congenital adrenal hyperplasia with 21-hydroxylase deficiency, isolated hypoaldosteronism, pseudohypoaldosteronism, edema, ascites, hypothyroidism; hyperosmolarity; SIADH, which may be associated with lung cancer, pancreatic cancer, central nervous system diseases, lung infections, acute intermittent porphyria, psychogenic polydipsia, false hyponatremia with extremely significant hypertriglyceridemia or hyperproteinemia; hyperglycemia.
Sample result (PDF)
Why does sodium deficiency occur?
When listing the factors leading to an increased need for sodium (see the section a few paragraphs above), almost all the causes of its deficiency were mentioned. In addition, a lack of a mineral and the need to use sodium may arise in a situation where there is not enough of this element in a person’s diet. This is rare, but it does happen. More often, a low sodium level occurs in people who are on a salt-free diet and at the same time subject themselves to significant stress, which is accompanied by intense sweating and loss of sodium.
Sometimes sodium deficiency is an “occupational disease.” For example, workers in hot shops who are exposed to elevated temperatures for several hours a day, drink a lot and sweat a lot can suffer from this metabolic disorder.
Stagnation of medications
Table 1 lists medications and drugs that cause hyponatremia. Hyponatremia is most often caused by diuretics and selective inhibitors of serotonin secretion. Most of these drugs are associated with SIADH, which results from normovolemic hyponatremia. Diuretics cause hypovolemic hyponatremia. Fortunately, in most seizures, after discontinuation of the drug, spontaneous correction of the electrolyte balance occurs.
Table 1. Medicines that cause hyponatremia
|
Syndrome of inappropriate secretion of antidiuretic hormone (SIADH)
SIADH is an important etiological cause of hyponatremia, and it is at fault when the antidiuretic hormone is not present in the body's needs when removing water. Because the antidiuretic hormone causes a decrease in fluid volume, hyponatremia results from increased water retention when sodium loss is evident. The diagnostic criteria for SIADH are presented in Table 2.
Table 2. Diagnostic criteria for SIADH (after J. Foster, 2001)
|
SIADH is a diagnosis of exclusion, which should be suspected if, in hyponatremia, low osmolarity of blood plasma is combined with disproportionately high osmolarity of the section, although it remains not obligatory to rediscover normal boundaries. Another characteristic sign is the presence of hypouricemia due to increased fractional excretion of urates. The most common etiological factors of SIADH are listed in Table 3.
Table 3. The most common etiological officials of SNADH
|
Any damage to the brain - from swelling to infection - can cause SIADH. Common common causes of SIADH are pneumonia (zocrema, legionnaires' disease) and empyema. Among other types of cancer, we can name bronchogenic carcinoma and granular cell carcinoma, which is also the most common source of ectopic secretion of antidiuretic hormone. Quite often, SIADH and mental disorders occur. More rare causes include acute intermittent porphyria, multiple sclerosis and Guien-Barré syndrome.
Value of blood plasma osmolarity
Normal level of plasma osmolarity (280–300 mmol/kg)
Increased hyponatremia and normal blood plasma osmolarity are compromised by pseudohyponatremia or TUR syndrome. Pseudohyponatremia is caused by the accumulation of large molecules, such as proteins and fats, in relation to sodium. These molecules do not change the osmolarity of the blood plasma, because if the aqueous sodium concentration is reduced, the protogal osmolarity does not change. In patients with pseudohyponatremia, important stages of hypertriglyceridemia and hyperproteinemia occur. Such diseases are, of course, normovolemic.
TUR syndrome (syndrome after transurethral resection of the prostate) is caused by the absorption of a large volume of hypotonic fluid during the hour of surgery and is characterized by hyponatremia with neurological and cardiac problems respiratory disorders.
Increased osmolarity of blood plasma (>300 mmol/kg)
Plasma osmolarity is increased in patients with hyponatremia and is reduced in cases of severe hyperglycemia, for example, in diabetic ketoacidosis or hyperglycemic hyperosmolar state. The presence of glucose molecules, which can have an osmotic effect and promote the movement of water from cells into the blood plasma, causes hemodilution. In the blood, osmotic diuresis, excess glucose, leads to hypovolemia. Hyperglycemia can be easily diagnosed by taking a blood sample from the patient's bed.
Reduced osmolarity of blood plasma (<280 mmol/kg)
Patients with reduced plasma osmolarity may be hypo- or normovolemic. For further differential diagnostics, measure the level of sodium in the sample.
Increase in sodium level in the section (>30 mmol/l)
The high concentration of sodium in the section indicates the excessive loss of sodium through the skin. In these patients, the main causes of hyponatremia include illness, deficient endocrinopathies, low threshold syndrome for osmotic pressure [2], syndrome of inappropriate secretion of antidiuretic hormone (SIADH), etc. Both drugs and drugs.
Diseases that cause hyponatremia include sodium-wasting nephropathy following chronic diseases (eg, polycystic disease, chronic pyelonephritis) and hyponatremia. hypertensive syndrome, which is often observed in patients with ischemic artery (for example, stenosis or occlusion of the artery). The combination of hypertension with hypokalemia (neural artery stenosis) or hyperkalemia (neural artery deficiency) helps to diagnose the etiology of this syndrome.
Endocrine illnesses rarely cause hyponatremia. It is necessary to remember about such “common” illnesses with minimal clinical signs, such as hypothyroidism and mineralocorticosteroid deficiency (for example, Adison’s disease), which can cause hyponatria Iyu. In any case, the level of thyrotropic, adrenocorticotropic hormone and cortisol is due, parts of hypothyroidism and hypoadrenalism can be attributed to polyendocrine deficiency syndrome (for example, Schmidt's syndrome). Treatment for Schmidt's syndrome includes replacement therapy with steroids before administration of thyroxine in order to prevent the development of Assonian crisis.
The syndrome of reduced threshold for osmotic pressure occurs when the threshold for secretion of antidiuretic hormone decreases. In such patients, after a test with oral hydration with water, normal excretion of water and intact tissue are revealed before dilution. This syndrome results in chronic, or stable, hyponatremia. It is used in cases of vomiting, tetraplegia, serious illnesses, poor nutrition or any chronic debilitating illnesses.
Reduced sodium level in the mixture (less than 30 mmol/l)
Patients with excessive sodium loss (with important care or loss through the ShKK due to vomiting and diarrhea) have a low concentration of sodium in the body, and parts of the body are encouraged to conserve sodium. Acute overindulgence in water, which can be clearly identified from the anamnesis, is eliminated after fluid hydration by hypotonic disorders and in psychiatric patients with psychogenic supernatural experiences in the country.
Unaslіdok Lіkuvannya by the concentrates of the course in the Sechi can be botied to be a native, in an hour of the remaining introduction to the drug, in reality of Suputniyu gypokalіmіy, the diuretiki in a history of the anamnesis.